Like many of you, I have always enjoyed the outdoors...walking, running, biking, hiking etc. However, recently, I have been more concerned about being safe, (getting older and more cautious, distracted drivers) when doing these activities on the side of the road.
Almost 15 percent of all motor vehicle injuries to people happened to those not in cars but while walking, running or hiking, so one needs to be safe. In fact, over 4,000 walkers or runners were fatally hit by a motor vehicle according to the Centers for Disease Control (CDC). These statistics continue to increase as the number of distractions to drivers increases (phone calls, texts, etc). Consequently, walkers, runners and cyclists must be more aware than ever to prevent injury from motor vehicles and stay safe.
Source: http://www.runnersworld.com
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Antibiotic resistance occurs when bacteria no longer respond to the drugs designed to kill them. For more than a decade, the Centers for Disease Control along with other national and international agencies has supported an initiative called “Antibiotic Stewardship” the hallmark of which is the judicious, appropriate use of antimicrobials.
It’s told in some sobering statistics from the CDC, World Health Organization, and Food and Drug Administration:
Patients and providers must take equal responsibility. When we get sick, we often feel we need an antibiotic right away. In fact, we often demand one. A study published in the New England Journal of Medicine in 2018 found that to achieve a patient satisfaction rating in the 90th percentile physicians needed to prescribe antibiotics 75% of the time. Is this the correct approach to therapy? Are we using antibiotics too readily? What are the consequences of profuse antibiotic use?
In which of the following situations are antibiotics warranted?
A. Cold symptoms (runny nose, sore throat, headache) with a fever of 101F for 2 days
B. Cold symptoms lasting 12 days with persistent stuffiness and headache
C. Cold symptoms for 3 days with yellow-green mucous discharge
D. all of the above
The correct answer is B. Let’s discuss the reasons. Symptoms experienced as part of the common cold can include green/yellow sputum, cough, runny nose, stuffiness, sore throat, headache, fever, and mild muscle aches. This illness is caused by a virus, most likely a rhinovirus. Currently, 160 identified strains of rhinovirus are know.
Antibiotics work to destroy bacteria, not viruses since they have no activity against viruses. Antibiotics target specific bacterial structures or functions. Common bacterial targets for antibiotics include the cell wall (amoxicillin), ribosome activity (azithromycin), and bacterial DNA (levofloxacin). All of those are lacking in the very primitive structure of a virus. So, you could sit in a bathtub full of penicillin and not cure your cold with an antibiotic because there is simply nothing for the antibiotic to destroy in the viral structure.
Why are antibiotics appropriate after 10 days with cold symptoms? The typical common cold lasts between five and ten days with symptoms peaking around three or four days and waning at day six. If symptoms are consistent or regress and then become worse it is likely a sign of bacterial superinfections (super = on top of).
Usually, we carry certain bacteria with us as part of our “normal flora”. The mouth, nasal passages, large intestines, and skin host the most bacteria in the body. These bacteria work with our body and provide various “services” including protection against other more dangerous bacteria, digestion of food, and production of vitamins. A viral infection disturbs the normal balance of bacteria, allowing for proliferation and subsequent bacterial infection.
Why should we be careful about antibiotic use?
Antibiotics are not innocuous substances. They have significant side effect profiles. Adverse drug reactions associated with antibiotics can be less severe and consist of mild rash or nausea. More serious reactions include heart arrhythmias, tendon rupture, Stevens Johnson Syndrome (severe skin rash resembling thermal burns), and liver and kidney damage. Remember – every drug – not only antibiotics – has the potential to cause unpredictable adverse reactions
The most compelling reason to be careful about antibiotic use is resistance. Each time bacteria are exposed to an antibiotic, some are destroyed but others adapt to resist the antibiotic and live to see another day (remember Darwin’s Survival of the Fittest?). Antibiotics are unique in that the more they are used, the less effective they become. When antibiotics are used inappropriately – not taking them on schedule, for the right duration, taking them for a viral illness – bacteria have a chance to adapt to overcome the antibiotic activity. The resistant bacteria may go on to set up a resistant infection in you or that bacteria may be transmitted to others.
There are several ways we can combat this problem according to the Joint Commission on Healthcare Accreditation 2020 Standards. It is important to identify the causative agent if possible.
