At least once a week, a patient jokingly asks if they can get a “lube job” to loosen up their stiff knee joint. I respond by providing them with information about osteoarthritis and viscosupplementation, a conservative treatment administered by injection and approved by the FDA for the treatment of osteoarthritis of the knee.
Osteoarthritis (OA) is also known as degenerative arthritis. It is the most common form of arthritis in the knee. OA is usually a gradual, slow and progressive process of “wear and tear” to the cartilage in the knee joint which eventually wears down to the bony joint surface. It is most often found in middle-aged and older people and in weight bearing joints such as the hip, knee and ankle. Symptoms include: pain, swelling, stiffness, weakness and loss of function.
Your family physician will examine your knee to determine if you have arthritis. In more advanced cases you may be referred to an orthopedic surgeon or rheumatologist for further examination and treatment. It will then be determined if you are a candidate for viscosupplementation. While this procedure is the most commonly used in the knee, it has also been used for osteoarthritis in the hip, shoulder and ankle.
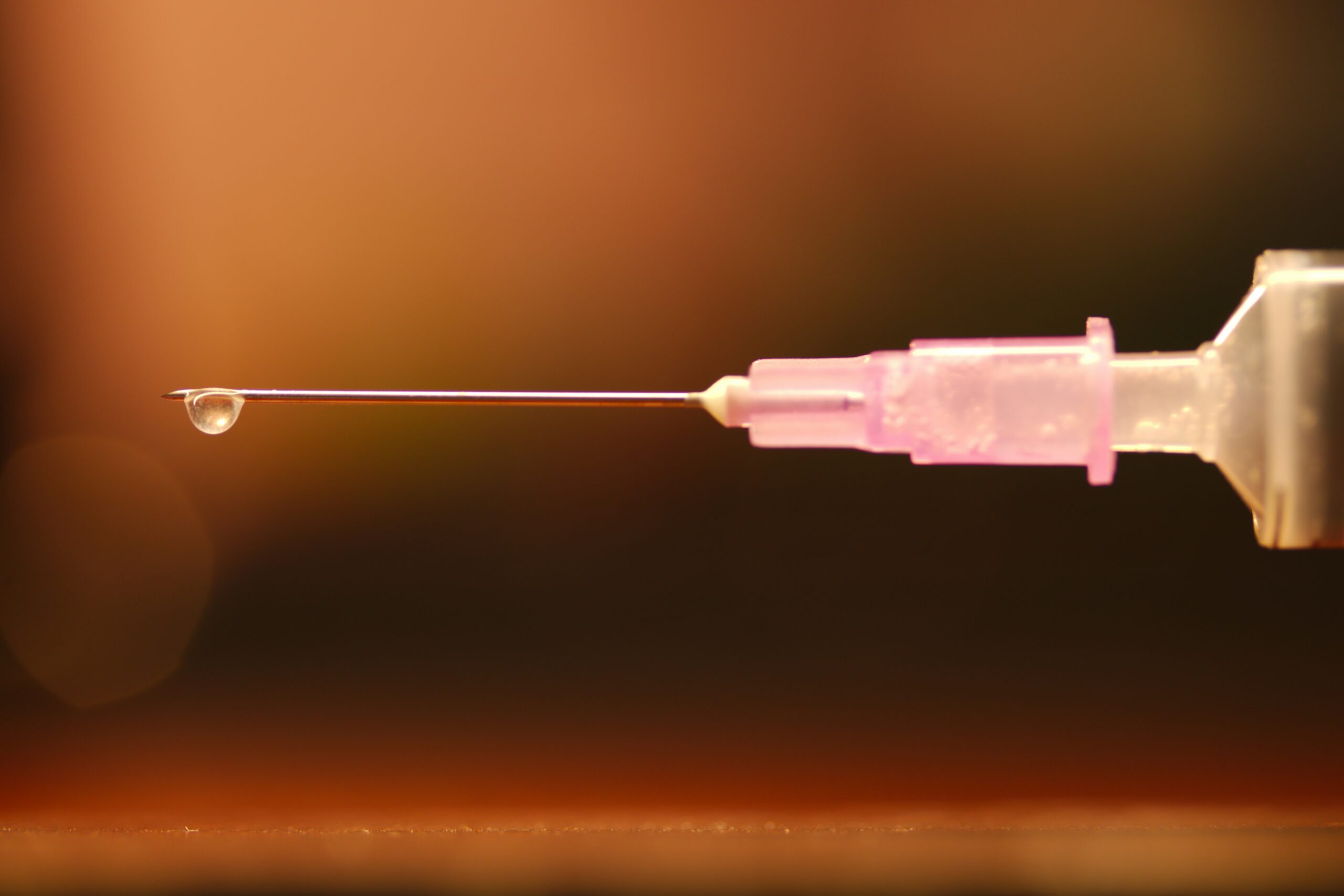
Viscosupplementation is a procedure, usually performed by an orthopedic surgeon or rheumatologist, in which medication injected into the knee joint acts like a lubricant.
