Since 1949 May has been designated as National Mental Health Month for the purpose of eliminating the stigma associated with mental illness by raising awareness. One of the most common mental health conditions is depression. New research from Boston University School of Public Health has found that depression has been increasing in the United States and life with COVID for more than two years has accelerated it rapidly. In 2021 the number of people suffering from depression increased more than 32 percent, affecting 1 in every 3 American adults. However, research also has good news to offer: one of the most understated benefits of exercise is mental health! Specifically, aerobic exercise (exercise that increases your heart rate for 30 minutes or more) such as walking, biking, running, swimming, hiking, elliptical & stepper machines to name a few, is the secret to “runner’s high.” This exercise euphoria is not limited to runners alone, but all who engage in aerobic exercise are more likely to experience high energy, positive attitude, and mental wellness.
Physical activity, specifically aerobic exercise, is a scientifically proven useful tool for preventing and easing depression symptoms. Studies in the British Journal of Medicine and the Journal of Exercise and Sports Science found that depression scores were significantly reduced in groups that engaged in aerobic running, jogging or walking programs, 30-45 minutes 3-5 days per week for 10-12 weeks when compared to a control group and a psychotherapy counseling group.
Depression is the most common mental disorder and is twice as common among women as in men. Symptoms include: fatigue, sleeplessness, decreased appetite, decreased sexual interest, weight change, and constipation. Many of these symptoms are likely to bring an individual to their family physician.
According to research, exercise reduces depression in two ways, psychologically (mentally) and physiological (physically).
Psychological or Mental Benefits of Exercise on Depression:
Physiological or Physical Benefits of Exercise on Depression:

NEXT MONDAY - Read Dr. Paul J. Mackarey’s "Health & Exercise Forum"!
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's Articles, check out our Health and Exercise Forum!
Farmers and gardeners in NEPA always say that Memorial Day, the “kick off” day for planting without the fear of frost, however, it is not too early to start to prepare…not only the beds but your body! While gardeners are anxious to work in their gardens and enjoy the fruits of their labor, a relaxing and enjoyable activity can turn dangerous quickly. Precautions are necessary as repetitive stress injuries such as shoulder and elbow tendonitis and carpal tunnel syndrome can stem from raking, weeding, digging and pruning. Additionally, simple scrapes, blisters, and bites can turn into serious problems if not treated appropriately. Since prevention is the best approach, the American Society of Hand Therapists (ASHT) promotes warm-up exercises and injury prevention tips to help all levels of gardeners avoid serious and long-term injuries while enjoying this popular outdoor activity.
ASHT recommends following these upper extremity warm-up exercises prior to gardening:
Note: These exercises should never be painful when completing them. You should only feel a gentle stretch. Hold 10 seconds and repeat 5 times. Should you experience pain, please consult a physician or hand therapist.


1. Forward Arm Stretch: Fold your hands together and turn your palms away from your body as you extend your arms forward. You should feel a stretch all the way from your shoulders to your fingers. (PHOTO 1)
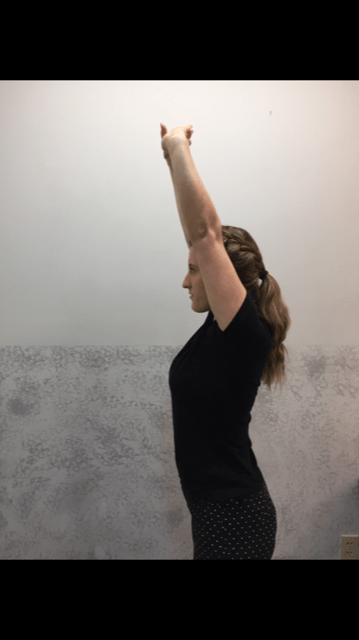
2. Overhead Arm Stretch: Fold your hands together and turn your palms away from your body, but this time extend your arms overhead. You should feel the stretch in your upper torso and shoulders to hand. (PHOTO 2)
3. Crossover Arm Stretch: Place your hand just above the back of the elbow and gently push your elbow across your chest toward the opposite shoulder. This stretch for the upper back and shoulder and should be performed on both sides. (PHOTO 3)
Professional Contributor: Nancy Naughton, OTD, CHT, is an occupational therapist and certified hand therapist practicing in NEPA. Model: Heather Holzman

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” Next Week: “Prevention of Gardening Injuries” Part II of II.
