June is migraine and headache awareness month! According to the World Health Organization about half of the world’s adult population has had a headache at least once in the past year. Prolonged use of electronic devices has greatly contributed to this problem. For many people, these headaches are infrequent and do not often affect daily life. But what about when your headache occurs frequently or is so severe it prevents you from going about your day to day activities? Some types of headaches are more easily treated and managed than others.
There are two types of headaches: primary and secondary. Primary headaches occur without an underlying disease and include migraines and tension-type headaches. Secondary headaches can be associated with serious disease, requiring emergency care, or can be referred from other structures of the body such as the cervical spine (neck).
Headaches symptoms that may constitute a medical emergency are: vomiting, seizures, fever, muscle pain, night sweat, weight loss, and neurologic symptoms such as blurred vision. If you are experiencing any of these symptoms, if your headache worsens, or your symptoms change it is recommended that you seek medical attention. Any headache that is unusual for you and does not resolve itself in a reasonable time should be brought to your primary care physician’s attention.
Migraines: Migraines are a primary form of headache that typically lasts from four to seventy two hours, can range from moderate to severe pain, and typically are located on only one side of the head. Often they can be accompanied by an aura, nausea or vomiting, sensitivity to sound, or light sensitivity. Migraines can be aggravated by routine physical activity such as going up stairs. This type of headache is thought to occur in the central nervous system.
Tension-type: Tension-type headaches are the most common primary headache disorder and can last anywhere from thirty minutes to seven days. These can often have a pressing or tightening quality that occurs on both sides of the head. Typically, there is no nausea, vomiting, or aggravation with physical activity, however, light or sound sensitivity can occur. This type of headache is thought to occur in the central nervous system but can have a hereditary component and is usually associated with muscle tender points. Tension – type headaches can be treated with relaxation techniques such as Progressive Muscle Relaxation (PMR), medications, and physical therapy.
The most common secondary headache that is not related to a serious medical condition is a cervicogenic headache (originating from the neck).
Cervicogenic Headache: The length of time a cervicogenic headache can last varies. Here the pain is on one side and usually starts in the neck. This type of headache is aggravated or preceded by head postures or movements of the neck. Due to the nerves of the neck and face sharing common connections, pain signals sent from one region can lead to discomfort in the other. Physical therapy can be an effective treatment to help relieve symptoms. For example: posture, exercise, ergonomics, massage, manual techniques, traction, trigger point, and acupressure.
A cervicogenic headache can be caused by an accident or trauma or can stem from neck movement or sustained postures. Sustained postures could mean sitting in front of a computer at work or looking down at your phone. Changing these postures throughout the day could help reduce symptoms. Changing postures could mean bringing your phone closer to you using pillows or another supportive surface when reading or checking social media. If you are someone who works at a desk, it could involve taking breaks or getting a standing desk. However your life requires you to move, there are some simple and effective exercises you can perform throughout the day to help cervicogenic headache symptoms.
Progressive Muscle Relaxation: PMR is an effective method for reducing tension throughout the body. With this method you first tense a muscle group, such as at the neck or shoulder, and then relax the muscles noting the difference between the two. This helps reduce both stress and tension. For more information or to learn how to do PMR, refer to podcast at: https://www.psychologies.co.uk/try-progressive-muscle-relaxation
Manage your stress level: While stressors vary from person to person, one method for managing stress is with exercise. Any form of exercise can help reduce stress, but a cost free method is aerobic exercise such as walking or running. A less time consuming method could be to perform deep breathing exercises throughout the day.
Heat or cold: When feeling sore or stiff, applying a hot or cold pack or taking a hot shower can help ease a tension headache.
Posture: Some tips for posture are to make sure your head is over your shoulders rather than sitting forward and making sure you are sitting or standing up straight with your shoulders back.
Over the counter medications: Talk to your doctor or pharmacist for additional information.
Posture: See tips listed under tension headaches.