The medication is hyaluronic acid is a natural substance that normally lubricates the knee. This natural lubricant allows the knee to move smoothly and absorbs shock. People with osteoarthritis have less hyaluronic acid in their knee joints. Injections of hyaluronic acid substances into the joint have been found to decrease pain, improve range of motion and function in people with osteoarthritis of the knee.
When conservative measures, such as anti-inflammatory drugs, physical therapy, steroid injections fail to provide long lasting relief, viscosupplementation may be a viable option. Often, physical therapy and exercise are more effective following this injection to provide additional long-term benefit. Unfortunately, if conservative measures, including viscosupplementation fails, surgery, including a joint replacement may be the next alternative.
In 1997 the FDA approved viscosupplementation for osteoarthritis of the knee. Presently, there are several products on the market. One type is a natural product made from the comb of a rooster. However, if you are allergic to eggs or poultry products or feathers, you should not use the natural product. The other medication is best used for patients with allergies because it is manufactured as a synthetic product.
The long-term effects of viscosupplementation is much greater when other conservative measures are employed:
SOURCES: Genzyme Co, Sanofi-Synthelabo Inc, Seikagaku Co. and American Academy of Orthopaedic Surgeons
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Human beings were designed to move…walk, run, climb, lift, hunt, and gather. Contemporary man has suffered greatly from a technologically driven inactive and sedentary lifestyle. Inactivity is associated with many health problems; obesity, adult-onset diabetes, high blood pressure to name a few. The problems associated with lack of movement are many:
The more you move your body, the more you colon moves! A regular and consistent exercise and activity regime, results in a more consistent bowel schedule, especially with age. Healthy muscle tone in your abdominal muscles and diaphragm is also the key to moving waste through your digestive tract.
Osteoarthritis, rheumatoid arthritis and many inflammatory or auto-immune diseases can cause achy and stiff joints. However, even healthy joints can also stiffen when you don’t use them enough. Put them to work so they don't get tight and cause pain.
All muscles get weak from lack of use, including the muscles that help your lungs expand and contract as you breathe if you don’t work them out regularly. The less exercise or activity you do, the more you experience shortness of breath, even during easy daily tasks.
Physical problems are not the only complication of inactivity. A lack of movement can also increase feelings of anxiety and depression. Aerobic exercises like walking, biking, swimming, or running, have been proven to stimulate endorphins to boost and steady your mood, and even improve your self-esteem.
Many studies have found that regular movement improves energy. Exercise helps deliver oxygen and nutrients to your tissues. When you sit or are inactive, tissues are not getting the same amount of fuel they need to keep you going.
Movement stimulates your metabolism. Hyperactive people burn more calories…just by fidgeting! Even if you are not hyperactive, the more active you are, the more calories you burn each time you move.
One of the first recommendations sleep doctors make to their patients suffering from insomnia is exercise. When you keep a regular exercise routine, you fall asleep faster, and you sleep deeper once you drift off.