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. Access of all of Dr. Mackarey's articles at our Health and Exercise Forum.
After a long winter, spring is finally in the air as indicated by the warm (summer-like) temperatures last week. While your mind may be ready to play golf (and other outdoor activities), however, it is important to remember that without proper warmup and preparation, the risk of injury can increase substantially. PGA professionals benefit tremendously from sport science, physical therapy and fitness programs on tour year round. Amateur golfers in northern climates require diligence and planning to prepare for the game after 4-6 months off to avoid injury.
Muscle strains, ligament sprains, neck and LBP is prevalent in the early season for golfers, especially for the amateur. The reasons are many: general deconditioning after winter inactivity, poor golf swing mechanics, excessive practice, inadequate warm-up and poor flexibility and conditioning. The very nature of the golf swing can create great stress on the body, especially after time off.



NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM
Access all of Dr. Mackarey's articles at our Health and Exercise Forum
After a long winter, spring is finally in the air as indicated by the warm (summer-like) temperatures last week. While your mind may be ready to play golf (and other outdoor activities), however, it is important to remember that without proper warmup and preparation, the risk of injury can increase substantially. PGA professionals benefit tremendously from sport science, physical therapy and fitness programs on tour year round. Amateurs in northern climates require diligence and planning to prepare for the game after 4-6 months off to avoid injury.
Muscle strains, ligament sprains, neck and LBP is prevalent in the early season for golfers, especially for the amateur. The reasons are many: general deconditioning after winter inactivity, poor golf swing mechanics, excessive practice, inadequate warm-up and poor flexibility and conditioning. The very nature of the golf swing can create great stress on the body, especially after time off.
Get to the course early enough to make time to stretch before you play and hit a few balls at the range. Always start with low irons and work up to driver. Take a hot shower before an early morning round and use compression shorts and shirts on cool days. Do Not Bounce or Overstretch! Stretch slowly, holding for 10-20 seconds:
Visit your doctor regularly and listen to your body.
NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” Next Week: Part II - Preseason Golf Tips.

This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician.
For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit our Health and Exercise Forum
According to the American Diabetes Association (ADA), 32.2 million adults and children, 10.5% of the population in the United States, have diabetes. Unfortunately, one-third of these people are not aware that they have the disease. It will be the purpose of this column to raise the level of consciousness through education and offer recommendations for lowering blood sugar levels naturally.
Perhaps no goal is more important to a person with diabetes than maintaining a healthy blood sugar level. When managed over time, healthy blood sugar levels can slow the onset of complications associated with the disease. According to the ADA, pre-diabetes, or impaired glucose tolerance, occurs when blood glucose levels are higher than normal (110 to 125mg/dl) but below type 2 diabetes levels (126mg/dl). 54 million Americans have pre-diabetes in addition to the 20.8 million with diabetes.
While medications are effective in maintaining blood sugar levels, for those who are borderline, there are effective ways to lower your blood sugar naturally. Your physician will determine which treatment is most appropriate for your problem. Also, maintaining your ideal body weight is always important.
**This column is based on information from local physicians Kenneth Rudolph, MD, Gregory Borowski, MD, the American Diabetes Association L (ADA), and Lifescript

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles, visit our Health and Exercise Forum
Diabetes is a disease in which the hormone insulin is not adequately produced or used by the body. Insulin is needed for cells to take up glucose after it is broken down from sugars, starches and other food that we eat. When working properly, this provides the fuel necessary for activities of daily living. While the exact cause is not completely understood, genetics is known to play a big role. However, environmental factors such as obesity and inactivity have also been found to play a large role.
According to the American Diabetes Association (ADA), 10.5% of the population in the United States or almost 34.2 million adults and children has diabetes. Unfortunately, one-third of these people are not aware that they have the disease.
