In 2000, President Bill Clinton dedicated March as National Colorectal Cancer Awareness Month. The purpose of this designation is to increase public awareness of the facts about colon cancer – a cancer that is preventable, treatable and has a high survival rate. Regular screening tests, expert medical care and a healthy lifestyle, which includes a proper diet and exercise, are essential for prevention. Several studies have demonstrated that exercise can also help prevent colon cancer.
The American Cancer Society estimates that there will be approximately 107,000 new cases of colorectal cancer in 2023. Of these, 52,550 men and women will succumb to the disease. It is the second-leading cause of U.S. cancer deaths for both men and women combined. The good news is incidence and mortality rates are dropping both nationally as well as in northeast Pennsylvania. The bad news is northeast Pennsylvania still has increased incidence and mortality rates when compared to the national average.
Studies show that prevention of this disease is multifaceted and includes: engaging in daily exercise, eating a low-fat diet with little red meat, avoiding smoking, drinking in moderation and having regular colonoscopy screenings.
Early detection is the key to survival. Death from colorectal cancer can be eliminated if caught at the earliest signs of disease. Colorectal cancer progresses very slowly, usually over years. It often begins as non-cancerous polyps in the lining of the colon. In some cases, these polyps can grow and become cancerous, often without any symptoms. Some symptoms that may develop are: blood in stool, changes in bowel movement, feeling bloated, unexplained weight loss, feeling tired easily, abdominal pain or cramps, and vomiting. Contact your physician if you have any of these symptoms.
The risk of colon cancer increases with age, as 90 percent of those diagnosed are older than age 50. A family history of colon cancer increases risk. Also, those with benign polyps, inflammatory bowel disease, ulcerative colitis or Crohn’s disease are at greater risk and should be screened more frequently.
The intestine works like a sewage plant, recycling the food and liquid needed by your body. However, it also stores waste prior to disposal. The longer the wastes remain idle in your colon or rectum, the more time toxins have to be absorbed from you waste into the surrounding tissues. One method in which exercise may help prevent colon cancer is to get your body moving, including your intestines. Exercise stimulates muscular contraction called peristalsis to promote movement of waste through your colon.
Exercise to prevent colon cancer does not have to be extreme. A simple increase in daily activity for 15 minutes, two times per day or 30 minutes, once per day is adequate to improve the movement of waste through your colon. This can be simply accomplished by walking, swimming, biking or playing golf, tennis or basketball. For those interested in a more traditional exercise regimen, perform aerobic exercise for 30-45 minutes four to five days per week, with additional sports and activities for the remainder of the time. For those in poor physical condition, begin slowly. Start walking for five to 10 minutes, two to three times per day. Then, add one to two minutes each week until you attain a 30-45 minute goal.
Medical Contributor: Christopher A. Peters, M.D - Dr. Christopher Peters is a partner of Radiation Medicine Associates of Scranton (RAMAS) and serves as medical director of Northeast Radiation Oncology Centers (NROC). He is an associate professor of clinical medicine at GCSOM.
Sources: American Cancer Society/Northeast Regional Cancer Institute, and CA Cancer J Clin.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

This year, Valentine’s Day is Valentine’s Weekend! And, while you may wonder what that has to do with health and wellness, you might be surprised to learn that love can be good for your health! Studies show that it is in our DNA to seek out good relationships and that these solid relationships can lead to a happier, safer and healthier life. Conversely, infatuation and less committed, volatile relationships that are “on and off,” are very stressful and unhealthy. But those fortunate to participate in a stable and satisfying long-term relationship are the beneficiaries of many health benefits! Whether you have spouse, partner, or close friend, (love is love is love), feeling connected, respected, valued, and loved is critically important to your health and wellness! So celebrate Valentine's Day and enjoy all the love that surrounds you!