Regular exercise tells your body to make more chemicals called growth factors. They boost blood vessel production in your brain. The more blood that gets to your brain, the better you can think, remember, and make decisions.
Spending most of your time sitting raises your risk of heart disease, in great part due to the fact that partly you’re more likely to have high blood pressure. This is a big risk factor for heart issues like coronary artery disease and heart attack.
When physical activity is a regular part of your life, your body has an easier time keeping your blood glucose under control. Exercise can stabilize blood sugar levels and keep you out of the type 2 diabetes danger zone.
When your core muscles are weak from lack of use, they can’t support your back the way they should. This makes it much easier to tweak your back muscles during everyday movements like standing or reaching. Pilates, yoga, and other exercises that use stretching are good for building a stronger back. Schedule an appointment with a good orthopedic and sports PT.
Logically, one might think that you’d be hungry more often if you exercised more, but the opposite is usually true. Aerobic exercise like biking, swimming, walking, and running can actually decrease your appetite because it changes the levels of certain “hunger hormones” in your body.
Studies show the more moderate activity you get, the lower your chance of catching a cold or other germs. When you make exercise a habit, your immune system gets stronger.
If your skin looks duller than usual, a lack of movement may be to blame. Some studies show that moderate exercise boosts your circulation and your immune system, which helps your skin keep that youthful glow.
SOURCE: WebMD

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
“Everybody talks about the weather, but nobody does anything about it,” said Mark Twain. Just ask 93% of the arthritis sufferers who believe that the weather affects their pain level. History tells us that Benjamin Franklin, Leonardo da Vinci, and Christopher Columbus also felt this way about the weather.
Patients at our clinic have been particularly sensitive to joint pain on cold, damp days, especially during the past few weeks. In my clinical practice of orthopedic and sports physical therapy, an informal survey found that 95 out of 100 patients (95%) with arthritis reported increased pain with weather changes. While most people report that the coldness and dampness seem to irritate their joints, they also report more pain with weather changes in the summer. There is a reasonable explanation…
Joints in the body have a lining called synovium that secretes a lubricating fluid called synovial fluid. In joints with arthritis, there is an overproduction of synovial fluid. In theory, when the barometric pressure changes, so to will the pressure inside your joints, especially if it is already overfull with extra fluid from arthritis. This added pressure stimulates the nerve endings in the joint to produce inflammation and pain.
Despite this overwhelming response from patients, scientific studies vary in their support of this claim. According to the Mayo Clinic, in 1961, a famous arthritis doctor (rheumatologist), built a climate chamber and discovered that when high humidity was combined with low barometric pressure, patients reported increased joint pain and stiffness. A recent study found that changes in barometric pressure and cooler temperatures are associated with joint pain. However, other studies have found increased joint pain with high barometric pressure in both warm and cold weather while another study found pain with low pressure.
What does this mean? It means that patients with arthritis consistently report pain with weather changes but science has not found an accurate method to consistently support these claims. Some of these inconsistencies may be attributed to the fact that there are differences in sensitivity among individuals. For example, some patients have symptoms before the weather changes, while others notice symptoms during or after the weather changes. Still yet, some report more pain in colder conditions while others notice more pain in warmer weather. It appears that changes in the weather, such as a high to a low or warm dry to cold damp and vice versa is the culprit when it comes to irritating arthritis in a joint.
If I have arthritis, should you move to Arizona? Yes and no! Yes, the warm and dry climate of Arizona will probably make you feel better overall. However, it will not cure the degenerative changes in your joints and you may still have pain when CHANGES in the weather occur. This is proven to be true by the fact that there are many very busy rheumatologists in Arizona!
In conclusion, it is safe to say that there is some evidence to support the claim that most patients with arthritis have increased symptoms of joint pain and stiffness with CHANGES in the weather:
Therefore, each patient must be individually evaluated by their physician to determine the extent of their arthritis and its relationship to the changes in the weather. While the cause of their increased symptoms with changes in the weather may not be completely understood, each patient must determine the adjustments in their lifestyle and/or medications according to the particular weather patterns that affect their problem most.