A Fasting Plasma Glucose Test (FPG) or an Oral Glucose Tolerance Test (OGTT) can be used to screen a person for diabetes or pre-diabetes. Due to the fact that it is easier, quicker and cheaper, the FPG is the recommended test by the ADA. A FPG test results between 110 and 125 mg/dl indicates pre-diabetes. A FPG of 126 mg/dl or higher indicates diabetes.
Type 1diabetes occurs when the islet cells of the pancreas are destroyed and unable to produce insulin. Without insulin the cells of the body are unable to allow glucose (sugar) to enter the cells of the body and fuel them. Without the hormone insulin, the body is unable to convert glucose into energy needed for activities of daily living. According to the ADA, 5-10% of Americans diagnosed with diabetes has type 1. It is usually diagnosed in children and young adults.
While type 1 diabetes is serious, each year more and more people are living long, healthy and happy lives. Some conditions that may be associated with type 1 diabetes are: hyperglycemia, ketoacidosis and celiac disease. Some things you will have to know: information about different types of insulin, different types of blood glucose meters, different types of diagnostic tests, managing your blood glucose, regular eye examinations, and tests to monitor your kidney function, regular vascular and foot exams.
While symptoms may vary for each patient, people with type 1diabetes often have increased thirst and urination, constant hunger, weight loss and extreme tiredness.
Type 1 diabetes increases your risk for other serious problems. Some examples are: heart disease, blindness, nerve damage, amputations and kidney damage. The best way to minimize your risk of complications from type 1diabetes is to take good care of your body. Get regular checkups from your eye doctor for early vision problems, dentist, for early dental problems, podiatrist to prevent foot wounds and ulcers. Exercise regularly, keep your weight down. Do not smoke or drink excessively.
Type 2 is the most common type of diabetes as most Americans are diagnosed with type 2 diabetes. It occurs when the body fails to use insulin properly and eventually it fails to produce an adequate amount of insulin. When sugar, the primary source of energy in the body is not able to be broken down and transported in the cells for energy, it builds up in the blood. There it can immediately starve cells of energy and cause weakness. Also, over time it can damage eyes, kidneys, nerves or heart from abnormalities in cholesterol, blood pressure and an increase in clotting of blood vessels.
Like type 1, even though the problems with type 2 are scary, most people with type 2 diabetes live long, healthy, and happy lives. While people of all ages and races can get diabetes, some groups are at higher risk for type 2. For example, African Americans, Latinos, Native Americans and Asian Americans/Pacific Islanders and the aged are at greater risk. Conditions and complications are the same as those for type 1 diabetes.
People with type 2 diabetes experience symptoms that are more vague and gradual in onset than with type 1 diabetes. Type 2 symptoms include feeling tired or ill, increased thirst and urination, weight loss, poor vision, frequent infections and slow wound healing.
**This column is based on information from local physicians Kenneth Rudolph, MD, Gregory Borowski, MD and the American Diabetes Association and Harvard Health Publications

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
Pain is different than discomfort! Muscle soreness and “feeling the burn” can occur during a normal healthy exercise routine. However, you should never experience a sharp, deep, intense, or lingering pain during or after exercise. In fact, if the soreness lasts more than 24-48 hours, than you did more damage than benefit to your muscles and other tissues and it is time to scale back and take time off. If necessary, use RICE (rest, ice compression and elevation). It is important to get in tune with your body and learn the difference between muscle strain and fatigue discomfort and pain from soft tissue damage from overuse and overload. Find the proper amount of weight and repetitions and gradually increase over time.
There is no solid evidence that stretching alone before a sport or activity prevents injury. In fact, over stretching may be counterproductive before a sport as it may weaken the muscle. The current wisdom on the matter is; never stretch a cold muscle. Instead, warm up for 5-10 minutes by actively moving the extremities and light jogging or biking and THEN lightly stretch the arms, legs, back etc. More vigorous stretching should be performed to improve the flexibility of tight muscles (ie calf and hamstring muscles) and best done after your workout but not before a sporting activity (tennis, basketball, etc.).
