
As most sports enthusiasts know, Aaron Rodgers, former Green Bay Packer quarterback and recent New York Jets QB (for just over a minute and half) suffered a season ending injury when he tore his Achilles tendon in the first game of the 2023/24 NFL season. Since then, I have been answering many questions from patients and sports fans about the nature of the Achilles Tendon rupture injury, recovery, and how to prevent it.
As the days continue to get shorter and temperatures begin a slow steady decline, athletes and exercise enthusiasts will work harder to warm-up and exercise during the winter months. A little caution and preparation are in order to avoid muscle/tendon strain, or worse yet, muscle/tendon tears, especially Achilles Tendon rupture. The Achilles tendon is one of the more common tendons torn.
This is the second of two columns on Achilles tendon rupture. Last week, I discussed the definition, sign and symptoms of the problem. This week will present examination, treatment and outcomes.
A thorough history and physical exam is the first and best method to assess the extent of the injury and determine accurate diagnosis. While a complete tear is relatively easy to determine, a partial or incomplete tear is less clear. Ultrasound and MRI are valuable tests in these cases. X-rays are not usually used and will not show tendon damage.
Consultation with an orthopedic or podiatric surgeon will determine the best treatment option for you. When conservative measures fail and for tendons completely torn, surgical intervention is usually considered to be the best option with a lower incidence of re-rupture. Surgery involves reattaching the two torn ends. In some instances, a graft using another tendon is required. A cast or walking boot is used post-operatively for 6-8 weeks followed by physical therapy.
Most people return to close to normal activity with proper management. In the competitive athlete or very active individual, surgery offers the best outcome for those with significant or complete tears, to withstand the rigors of sports. Also, an aggressive rehabilitation program will expedite the process and improve the outcome. Walking with full weight on the leg after surgery usually begins at 6 -8 weeks and often requires a heel lift to protect the tendon. Advanced exercises often begin at 12 weeks and running and jumping 5-6 months. While a small bump remains on the tendon at the site of surgery, the tendon is well healed at 6 months and re-injury does not usually occur.
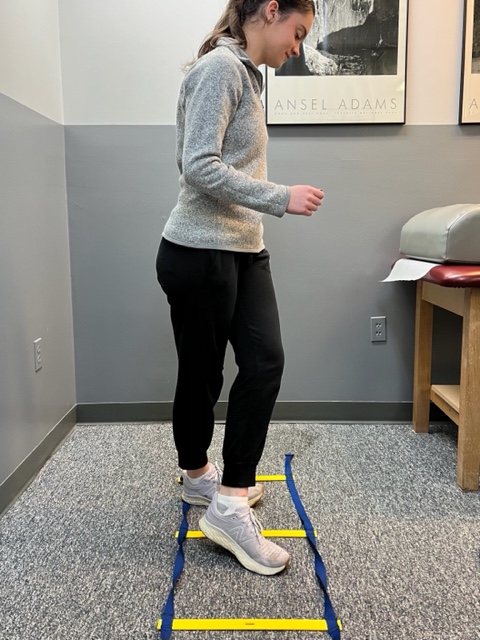
Prevention of muscle and tendon tears is critical for healthy longevity in sports and activities. In addition to the Achilles tendon, the tendons of the quadriceps (knee) and rotator cuff (shoulder) are also vulnerable. A comprehensive prevention program includes: gradual introduction to new activities, good overall conditioning, sport specific training, pre-stretch warm-up, stretch, strengthening, proper shoes, clothing, and equipment for the sport and conditions. Also, utilizing interval training, eccentric exercise (lowering body weight slowly against gravity – Photo 1) and proprioceptive and agility drills are essential (Photos 2 & 3).


In PHOTO 1a & 1b: Eccentric Lowering and Lengthening: for the Achillies tendon during exercise. Beginning on the ball of both feet (1a), bend the strong knee to shift the weight onto the weak leg (1b). Slowly lowering the ankle/heel to the ground over 5-6 seconds. Repeat.
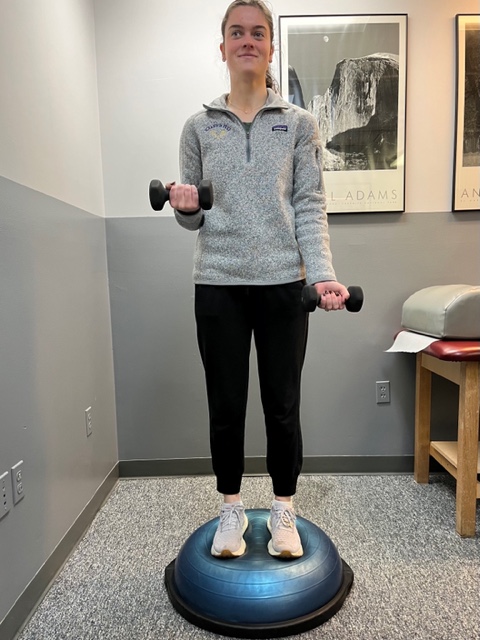
In PHOTO 2: Proprioceptive Training: for the Achillies tendon. Standing on a Bosu Ball while exercising the upper body (for example, biceps curls, shrugs, rows, lats) while maintaining balance on the ball.
PHOTO 3: Agility Drills: for the Achilles tendon involves stepping through a “gait ladder” in various patterns and at various speeds.
MODEL: Kerry McGrath, student physical therapy aide at Mackarey Physical Therapy
Sources: MayoClinic.com;Christopher C Nannini, MD, Northwest Medical Center;Scott H Plantz, MD, Mount Sinai School of Medicine

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's articles, visit our exercise forum!