Visit your doctor regularly and listen to your body.

NEXT SUNDAY IN THE PAPER AND EVERY MONDAY'S BLOG – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's articles, visit our exercise forum!
“I can’t comb my hair.” “I can’t wash my back.” “I have a difficult time putting on my jacket.” “It’s hard for me to tuck my shirt in.” “I can’t reach for things on a high shelf.” These are all very common complaints from people with frozen shoulder. Also known as adhesive capsulitis, frozen shoulder is a condition that results in a tightness of the shoulder reducing its overall movement.
The bones which make up the shoulder joint are held together by a lose capsule of connective tissue. The connective tissue is loose to allow maximal movement of the shoulder, the most mobile joint in the body. With frozen shoulder, this loose connective tissue capsule tightens which restricts the overall movement of the shoulder. Another way to understand frozen shoulder is to look at the construction of the shirt or blouse you are presently wearing. All shirts have extra fabric in the armpit. This extra fabric allows for freedom of movement for the shoulder. Try this: grab the extra fabric under the armpit of your shirt and tightly squeeze it. Now, try to raise your arm over your head. You will notice that you will be unable to raise your hand over your head due to the restriction of the tight fabric. The fabric of the shirt is very similar to the connective tissue of the shoulder. A tightening of the connective tissue will restrict movement of the shoulder.
How does this connective tissue become tight? This is not completely understood. While some conditions are due to trauma, prolonged tendonitis or bursitis, most patients with frozen shoulder will state that “it just happened.” They indicate that they did not fall on it or suffer an injury; however, a gradual loss of movement occurred over the past several months. They do typically indicate that certain movements are painful such as reaching overhead or reaching behind their back. It is known that middle aged women are most prone to this condition and that individuals with diabetes are more commonly affected. Interestingly, right-handed individuals more commonly get frozen shoulder on their left side.
Treatment for frozen shoulder is varied. Most cases require some form of medical intervention. Physical therapy is commonly used to decrease pain, improve strength and range of motion and ultimately function. The physical therapist makes the tight connective tissue more pliable usually with moist heat and ultrasound immediately followed by manually stretching the connective tissue. As the connective tissue is stretched the movement of the shoulder gradually returns. This is a gradual process and treatment may last for several weeks or months. In severe cases, a surgeon will stretch out the connective tissue while the patient is under anesthesia. Following this surgical stretching, the patient is typically sent to physical therapy to maintain the stretch.
As indicated above, most cases of frozen shoulder require medical intervention. If you suspect that you might have frozen shoulder, it is recommended that you see your family physician or orthopedic surgeon and get a referral to a physical therapist.
Movement Is Your Best Friend - If you think you have frozen shoulder, you need to move the shoulder and move it a lot. If you baby the shoulder and protect it from movement the condition will get worse.
Pain Is Your Worst Enemy Yes, move the shoulder as much as you can but do not move it to the point of pain. If you move the shoulder to the point that it is now painful – the frozen shoulder will typically get worse. The bottom line is you want to move the frozen shoulder as much as possible without causing pain.
Warm-Up The Shoulder Before Movement – Use a heating pad, hot shower or bath, or brisk walking to warm up the shoulder before you perform range of motion exercises.
Use a Cold Pack or Ice – after the exercises to control pain and inflammation. Do the exercises 10-15 times each within the limits of pain 3-5 times per day.
Contributions: Gary Mattingly, PT, PhD, Professor, University of Scranton, Department of Physical Therapy, Associate, Mackarey Physical Therapy (deceased).
Read Dr. Mackarey’s Health & Exercise Forum – every Monday – next week: “The Throwing Shoulder”

This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Read all of Dr. Mackarey's Articles at mackareyphysicaltherapy.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.