It depends on your body type and hormones! It is very unlikely that women and prepubescent males will bulk up from lifting weights…especially light weights (blame or thank hormones). It will, however, increase metabolism and fat burning efficiency which can lead to weight loss and good muscle tone. Stick with low resistance and high repetitions for best results.
It is not possible to target an area of the body to burn more fat! It is very common for women to ask for a specific exercise to reduce the fat in their buttocks, thighs, and abdomen. Regretfully, it is not possible to target weight loss in these areas or other body parts. In fact, when you lose weight through diet and exercise, the caloric expenditure will be evenly distributed throughout the body. However, once the adipose tissue in a specific part of the body such as the abdomen is reduced from general weight loss, targeting the area with exercises specific to that muscle group will improve the tone and definition for a leaner look in that region.
Sure, it would be great to dedicate 60 minutes 5 -6 days a week for exercise. But for most of us who work and raise a family it is not practical. The good news is that the research supports 30 minutes of exercise 3-5 days a week. Moreover, evidence shows that 10 minutes, three times a day, 5 days per week will help you attain the 150 minutes a week supported in most exercise studies.
Most people with the most common form of arthritis, osteoarthritis, feel better when they are moving. That is not to say that they don’t have increased symptoms when they OVERDO it. An exercise program specifically designed for a person’s problem and limitations will improve their symptoms and function. For example, if an individual has arthritis in their knees, they should use an exercise bike (partial weight bearing) or swim (buoyancy effect of water) instead of walk or run (full weight bearing) for aerobic exercise.
Furthermore, they would do far better with light cuff weights in a sitting or lying position to strengthen their legs than performing squats or lunges. It is important to remember, the weight gain and joint weakness and stiffness associated with a sedentary lifestyle will do more harm to an arthritic joint than a proper exercise program.
Not unless you are planning a killer workout! The number one reason most of us exercise is to lose or control body weight. High calorie sports drinks are counterproductive and unnecessary. If you do not plan on exercising for more than 60 minutes, good old fashion H2O is more than adequate. However, if you plan to do a “killer” workout for more than 60 minutes and may incorporate a high intensity interval training (HIIT) program, than a sports drink with electrolytes and other nutrients, may be of value.
For most of us, effective resistance training is not about the equipment. It is safe to say, caveman was pretty fit and strong despite the fact that he never went to a gym and lifted weights. He did however, lift, push, pull, and carry heavy stones, timber, and animals for day-to-day survival. So too, it is for modern man, the body does not distinguish between the resistance provided by a elastic band, dumbbell, or cable with pulleys and weight stacks. As long as the basic principles of strength training are applied, (isolating a muscle or muscle group, loading the muscle with enough force to bring it to fatigue without causing tissue damage, and allowing for adequate rest and recover) than the muscle will gain strength regardless of the type of resistance.
First, let me confess that I love to run and up until recently, ran almost daily. However, now that I am over 60, I had to find new forms of aerobic exercise which would be kinder and gentler to my joints. So, I mix it up between biking (indoors and outdoors, recumbent and upright), brisk walking or hiking, elliptical and stepper and swimming laps. Again, like the caveman weightlifting example, the body (heart and lungs) does not know what is causing an increase in heart rate for 30, 45 or 60 minutes, it only knows that it must respond to allow the body to function under this stress. And, in the process it becomes conditioned to the point that it will work much more efficiently when not under stress with a lower heart and respiratory rate and blood pressure at rest.
Those over 50 would be well-advised to engage in low-impact aerobics on a regular basis. For example, if you want to run two to three days per week, do not run two days in a row and consider performing low impact exercise in between. Some examples of low impact aerobics are walking, treadmill walking, swimming, elliptical trainer, and an exercise or road bike.
Change is necessary with age! For many years, I have repeatedly preached about the value of engaging in an active lifestyle throughout life. It is especially important to be active as one gets older to maintain mobility and independence. However, many take this advice to an extreme and refuse to accept the inevitable changes that occur in the body with age. They run, jump, lift and throw like a teenager and often fail to modify their activity or exercise regimen appropriately for their age. Consequently, they suffer from multiple injuries, including muscle tears, tendonitis, bursitis, impingement, and advanced osteoarthritis.