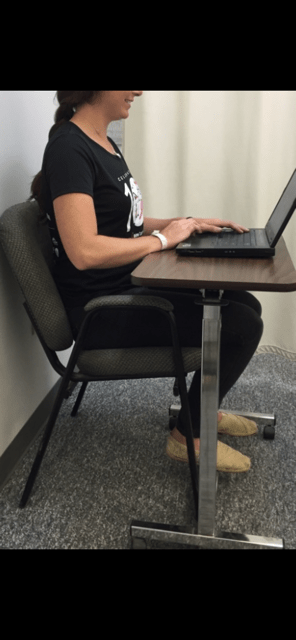
Ergonomics: If your job or hobbies require you to sit for extended periods it may be beneficial to change positions throughout the day or consider getting a standing desk. Also, limit time on electronic devices. When sitting make sure the monitor is at eye level, your legs are able to fit under your desk, and you are close to the keyboard and monitor. If you are working with a laptop or phone, avoid putting it on your lap. Instead, bring your laptop closer to you by putting pillows on your lap or using an ergonomic desktop. See photo below.
Exercise: Some exercises to help relieve symptoms are chin tucks, shoulder blade pinches, and back extension. These exercises can be performed multiple times throughout the day in sitting or standing.
Physical Therapy: Physical therapy may include massage, manual techniques, stretching, traction/ decompression and exercise. A physical therapist can assess your posture and provide strategies specific to you.
Over the counter medications: While medication may not cure cervicogenic headaches, they may help relieve pain. Talk to your doctor or pharmacist for additional information.
Visit your doctor regularly and listen to your body.

Dr. Chua is a neurologist and headache specialist at Geisinger Health System in Northeast Pennsylvania. In addition to caring for people with headache and facial pain disorders, Dr. Chua also serves as: Director of Headache Medicine at Geisinger, Clinical Director of Neurology at Geisinger Wyoming Valley, faculty at Thomas Jefferson University’s Advanced Headache Diagnosis and Management Post-Graduate Certificate Program, and Treasurer and Executive Board Member of the Association of Migraine Disorders. In her spare time, she enjoys going on adventures with her husband and toddler, learning new skills (she is now certified in battlefield acupuncture), and buying great books she will never have time to read!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Holiday shopping is stressful to your body, as well as your wallet, having the potential for a backache afterwards. Driving from store to store, getting in and out of the car, bundled in a sweater and winter coat, the expert shopper carries package after package from the store, to the car, over and over again. Six, eight, or ten hours later, the shopper arrives home exhausted, only to realize that 15, or 20 packages must be carried from the car into the house. This dilemma is compounded by the fact that the rain turned to sleet, and the sleet to snow. Travel by car and foot are treacherous.
You are slipping and sliding all the way from the car to the house while carrying multiple packages of various sizes and shapes. The shopping bags get wet and tear, forcing you to tilt your body as you carry the packages. Of course, no one is home to help you unload the car and you make the trip several times alone. You get into the house exhausted and crash onto the couch. You fall asleep slouched and slumped in an overstuffed pillow chair. Hours later you wake up with a stiff neck and a backache from shopping. You wonder what happened to your neck and back.
Plan Ahead: It is very stressful on your spirit, wallet and back to do all of your shopping in the three weeks available after Thanksgiving. Even though we dislike “rushing” past Thanksgiving to the next holiday, try to begin holiday shopping in before
Use the Internet: Supporting local businesses is important. However, Internet shopping can save you lots of wear and tear. Sometimes, you can even get a gift wrapped.
Gift Certificates: While gift certificates may be impersonal, they are easy, convenient and can also be purchased over the internet.
Perform Stretching Exercises: Stretch intermittently throughout the shopping day…try the three exercises below, gently, slowly, hold 3 seconds and relax, repeat 5 times.



Model: Paul Mackarey, PT, DPT, Clinic Director, Mackarey PT
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Part I of II
Difficulty sleeping during the COVID-19 quarantine has become a common problem and can be manifested in a variety of ways; insomnia, fragmented sleep and nightmares. National prescription providers have reported a 21% increase in anti-insomnia, anti-anxiety and antidepressant medications since March of 2020. The next two weeks in Health & Exercise Forum” will be dedicated to sleep wellness.