For example, a sore throat should not be treated with antibiotics until a throat culture or rapid strep test is obtained and a bacterial cause is identified. According to the Infectious Disease Society of America, 90 percent of adult sore throats have a viral cause, not bacterial. Avoid unneeded clinic or urgent care visits and utilize OTC and non-drug measures to manage non-bacterial infection symptoms.
Mislabeled allergy status leads to more expensive, less optimal antibiotic choices, more complex administration, increased resistance rates, and more treatment failures. The most common listed drug allergy in the US is Penicillin. According to the CDC, 10% percent of patients reports an allergy, however, < 1% of patients have a true allergy precluding penicillin or penicillin-like agents (the biggest class of antibiotic agents).
Vaccines may prevent bacterial infections or prevent viral infections which will avert a bacterial superinfection. Here are two examples of where vaccines can lower antibiotic use. The pneumococcal “pneumonia” vaccine protects against the bacterium Streptococcus pneumoniae. Following the current guidelines for vaccination during childhood and adulthood decreases pneumococcal infections. According to the CDC, this vaccine has reduced pneumococcal infections by more than 90% in children. In addition, antibiotic-resistant pneumococcal infections have decreased in the United States since the pneumococcal vaccine was introduced.
The shingles vaccine also minimizes antibiotic use. The shingles vaccine “Shingrix”, is currently approved for individuals 50 years old (and older) as a two-dose series. Not only does it effectively prevent the occurrence of shingles, a painful, debilitating re-emergence of the chickenpox virus, but also reduces the risk of a potential secondary bacterial skin superinfection. Vaccine prevention of viral illness may subsequently eliminate antibiotic use.
Educating patients and prescribers will lead to the proper use of antibiotics to curb antibiotic resistance.
Guest Author: Dr. Gretchen Welby, PharmD, MHA
Dr. Welby received degrees from Keystone College and Philadelphia College of Pharmacy and Science. She received a Master of Health Administration Degree from the University of Scranton and a Doctor of Pharmacy degree from Temple University. She is currently the Academic Director of the Physician Assistant Program at Marywood University where she teaches Anatomy, Physiology, Pathophysiology, and Pharmacology.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Ice baths have become a new trend or fad in health and fitness, especially among elite athletes and some celebrities. However, it is far from a new treatment modality. In fact, the Ancient Greeks employed cold-water immersion for fever, pain relief, relaxation and socialization. In addition, Hippocrates documented the use of cold for medicinal purposes for its analgesic benefits.
Ice baths, a type of cryotherapy, is also referred to as cold water immersion (CWI) or cold water therapy. This involves immersing your body in ice water for approximately 5-15 minutes from the neck down at 50-59 degrees. The ice baths are commonly used for pain, delayed-onset muscle soreness (DOMS), and inflammation and mood elevation.
In theory, the cold water lowers the temperature of your skin and body by vasoconstriction (narrow) of the blood vessels. When you get out of the cold, water the vasodilatation (widen) of the blood vessels. Immediately, this brings fresh oxygen and nutrient-rich blood back to the tissues to warm the body and in the process, reduce pain, inflammation and promote healing.
If you have the following health conditions, ice baths may not be the best therapeutic modality for you. Before you consider trying an ice bath, consult with your physician to avoid potentially serious problems:
While some studies have shown that subjects report less muscle soreness following CWI when compared to rest, most studies suggest that the reported effects are placebo. Also, reports of improved circulation, reduced inflammation and improved recovery or performance has not been scientifically validated. In view of this, it is recommended that those considering the use of CWI for pain and inflammation management, reduced muscle soreness, and mood elevation, should consult their physician to determine if the potential risks are worth the purported benefits.
SOURCES: nih; health.com; health.clevelandclinic.org; prevention.com

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
During a recent “lunch-and-learn” meeting at our office, several younger staff members were discussing the use of supplements to compliment their fitness routines. One such staff member, Lily Smith, a physical therapy student aid at our clinic from the University of Scranton, is also a serious weight training and fitness enthusiast and shared her experience with creatine supplements with the hope of educating others, especially those preparing to “get fit” in 2024!