Keep in mind, everyone ages differently. One person at 60 years of age may be the equivalent of another at 50. However, change with age is inevitable, so be kind to your body…it’s the only one you have! It is always prudent to consult your physician and physical therapist for a program designed specifically for your needs.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
Access all of Dr. Mackarey's articles in our Health Care Forum!
PEOPLE WILL OFTEN ASK ME, “IS THERE SUCH A THING AS AN EXERCISE RUT?” THEY WANT TO KNOW WHY THEY DO NOT SEEM TO BE IMPROVING WITH THEIR EXERCISE PROGRAM…they exercise 3-4 times a week for 30 to 45 minutes and they feel frustrated and STUCK in a rut.
The purpose of this column will be to offer suggestions on how to improve or get more out of a “stale” exercise program. Last week’s column offered tips to improve a stale cardiovascular and strength program. This week we will discuss flexibility and functional training tips and include the components necessary for a healthy mind, body and spirit connection.
Flexibility training involves the careful stretching of the muscles, tendons and joints to improve the range of motion in order to safely perform daily activities and sports without injuring or tearing soft tissues. It is probably the most neglected part of the fitness program. However, while the amount of inherent flexibility varies for each person, a minimal range is necessary as it relates to daily activities and sports. For example, as you age it is important to have enough flexibility in your back, hips and knees to wash your feet, put shoes and socks on. Flexibility exercises should always be performed after a warm –up activity and done slowly and gently.
There are two types of flexibility exercises; dynamic and static. Dynamic stretching is performed with movement such as pushing the ankle up and down like a gas pedal. Passive stretching is performed using an outside force such as using a towel to pull the ankle up in order to stretch the calf. Dynamic should be performed before an activity (before running or playing tennis) and static performed after the activity is over in order to increase range of motion for future activities.
In conclusion, it is easy for fitness enthusiasts to get so focused on maintaining a routine that they allow their program to become stale and ineffective. It is essential to reassess and update your program to prevent stagnation.
Make sure the routine has all three fundamental components of a well-balanced exercise program; cardiovascular, strength and flexibility training. Moreover, to be truly healthy, one must work toward a “Healthy Mind, Body, and Spirit. Therefore, in addition to traditional exercise one must incorporate the following: nutrition; meditation, relaxation techniques, yoga, core fitness; functional/sports specific training; leisure sports and activities
In order to prevent an exercise program from getting stale, one must incorporate all aspects of wellness…a healthy mind, body and spirit!
While each component offers its own specific benefit, the combination of all three cooperatively provides unique value. Too often, fitness enthusiasts concentrate on the exercises they LIKE or are good at more than the ones they NEED.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine
For all of Dr. Mackarey's articles our Health Care Forum
People will often ask me, "Is there such a thing as an exercise rut?" They want to know why they do not seem, to be improving with their exercise program?... they exercise 3-4 times a week for 30 to 45 minutes and they feel frustrated and STUCK in a rut. While initially responding favorably to exercise, after 6 -9 months or more, they do not notice progress in weight loss, strength, tone, endurance or daily function.
Here are a few suggestions on how to improve or get more out of a “stale” exercise program.
Step one is to build an exercise program that is grounded in the basics. Next, Step two, which begins after the basics have been mastered, includes the components necessary for a healthy mind, body and spirit connection and translates into functional activities of daily living including work and leisure sports.
Make sure your routine has all three fundamental components of a well-balanced exercise program:
While each component offers its own specific benefit, the combination of all three cooperatively provides unique value. Too often, fitness enthusiasts concentrate on the exercises they LIKE or are good at more than the ones they NEED. A well-balanced program includes what you like and need!
In fact, recent studies show that those performing all three components surpassed those performing one or any combination of two of the training types when tested for efficient:
Cardiovascular exercise is any activity that raises your heart rate and respiratory rate. This type of exercise strengthens the heart muscle and the muscles that assist in breathing. When these muscles are stronger, they in turn work more efficiently to deliver oxygen to your muscles and other parts of the body. Ultimately, these oxygenated muscles can work harder and longer to burn fat during exercise and at rest.