SOURCES: WebMD

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

This column is dedicated to the family and friends of Rosemay “Rosie” Malloy and her wonderful disposition and laughter. Losing Rosie this past fall has left a painful void for those among us who were fortunate to know her and call her friend. Moreover, Rosie was an inspiration and role model for all who were paying attention…she was the embodiment of a quote by Dr. Paul Mercer, “laughter is the best medicine!”
Despite having her share of serious health problems that would wipe the smile off any reasonable face Rosie smiled her way to health and happiness. And, if she wasn’t up to the smiling task, she was always surrounded by her laughing and smiling family….it was contagious and infectious!
*Scientific evidence supports the notion that “laughter is the best medicine” as studies of tens of thousands of seniors found that those who find it difficult to laugh and smile have a much higher risk of developing functional disabilities. The biological explanation of how laughter reduces stress, anxiety and depression has to do with the stress-reducing effects of suppressing epinephrine and cortisol while enhancing the levels of dopamine and serotonin which are hormones linked to happiness. In fact, deficiencies in both dopamine and serotonin are linked to depression.
While laughter has been found to decrease stress and improve mood, it has also been linked to improved physical and mental resilience. It is good for relationships and a powerful tool for dealing with conflict and tension.
Recent research is very encouraging and supports the use of laughter and exercise to prevent and treat depression as a powerful adjunct to therapy and medication. While it is important to state that depression is no laughing matter, many mental health professionals support it as a method to confront an unpleasant situation and gain some level of control over it. One study showed that elderly people who used humor on a regular basis, reported improved satisfaction in life as compared to their less humorous contemporaries.
*Sources: NIH, Japanese Gerontological Evaluation Study, LifeScript.com

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Last week, this column discussed the many benefits of snowshoeing as an option for those in NEPA to get outdoors and enjoy the winter. Today’s column will present another option for outdoor exercise when the weather is inclement…winter walking or running.
We live in such a beautiful environment. Each season brings its own unique beauty and winter is no different. Most will not have to abandon outdoor activities, but you must make some adjustments in equipment, clothing and food for each season and temperature changes that go with it. These tips are also appropriate for those who qualified for the Boston Marathon in the spring and will be training all winter, as well as those who enjoy walking and running throughout the winter for exercise. Consider the importance of making changes and adjustments in training as well as clothing and equipment, according to the weather and temperature.
There are running shoes specifically designed for use in wet, cold and sloppy winter conditions. These running shoes, which can also be used for walking, are considered “winterized” because they offer waterproofing, sealed seams, gaiter collars to keep out snow and slop, slip resistant fabric, anti-roll stability features, anti-microbial material and aggressive tread patterns for traction on slippery surfaces. Some shoe recommendations for both walkers and runners include:
Additionally, I am a strong proponent of walking with trekking poles for improved balance and safety when brisk walking in winter conditions. They are light weight, adjustable, and collapsible. Some examples are: Trekology Trek Z 2.0 – 45. and REI Co-op Trailmade $79.00. Also, an old pair of ski poles will work just fine.
Over the past several years great strides have been made on understanding the effects of extreme temperatures on performance. Current wisdom from the University of Otago in New Zealand has found:
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

When I was a young boy growing up in NEPA, one of my favorite winter things was to walk in the freshly fallen snow. I loved the feel of fresh crisp air through my lungs, the mesmerizing sparkle of snow falling in the moonlight, the peaceful sound of silence as pedestrian and motor traffic came to a halt and only thing audible was the muffled sound of my boots as they crunched the snow beneath… for me, if it is sizzling hot in hell, it snows in heaven! Well, I am happy to share with you, as I struggle to hold on tightly to my “inner child,” I am as excited and inspired by a walk in the snow today, as I was 45 years ago. It is my hope, that this column will inspire my readers to consider a beautiful walk in the snow to rediscover their “inner child.”
While there are many options and opportunities available to enjoy winter in NEPA such as downhill skiing, cross country skiing, winter mountain biking, ice skating, and sled riding, none is as easy and natural as snowshoeing.