A National Health Interview survey found the creatine use among adolescents and young adults to be 34%. It is also very popular in the military with 27% average usage. While athletes and exercise enthusiasts use protein shakes and creatine supplements with hopes to improve size, strength and performance, it appears that most users do not have a full understanding of the risks and benefits. In view of this, today address the use of creatine in strength training and make recommendations based on the literature.
As long as I can remember, young athletes would take or do anything that they believed would improve their speed, strength, agility and athletic edge in order to succeed in sports. Running with weights wrapped around the ankles, drinking raw eggs and whole milk, and consuming copious amounts of beef, pork, and chicken were not unusual. Today, it may not be much different. However, the products do not come from our kitchen cabinet and tremendous misinformation is associated with it. Creatine is one example that was purported to enhance performance as early as the 1970’s but only gained popularity in the 1990’s. 40% of all college athletes and 50% of professional athletes admit to using creatine at some point, despite a lack of scientific evidence to support its effectiveness or safety.
This supplement is a natural substance that turns into creatine phosphate in the body. Creatine phosphate helps produce adenosine triphosphate (ATP), which provides energy for muscles to contract. While the body produces some creatine, it can also be found in foods rich in protein such as meat and fish. Manufacturers claim that creatine use will improve strength, increase lean muscle mass and aide in the recovery from exercise induced fatigue.
While creatine is popular among young people due in part to its availability, very little research has been done in people under 18 years of age. Even in the few studies conducted on adults, the results regarding efficacy are mixed. Some studies show that creatine may improve strength performance due to the recovery cycle of ATP. In theory, the use of creatine is purported to allow one to recover more quickly from exercise. For example, shortly after lifting heavy weights to failure, a quick recovery might allow the weight lifter to lift an additional set of repetitions to increase the duration of intensive training. Therefore, based on this theory, one must work out to complete failure during training to benefit from creatine. However, it is important to remember, there is no evidence that this purported benefit is realized in performance improvement in weight training or endurance sports.
Furthermore, no studies support the notion that it improves performance in endurance sports. Also, research does show that not all users are affected by creatine the same way. Most users fail to find any benefit at all. More concerning to this author is the fact that there are no guidelines for safety or disclosure of side-effects from long term use. Make no mistake, based on the research and current wisdom, CREATINE IS AN UNPROVEN TREATMENT SUPPLEMENT!
If one decides that creatine is a product they would like to use, despite the lack of evidence for its effectiveness, there are recommendations that one should follow for proper use. But there is no consistently established dose. Some studies have found 25 grams daily for 14 days as a “kickstart” dose or “loading” phase followed by 4-5 grams (or 0.1 g/kg of bodyweight) daily for 18 months with few side effects such as: muscle cramps, dehydration, upset stomach, water retention/bloating with weight gain. It is important to remember when establishing a dosage that many weight training supplements already contain creatine and in high doses excess creatine is excreted by the kidneys. It is also recommended that creatine users “wean off” the product when they decide to discontinue use.
Remember, an average adult in the United States receives 1 to 2 grams of creatine each day from a normal, well-balanced diet. Creatine is naturally found in meat, poultry and fish and theoretically, one could increase their creatine intake through dietary changes. Some manufacturers recommend 10 to 30 grams per day with a maintenance dose of 2 to 5 grams per day for athletic performance. Creatine is available in many forms; tablets, capsules and powder. It should be kept in a cool, dry place out of direct sunlight.
Creatine use is not recommended if you are pregnant, breast feeding, have kidney disease or bipolar disorder. There are many reported side effects associated with creatine use such as; water retention, nausea, diarrhea, cramping, muscle pain and high blood pressure. It is recommended that users consume large quantities of water when taking creatine to prevent dehydration. It may be very dangerous to use creatine when dehydration or weight loss is associated with an activity such as wrestling or summer sessions during football.
Furthermore, some studies show that large amounts of carbohydrates may increase the effects of creatine and caffeine may decrease the effects. Users are warned that using creatine with stimulants such as caffeine and guarana (a Brazilian plant extract similar to caffeine found in energy drinks) can lead to serious cardiac problems. The effects of creatine supplements on the many organ systems of the body are unknown. High doses may cause kidney damage. Although no cases have been reported in the literature, it is not known how it may interact with other supplements, over-the-counter medications and prescription drugs.
