

Guest Author: Matt Miraglia, DPT
Matthew Miraglia – received a Doctor of Physical Therapy degree from Temple University in May of 2019 and interned at Mackarey Physical Therapy. He grew up in Plains, PA and graduated from Coughlin High School in Wilkes-Barre. Prior to PT school, he received a bachelor of science in kinesiology from Temple University. Matthew plans to graduate with his doctoral degree in May and work in an outpatient physical therapy clinic in the Wilkes-Barre/Scranton Area.
As discussed last week in Hip Replacement Updates – Part 1, there are a wide variety of reasons for why a total hip arthroplasty (THA), or replacement, may be needed, as well as steps that lead to requiring a total hip replacement. Those that do eventually require a THA should be well prepared for their rehab journey going forward, both before and after the surgical procedure. This article will discuss potential precautions after surgery, as well as a few exercises that will serve as a foundation for the rehabilitation process going forward.
Your surgeon should have discussed with you the type of approach that he/she will be performing, and post-operative precautions that you should be aware of. Depending on the procedure approach, it is critical that recommended precautions are followed in order to protect the integrity of the joint replacement, and allow for proper healing.


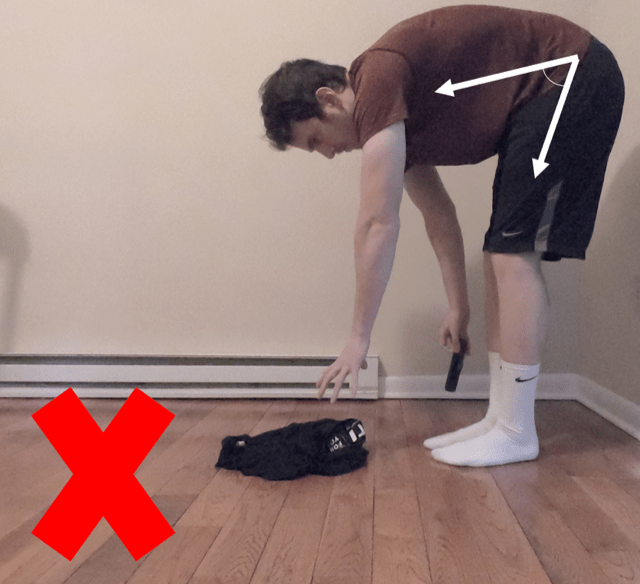

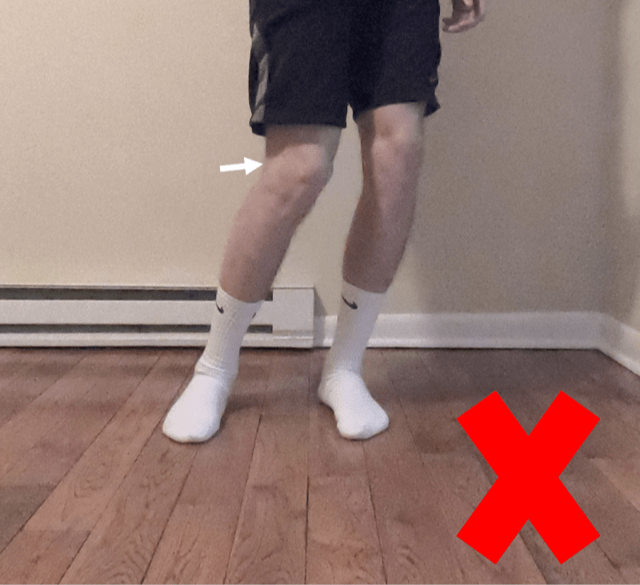
By following these precautions, your hip will be allowed to heal without putting additional strain on the replacement
In addition to precautions, your surgeon should also discuss your ability to bear weight on the affected limb. Most patients are weight bearing as tolerated after surgery, meaning they can put as much weight as they are able to through the leg, but depending age, body type, and if there were any potential surgical complications, weight bearing status may be different. Often a walker is need for a short time after surgery and then advanced to a cane.
Prior to surgery and immediately after surgery there are a few simple exercises that will either maintain (prior to) or help restore (afterwards) hip strength and mobility regardless of the surgical approach utilized. These exercises include: (See Photos)
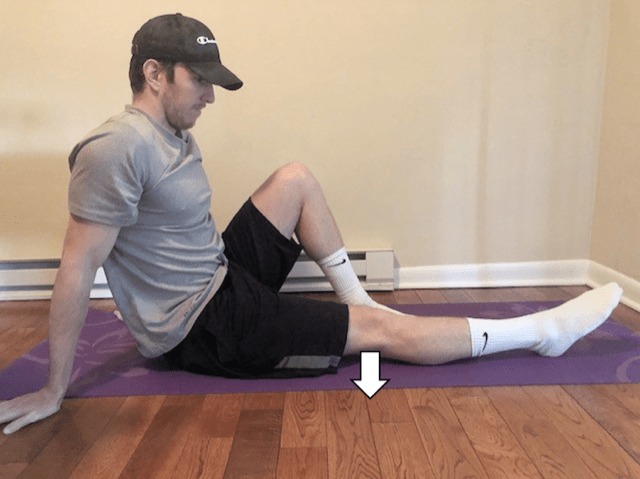

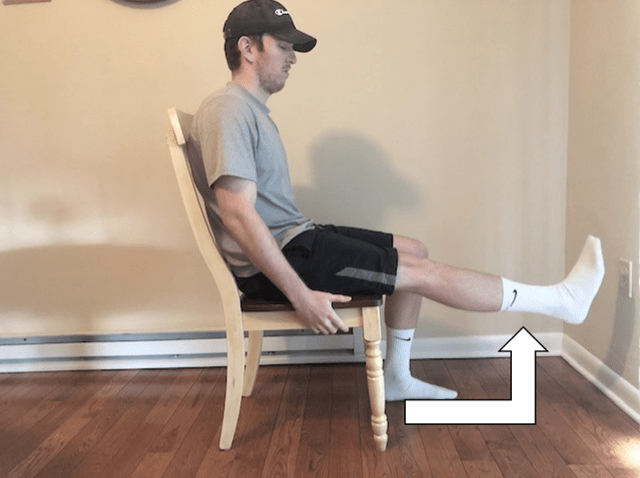
These exercises will serve as a base for strength and mobility of the hip until pain levels begin to decrease and you are able to tolerate and participate in exercises that require greater mobility in order to complete. Eventually, after a strong base has been formed with strength and mobility of the hip, functional activities will be reintroduced in order to make daily activities easier and more comfortable (walking, climbing stairs, sitting to standing, etc.)
Often, it is recommended that a patient see a doctor of physical therapy before surgery to review the procedure, prepare the home environment for safety and to begin a pre operative exercise program.
In summary, hip replacements have been shown to be one of the most stable of all joint replacements with good outcomes. This article highlights surgical precautions and gives a brief overview of the initial rehabilitation process after surgery. If you have further questions about your specific condition and your surgical treatment plan, you should consult your orthopedic surgeon or physical therapist to help guide you through the process.
For more information visit: American Academy of Orthopedic Surgeons at www.aaos.com
Visit your doctor regularly and listen to your body.
NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine (formerly The Commonwealth Medical College).