The advantages are many:
As a result, the popularity of snowshoeing is growing rapidly. According to the Outdoor Industry Association, the number of snowshoe participants have increased by 7.5% to 4.1 million in 2011 and 40.7% overall since 2008.
History (Raquettes GV, Quebec, Canada info@gvsnowshoes.com)
While the advent of the wheel is estimated to have been approximately 3,500 BC, the snowshoe had already been established and developed by 6,000 BC according to Stone Age engravings found in Norway. The snowshoe was an instrumental tool used by early humans to cross the Bering Strait into North America.
Some historians feel the snowshoe developed, like many great inventions, as an imitation of nature. For example, animals such as the snowshoe hare use expansive feet to increase their surface area, limit sinking and move more efficiently through the deep snow. Hardwood frames with leather webbed lacing comprised the early snowshoes used by fur trappers, traders, and Native Americans. More recently, materials have advanced and light but durable aluminum frames comprise snowshoes that are used by park rangers and winter recreation enthusiasts.
Like all sporting equipment, you usually get what you pay for. Snowshoes range in cost from $50.00 to $300.00. Most people will be fine in a good pair for under $100.00. LL Bean and Dick’s Sporting Goods and Sierra Store offer several affordable options.
Some equipment examples are Tubbs Wayfinder Flat - $199 and Redfeather - $82.00. Ski poles are recommended for efficiency when snowshoeing. Traditional ski poles or adjustable hiking poles can be used. Warm and supportive winter boots or hiking shoes are essential.
Now you are ready to go! The next time a snow storm dumps 8 – 10 inches on NEPA, get outside BEFORE the streets are plowed. Put on you warm winter boots, strap them into the bindings of your new snowshoes and walk out your front door and explore your neighborhood as you have never seen it before...white, clean, glistening, crisp and quiet. Let your mind wander, enjoy winter and rediscover your inner child!
Next Week: Part II of II...Winter Walking and Running
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

The number one New Year’s Resolution in the United States is to lose weight. A close second is to gain control over one’s life. One of the best ways to lose weight is thought diet and exercise. It can also be a very effective method to begin taking control of one’s life. This is especially true for those suffering from stress, anxiety and depression. This year make your New Year’s Resolution to “Get a Runner’s High on Life!”
Specifically, aerobic exercise (exercise that increases your heart rate for 30 minutes or more) such as walking, biking, running, swimming, hiking, elliptical & stepper machines to name a few, is the secret to “runner’s high.” This exercise euphoria is not limited to runners alone, but all who engage in aerobic exercise are more likely to experience high energy, positive attitude, and mental wellness – not to mention burn calories.
Physical activity, specifically aerobic exercise, while well known for its importance to one’s physical well-being has also been scientifically proven valuable for preventing and easing stress, anxiety and depression. Studies have found improvement in mental health for groups that engaged in aerobic running, jogging or walking programs, 30-45 minutes 3-5 days per week for 10-12 weeks when compared to a control group and a group in counseling.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.comPaul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

The “first Thanksgiving” was in 1621 between the Pilgrims of Plymouth Colony and the Wampanoag tribe in present day Massachusetts to celebrate the harvest and other blessings of the previous year. In 1789, President George Washington, at the request of Congress, proclaimed Thursday, November 26, as a day of national thanksgiving. In 1863, Abraham Lincoln proclaimed the national holiday of Thanksgiving to be the last Thursday of November.
Americans and Canadians continue to celebrate this holiday as a time for family and friends to gather, feast, and reflect upon their many blessings. Like most, I am very grateful for the simple things; family, good friends, food, shelter, and health. It turns out that being grateful is, not only reflective and cleansing; it is also good for your health!
Grateful people are more likely to behave in a prosocial manner, even when it is not reciprocated. A study by the University of Kentucky found those ranking higher on gratitude scales were less likely to retaliate against others, even when others were less kind. Emmons and McCullough conducted one of the most detailed studies on thankfulness. They monitored the happiness of a group of people after they performed the following exercise:
There are many things in our lives, both large and small, that we might be grateful about. Think back over the past week and write down on the lines below up to five things in your life that you are grateful or thankful for.” The study showed that people who are encouraged to think of things they’re grateful for are approximately 10% happier than those who are not.