In conclusion, despite the lack of scientific evidence that creatine is more effective than proper nutrition and effective weight training, it remains a popular, easily available supplement purported to improve strength, endurance and performance in athletes. While relatively safe if taken as directed, it is always wise to consult your physician, especially if you have a history or risk of kidney problems. And, by the way, Lily did not feel that creatine supplements made any significant difference, positively or negatively. She no longer uses it due to the expense, inconvenience and lack of scientific evidence to support its efficacy.
Sources: University of New England; Medicine & Science in Sports & Exercise; NIH and Lily Smith, PT student, University of Scranton, Student PT aide, Mackarey Physicla Therapy
.Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Studies have shown a recent escalation of joint replacements in a much younger and more active group than previously noted…the baby boomer! While the end result is mostly physical, the cause is often psychological. We all know the personality type: type A, hyperactive, goal-oriented, driven, possessed and highly organized – almost at all costs! Many of you have seen fitness enthusiasts running through the streets at 5:30 AM for 5-10-15 miles each day. Moreover, many of these runners have more activities planned later in the day: golf, tennis, ski, swim, play sports with their kids. Well, after 20 years of this behavior, many of these enthusiasts are now suffering the effects of long term multiple micro traumas. They are suffering from what orthopedic surgeons at the University of Pennsylvania call “Boomeritis! Boomeritis is inflammation of the baby boomer from overuse. Lower back pain, hip, groin, and knee pain is almost a daily event.
As baby boomers continue to enjoy sports with the same vigor and intensity as when they were younger, they are finding that their older bodies just can’t keep up. While these individuals often succeed in finding the balance of fitness and craziness, they have had times when they took it too far. Furthermore, nearly all compulsive exercisers suffer from over training syndrome. When take too far compulsive behavior is rationalized by insisting that if they didn’t work to extreme then their performance would suffer.
*Each sign is worth 1 point:
If you have two or more of the warning sings, consult your family physician to rule out potentially serious problems.
Avoid weight bearing exercises two days in a row. Run one day, walk, swim or bike the next.
Use the elliptical instead of the treadmill.
Avoid squatting…deep squatting is bad for your hips and knees. Even when gardening, use a kneeling pad instead of bending down and squatting.
Visit your family doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles, visit our exercise forum!
Fall is here, cross-country running season has begun and the 26th Steamtown Marathon is only a few weeks away! With that in mind, running injuries, some very specific to women, are on the increase…
While driving to or from work have you noticed more local running enthusiasts in the past few years? Moreover, have your noticed that most of the runners are women? Scranton Running Company has contributed to NEPA’s participation in a national trend; more women are engaged in running than men! Female runners account for 9.7 million runners (57%) while 7 million males run on a national level.
With this surge, the female runner has been subjected to a host of related injuries, including shin splints, which often lead to stress fractures. New research has found that stress fractures may be related to the loss of weight and body mass associated with the sport.
A recent study from Ohio State University found that female runners with a Body Mass Index (BMI) below 19 may have a higher risk of developing stress fractures than women with a BMI of 19 or above. Furthermore, the study also found that these women took longer to recover from these injuries.
According to Timothy Miller, MD, “When body mass index is very low and muscle mass is depleted, there is nowhere for the shock of running to be absorbed other than directly into the bones. Until some muscle mass is developed and BMI is optimized, runners remain at increased risk of developing a stress fracture,”
The study also found that female runners with a BMI of 19 or higher with severe stress fractures required 13 weeks to recover from their injuries and return to running. Runners with a BMI lower than 19, however, took more than 17 weeks to recover.
They concluded that women should know their BMI and consult with a medical professional to maintain a healthy number. Additionally, women should cross-train and include resistance training to improve the strength and muscle mass of the lower extremities to prevent injury.
The current BMI wisdom, according to the National Institutes of Health, is 19.8 for men and 24 for women, however, strong and competitive women tend to have a BMI of 26. A BMI of 18 is considered malnourished.
Body mass index (BMI) is a measure of body fat based on height and weight of adult men and women over 20 years of age, according to the National Institutes of Health.