We do it every night, hopefully. Children are doing it. Our grandparents are doing it. Teenagers do it all the time. We sleep of course. These hours in which we slumber are vital to our ability to function during the day and to our health overall. It does not appear evolutionarily advantageous for us to be unconscious for extended periods of time. Modern science tells us that much of our body’s restoration, strengthening, and processing occurs while we sleep. Our brains consolidate the information they have learned throughout the day and enhance our memory. Additionally, sleep restores sugar storage in our brains and improves the functioning of our immune system. But science does not illuminate why we need such a prolonged period other than the fact that we just seem to get sleepy after a long day.
Sleep is crucial to us as a species, but it is not always easily attained. For many individuals across the globe, this author included, sleeping properly can be a challenge. The trial and tribulations of the human experience can lead to restless nights and early morning risings without adequate sleep. But what is considered “adequate” sleep? The answer depends on your age. As we grow older, our sleeping requirements change drastically from infancy to elderdom. Infants are learning and processing so much information of this new world they now inhabit. Thus, their brains need enough time to analyze and consolidate the data, necessitating 12 to 15 hours of sleep. As we advance into adulthood, our sleep requirements drop to approximately 7 to 9 hours with some variability from person to person. Good indications of a restful night’s sleep include waking up feeling refreshed, functioning with enough energy for your daily tasks, and having continuous sleep- meaning there are not extended periods of time of wakefulness when we are supposed to be sleeping.
This seems easy enough to say, but significantly more difficult to do. Current reports demonstrate that roughly 100 million people suffer from insomnia at some point each year, with 25% progressing to long-term chronic sleep insufficiency. Insomnia is described as difficulty falling asleep or staying asleep for three nights per week for at least two consecutive weeks in a three-month period. There are a lot of unhealthy sleeping habits permeating the country. We measure the quality of sleep in two different dimensions duration (quantity) and depth (quality). The duration is straightforward enough. Do you sleep for the recommended 7 to 9 hours per night? The quality is a little more difficult to quantitate. Some individuals may sleep for the proper duration of time, but the depth is not adequate. Sleep quality is determined by the number of arousals or awakenings in a given night. As few as 5 arousals in a night can result in daytime sleepiness and performance deficits. In addition, how long we remain in certain phases of sleep also determines the quality of our sleep. There are four stages of sleep: N1, N2, N3, and REM with N3 being the most restful of the stages. When we fall asleep, we go through a predictable descent into sleep. We repeat the cycle of N1 to N2 to N3 to REM sleep every 60 to 90 minutes. The more time we remain in the restful stages, N3 and REM, the better our sleep is. As we age, we inevitably spend less and less time in restful sleep.
There are many factors that influence how we sleep. Everything from what we drink to the type of curtains we have can impact those crucial hours of sleep. Some of the more common culprits that disrupt our sleep are:
For More Informations:
-http://healthysleep.med.harvard.edu/healthy/
-https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2110998
-https://www.sciencedirect.com/topics/medicine-and-dentistry/insomnia
Read Dr. Mackarey’s Health & Exercise Forum – every Monday. Next Week Read, Sleep and Wellness Part II.
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine.
Read all of Dr. Mackarey's articles in our health and exercise forum: https://mackareyphysicaltherapy.com/forum/
Guest Columnist: Timothy Farrell, MD3

Tim Farrell is a third year medical student at Geisinger Commonwealth School of Medicine. Originally from Clarks Summit, Pennsylvania, Tim received his bachelor’s degree from Loyola University Maryland in Baltimore, MD. Currently a 2nd Lieutenant in the US Army, he enjoys listening to music, running, and spending time with his two dogs. He volunteers with the Cody Barrasse Foundation in the Organ Transplant Assistance Program, where he helps patients receive grant funding as they await their transplant surgery. He hopes to pursue a career in General Surgery.