Amy Morin, psychotherapist, mental health trainer and bestselling author offers this advice: “Developing an “attitude of gratitude” is one of the simplest ways to improve your satisfaction with life. We all have the ability and opportunity to cultivate gratitude. Simply take a few moments to focus on all that you have, rather than complain about all the things you think you deserve.” So…be grateful and have a happy Thanksgiving!
Source: NIH, Forbes, Amy Morin “13 Things Mentally Strong People Don’t Do.”
Visit your doctor regularly and listen to your body.
Keep moving, eat healthy foods, exercise regularly, and live long and well!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Recently, two patients asked me when I thought it would be safe for them to return to their exercise programs after abdominal surgery. She stated that she was not sure how to properly and safely implement or return to her program.
This column will attempt to ensure a safe return to activity and exercise following general surgery such as gall bladder, appendix, hernia, etc. The post-operative patient has many questions: When is it safe to begin an exercise program? How do I begin? What is the best exercise? Which exercises are best? How do I know if the activity is too intense or not intense enough? Are there safe guidelines?
Before you begin, discuss your intention to exercise with your surgeon and primary care physician. Get medical clearance to make sure you can exercise safely. With the exception of short daily walks, don’t be disappointed if your surgeon requires you to wait at least until your 6 week post-op check-up to begin exercise.
While a 60 minute workout would be the long term goal, begin slowly at 15-20-30 minutes and add a few minutes each week. Make time to warm up and cool down.
Warm-up 5-10 minutes
Strength Training 10-15-20 minutes
Aerobic 10-15-20 minutes
Cool down 5-10 minutes
How to Monitor Your Exercise Program:
First, determine your resting heart rate by taking your HR (pulse) using your index finger on the thumb side of your wrist for 30 seconds and multiply it by two. 80 beats per minute is considered a normal HR but it varies. This is a good baseline to use as a goal to return to upon completion of your workout. For example, your HR may increase to 150 during exercise, but you want to return to your pre exercise HR (80) within 3-5 minutes after you complete the workout.
For those who are healthy, calculating your target heart rate (HR) is an easy and useful tool to monitor exercise intensity.
220 – Your Age = Maximum Heart Rate
EXAMPLE for a 45 year old: 220 – 45 = 175 beats per minute should not be exceeded during exercise.
For those concerned about calories expended during exercise.
NOTE: Keep the level at a light/moderate level for the first four to six weeks and advance to the moderate/heavy at week six. The Very Heavy Level may not be appropriate for 12 weeks post op is for those who have a reasonable fitness level and exercise 4-5 days per week.
Example of Data Found on Fitness Equipment
Remember, this is only accurate if you program your correct height, weight and age.
Level kCal/min MET
Light 2 - 4.9 1.6 – 3.9
Moderate 5 - 7.4 4 – 5.9
Heavy 7.5 - 9.9 6 - 7.9
Very Heavy 10 - 12.4 8 – 9.9
Always secure physician approval before engaging in an exercise program.
If the patient is on beta blockers (Atenolol, Bisoprolol, etc), it is important to use the Borg Rating of Perceived Exertion Scale (RPE) scale to determine safe exercise stress since exercise will not increase HR as expected:
0 - Nothing at all
1 - Very light
2 - Light
3 - Moderate
4 - Somewhat intense
5 - Intense (heavy)
6
7 - Very intense
8
9 - Very, very intense
10 - Maximum Intensity
NOTE: Keep the RPE at 2-3 the first 6 weeks post op and advance to level 3-4 at 8-12 weeks post op. Levels 5-6-7 are for those with a reasonable fitness level and exercise 4-5 days per week. The advanced levels should not be attained until 2-3 months of exercise and 3-4 months post op.