BMI = (weight in pounds / height in inches squared) X 703)
Example 1: a person who weighs150 pounds and is 68 inches (5 feet 8 inches) tall has a BMI of 22.8
Example 2: a person who weighs 110 pounds and is 66 inches (5 feet 5 inches) tall has a BMI of 17.7
Underweight < 18.5%
Normal weight 18.5 to 24.9%
Overweight 25 to 29.9%
Obesity 30 and over
A stress fracture is fatigue damage to bone with partial or complete disruption of the cortex of the bone from repetitive loading. While standard x-rays may not reveal the problem, a bone scan, and MRI will. It usually occurs in the long bones of the leg, mostly the tibia (shin bone) but also the femur (thigh) and foot. Occasionally, it occurs in the arm.
FEMALE RUNNERS WITH BMI LOWER THAN 19 – is a primary risk factor.
10-21% of all competitive athletes are at risk for stress fractures. Track, cross country and military recruits are at greatest risk. Females are twice as likely as males to have a stress fracture. Other athletes at risk are: sprinters, soccer and basketball players, jumpers, ballet dancers are at risk in the leg and foot. Gymnasts are also vulnerable in the spine while rowers, baseball pitchers, golfers and tennis players can experience the fracture with much less frequency in the ribs & arm.
The problem is much more prevalent in weight bearing repetitive, loading sports in which leanness is emphasized (ballet, cheerleading) or provides an advantage (distance running, gymnastics).
Stress fractures usually begin with a manageable, poorly localized pain with or immediately after activity such as a shin splint. Over time, pain becomes more localized and tender during activity and then progresses to pain with daily activity and at rest.
Source: Ohio State University, Science Daily
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy!
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Paul's Articles, visit our exercise forum!
Farmers and gardeners in NEPA always say that Memorial Day, the “kick off” day for planting without the fear of frost, however, it is not too early to start to prepare…not only the beds but your body! While gardeners are anxious to work in their gardens and enjoy the fruits of their labor, a relaxing and enjoyable activity can turn dangerous quickly. Precautions are necessary as repetitive stress injuries such as shoulder and elbow tendonitis and carpal tunnel syndrome can stem from raking, weeding, digging and pruning. Additionally, simple scrapes, blisters, and bites can turn into serious problems if not treated appropriately. Since prevention is the best approach, the American Society of Hand Therapists (ASHT) promotes warm-up exercises and injury prevention tips to help all levels of gardeners avoid serious and long-term injuries while enjoying this popular outdoor activity.
ASHT recommends following these upper extremity warm-up exercises prior to gardening:
Note: These exercises should never be painful when completing them. You should only feel a gentle stretch. Hold 10 seconds and repeat 5 times. Should you experience pain, please consult a physician or hand therapist.


1. Forward Arm Stretch: Fold your hands together and turn your palms away from your body as you extend your arms forward. You should feel a stretch all the way from your shoulders to your fingers. (PHOTO 1)
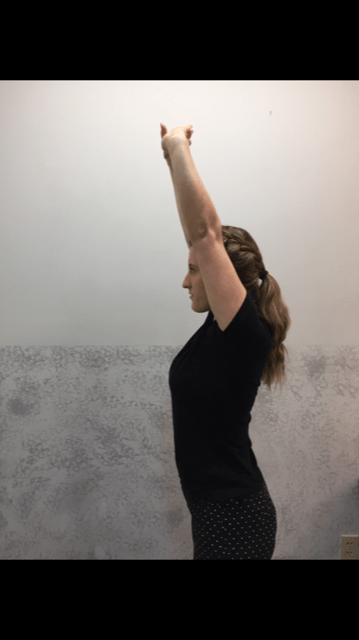
2. Overhead Arm Stretch: Fold your hands together and turn your palms away from your body, but this time extend your arms overhead. You should feel the stretch in your upper torso and shoulders to hand. (PHOTO 2)
3. Crossover Arm Stretch: Place your hand just above the back of the elbow and gently push your elbow across your chest toward the opposite shoulder. This stretch for the upper back and shoulder and should be performed on both sides. (PHOTO 3)
Professional Contributor: Nancy Naughton, OTD, CHT, is an occupational therapist and certified hand therapist practicing in NEPA. Model: Heather Holzman

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” Next Week: “Prevention of Gardening Injuries” Part II of II.
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. Access of all of Dr. Mackarey's articles at our Health and Exercise Forum.