*Most experts recommend at least 30 minutes of sustained cardio, 3-4 days per week. However, recent studies support the notion of performing 10-15 minutes, twice daily, 4 days per week. For those “stuck” in a fitness rut, to advance your program, cardio should be performed 5-6 days per week for 45-60 minutes.
Strength training is an activity that provides any type of resistance to muscle contraction to build strength in the muscle. The resistance can be without movement against an immovable object such as pushing against a wall (isometric) or with movement such as lifting up or lowering a weight down against gravity (isotonic/dynamic). There are two types of isotonic muscle contraction; concentric, which involves raising the weight against gravity as the muscle shortens and eccentric which involves lowering a weight against gravity as the muscle lengthens.
A standing biceps curl is an example that incorporates both concentric and eccentric contractions. A progressive strength training program includes all three types of muscle contraction. By using the classic bicep muscle curl these photos will demonstrate all three types of muscle contraction:


Sources: National Institutes of Health; American Council on Exercise
Model: Heather Holzman

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” Next Week: Read Stuck in an Exercise Rut…Part II of II!
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine
For all of Dr. Mackarey's articles visit: Mackarey's Health and Exercise Forum!
Tomorrow is Valentine’s Day! And, while you may wonder what that has to do with health and wellness, you might be surprised to learn that love can be good for your health! Studies show that it is in our DNA to seek out good relationships and that these solid relationships can lead to a happier, safer and healthier life. Conversely, infatuation and less committed, volatile relationships that are “on and off,” are very stressful and unhealthy. But those fortunate to participate in a stable and satisfying long-term relationship are the beneficiaries of many health benefits! Whether you have spouse, partner, or close friend, (love is love is love), feeling connected, respected, valued, and loved is critically important to your health and wellness!
The US Department of Human Services found that couples in a committed long-term relationship are less likely to require sick visits to their physician. And, when hospitalized, these “love birds,” have shorter hospital stays. One theory for this health benefit is that couples in good relationships watch after each other to ensure regular healthy visits for routine care and testing. Consequently, they are less likely to have unexpected serious illnesses.
Experts feel that social isolation is associated with unhealthy behavior and depression. Happy, loving and committed couples are far less likely to suffer from depression. Furthermore, these couples are less likely to engage in risky and unhealthy behaviors such as excessive drinking and drug abuse.
Researchers have found a strong relationship between marital status and blood pressure. Happily married couples have the lowest, while unhappily married couples have the highest. Happy singles scored somewhere in between. It is also interesting to note that non married committed couples and well-adjusted singles with strong support groups had lower blood pressure.
Studies show that long-term committed couples have far less anxiety than new romance. MRI brain scans found both groups showed high activation in areas of the brain related to romance, but only new couples had activation of the area of the brain associated with anxiety.
A CDC report on pain included a study of more than 127,000 adults and found that married people were less likely to complain of headaches and lower back pain. In fact, one study showed, when a happily married couple held hands, pain thresholds improved and, the happier the marriage, the greater the effect
Similar to the findings on pain, there is a strong link between happy and committed couples and stress management. The support and love from a strong and healthy relationship provides good coping methods to help overcome adversity…job loss, illness etc.
Solid loving relationships can boost your immune system. In fact, researchers at Carnegie Mellon University found that people who exhibit positive emotions are less likely to get sick after exposure to cold or flu viruses.
It may be that a wound from “Cupid’s Arrow” will heal faster when you are in a loving relationship. Researchers at Ohio State University Medical Center gave married couples superficial wounds and followed their healing time. The wounds healed nearly twice as fast in spouses who interacted warmly compared with those who behaved with hostility.
Strong research indicates that married people live longer. Researchers found that people who had never been married were 58% more likely to die than married people. Some reasons purported were mutual financial, emotional and physical support and assistance from children. One common denominator for a short life span is loneliness and those in a healthy relationship may live longer because they feel loved and connected.
A study in the Journal of Family Psychology showed that happiness depends more on the quality of family relationships than on the level of income. So, according to the research, when it comes to a long, happy and healthy life…love is more important than money!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM
For all of Dr. Mackarey's articles visit our "Health and Exercise Forum"