MEDICAL CONTRIBUTOR: Timothy Farrell, MD, is a general surgeon at GCMC.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Fall has arrived in NEPA and walking is a great way to enjoy the fall foliage. Moreover, a new study has found that walking can reduce lower back pain. Researchers in Australia followed more than 700 adults who had a recent onset of lower back pain (and were able to bear full weight without associated leg symptoms) and enrolled them in a walking program under the supervision of a physical therapist. One group walked for 30 minutes, 3-5 times per week and the control group remained inactive. Both groups were followed for more than three years and discovered that the inactive control group was twice as likely to suffer from repeated flare-ups of lower back pain when compared to the walking group.
It is good news for those who enjoy walking, however, for many who have not maintained an active lifestyle or have health issues, it is challenging to know where to begin. Also, beginning without a good plan can lead to injury and leave you discouraged. For example, those overweight and de-conditioned should not start a walking program too aggressively. Walking at a fast pace and long distance without gradually weaning yourself into it will most likely lead to problems.
There is probably nothing more natural to human beings than walking. Ever since Australopithecus, an early hominin (human ancestor) who evolved in Southern and Eastern Africa between 4 and 2 million years ago, our ancestors took their first steps as committed bipeds. With free hands, humans advanced in hunting, gathering, making tools etc. while modern man uses walking as, not only a form of locomotion, but also as a form of exercise and fitness. It is natural, easy and free...no equipment or fitness club membership required!
Walking to reduce or control lower back pain is only one of many important reasons to begin a program. According to the American Heart Association, walking as little as 30 minutes a day can provide the following benefits:
Anything is better than nothing! However, for most healthy adults, the Department of Health and Human Services recommends at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous aerobic activity, or an equivalent combination of moderate and vigorous aerobic activity. The guidelines suggest that you spread out this exercise during the course of a week. Also aim to do strength training exercises of all major muscle groups at least two times a week.
As a general goal, aim for at least 30 minutes of physical activity a day. If you can't set aside that much time, try several short sessions of activity throughout the day (3 ten or 2 fifteen-minute sessions). Even small amounts of physical activity are helpful, and accumulated activity throughout the day adds up to provide health benefit.
Remember it's OK to start slowly — especially if you haven't been exercising regularly. You might start with five minutes a day the first week, and then increase your time by five minutes each week until you reach at least 30 minutes.
For even more health benefits, aim for at least 60 minutes of physical activity most days of the week. Once you are ready for a challenge, add hills, increase speed and distance.
Keeping a record of how many steps you take, the distance you walk and how long it takes can help you see where you started from and serve as a source of inspiration. Record these numbers in a walking journal or log them in a spreadsheet or a physical activity app. Another option is to use an electronic device such as a smart watch, pedometer or fitness tracker to calculate steps and distance.
Make walking part of your daily routine. Pick a time that works best for you. Some prefer early morning, others lunchtime or after work. Enter it in your smart phone with a reminder and get to it!
Studies show that compliance with an exercise program is significantly improved when an exercise buddy is part of the equation. It is hard to let someone down or break plans when you commit to someone. Keep in mind that your exercise buddy can also include your dog!
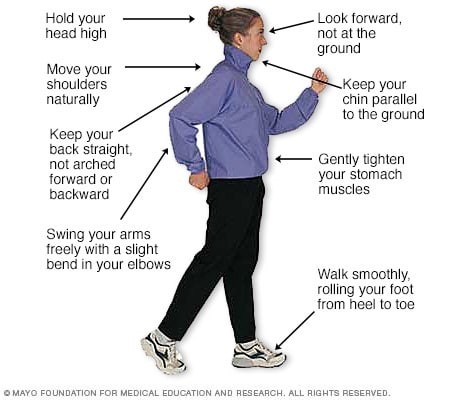
Like everything, there is a right way of doing something, even walking. For efficiency and safety, walking with proper stride is important. A fitness stride requires good posture and purposeful movements. Ideally, here's how you'll look when you're walking:
Sources : Sapiens.org; WebMD; Mayo Clinic, “Health & Science New”
Visit your doctor regularly and listen to your body

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Congratulations to more than 1,000 courageous runners who finished the 27th Annual Steamtown Marathon today. Most, if not all of you are waking up this morning with a little less jump in your step than you had yesterday.
As active people by nature, many of you will resist the logic of rest, despite the pain and stiffness in your muscles and joints. Therefore, I would like to offer some words of wisdom, based on science, to encourage you to adequately rest and allow your body to recover.
With adequate rest and recovery, an elite runner can quickly regain full form in 3-4 weeks, while an average runner may require 4-6 weeks. Meb Keflezighi, an elite American runner and winner of the 2014 Boston Marathon, is an excellent example of the merits of rest and recovery. However, he discovered it by accident…following the 2012 New York City Marathon, Meb developed a foot infection which required three weeks rest. With the Olympic Trials just 70 days away, Meb quickly regained his pre-injury fitness level to win the 2012 US Olympic Marathon Trials and join the US Olympic Team in London. It may be that his injury was fortuitous and allowed him adequate recovery time, (that he might not have otherwise allowed), preparing him for intensive training leading up to the trials.
The Effects of Running 26.2 Miles on the Body:
(RunNow.com - Jim Peskett)
One of the most obvious effects of running a marathon is significant muscle and joint pain and stiffness. It will set in after you sit for a while and attempt to get up and move around. For most, it will be more pronounced the day after the marathon, as you get out of bed and limp to the bathroom. Studies show that the leg muscles, (especially the calf muscles) display significant inflammation and necrosis (dead tissue) in the fibers of the muscle. In other words, the trauma to the muscles is so severe that tissue damage causes muscle cells to die. Consequently, studies found that muscle strength, power and endurance is compromised and required significant time to recover… sometimes as long as 4-6 weeks!
Additionally, many runners report severe bone and joint pain following the race. Some studies report findings of microfractures or bone bruising from the repeated and prolonged pounding of the marathon. It is purported that the stress on the joints may be related to: weight and body type, running shoes, running style and mechanics. While not dangerous, again, it is important to respect the stress placed on the body and allow adequate healing…LISTEN TO YOUR BODY!
Creatine kinase is an enzyme found in the brain, skeletal muscles and heart. It is found in elevated levels in the presence of cellular damage to these tissues, for example, following a heart attack. Similarly, significantly elevated creatine kinase levels are found in the blood of runners up to 4 days post marathon, demonstrating extensive tissue damage at the cellular level. It is important to note, that these enzyme markers are present, even if a runner does not experience muscle soreness. So, adequate rest for healing and recovery is required, regardless of soreness.
It is not a coincidence that the runners are more likely to contract colds and flu after intensive training or running 26.2 miles. The immune system is severely compromised after a marathon and without adequate recovery; a runner can become ill and ultimately lose more training time or will underperform.
FALSE: As stated above, enzyme levels that indicate cellular damage to the tissues are present in the post-marathon runner, even in those without significant pain.
FALSE: In addition to rest, drink, drink, drink - 24 ounces of water for every 2 pounds you lose after the marathon. This is based on pre and post exercise weight. You just burned 2,600 calories so avoid diet soft drinks. You need the glucose (sugar) boost. Also, don’t drink alcohol and use minimal amounts of caffeine (the equivalent of 1-2 cups of coffee). First, drink plenty of water and sports drinks (Gatorade) to prevent a diuretic like caffeine from messing up your fluid balance.
FALSE: Studies clearly show that the VO2 Max, (the best measurement of a runner’s endurance and fitness), is unchanged after one week of inactivity. And, after two weeks, the loss is less than 6% and can be regained quickly. Moreover, it is important to remember, without adequate rest and recovery, performance is comprised, not by the loss of VO2 Max, but by muscle-skeletal tissue damage, which renders the leg muscles of the runner weaker. Remember Meb Keflezighi!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
