It is two months away from the 25th Steamtown Marathon. This column is dedicated to those dedicated runners preparing for the big day, Sunday, October 9, 2022.
Congratulations and thank you to Bill King, founder and race director, and his band of brothers, for their tireless efforts organizing and sustaining a great race that instills pride for all people of NEPA. It has inspired many people, including me, to transfer the discipline and determination required to complete a marathon by overcoming challenges one mile at a time.
Now, a little marathon history: In 490 B.C. Phedippides, ran 25 miles from Marathon to Athens to deliver an important military message and died immediately. Ironically, the first marathon of the modern Olympic Games in 1896 in Athens was won by Spiridon Louis, a humble Greek peasant, who stopped along the way for a glass of wine and told the owner of the tavern that he would win the race. He was determined to pace himself properly, as he knew the dusty, hilly path better than anyone in the field. He was greeted with jubilation and become a hero and legend.
Visit your doctor regularly and listen to your body.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
For all of Dr. Mackarey's articles visit: www.mackareyphysicaltherapy.com/forum
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
I have a vested interest in this column…I just had a big birthday! It is a BIG birthday because it is the one before I get health care insurance from Uncle Sam! Consequently, the “aging process” is very much on my mind!
In the book, “Being Mortal,” Atul Gawande discusses the role of medical care placing emphasis on “well-being” rather than survival, especially as it relates to end-of-life care. It is a “must read” for health care providers as well as the general public. The book also describes, in great detail, the process of aging; the physiology of bone and muscle mass loss, factors affecting balance and coordination, changes in mental acuity, memory, and mood. As depressing as it sounds (many of the changes begin as early as mid to late thirties), it is also a “call to arms!”
To prepare for the inevitable aging process one must be proactive, not reactive. From an early age, challenge yourself mentally by taking classes and learning things for which you may not have an interest. Try new physical activities and sports even if you feel unable to excel. Find balance in your diet by trying to eat fruits and vegetables that you don’t find appealing. Engage in daily exercise and physical activities even if you would rather be indoors playing video games. Lastly, get professional advice on matters beyond your scope. See your physician regularly for routine care and diagnostic tests, find a mental health professional if you are not at peace, consult with a physical therapist to help you design an exercise routine appropriate for your individual needs.
While it is never too late, remember, slowing down the aging process should not begin at 60, it begins at 30!
Minor word or memory loss is a normal part of aging as the brain changes and affects how you remember things. Don’t hesitate to use technology or other tricks to assist you. For example, consider using alerts, reminders and lists on your smart phone. Also, you may want to organize certain items in a set location, use post it notes or a white board. However, these reminders are not a substitute for keeping your mind sharp. Studies show that being social, exercising regularly, eating well and learning a new skill can go a long way to maintain a healthy brain.
According to several studies on aging, unfortunately, most people gain 1-2 pounds per year (10 to 20 pounds over 10 years). The aging body does not burn calories like you used to. But there are some simple steps you can implement to offset this pattern of weight gain. Obviously, eat less (less calories) and exercise more (stimulate your metabolism). Consider fruits, vegetables, and leaner protein instead of foods high in sugar/carbs and saturated fats and don’t forget portion control. Be active and take the stairs instead of the elevator.
Aging can also affect sexual performance. According to the Mayo Clinic, lower testosterone levels in men can lead to erectile dysfunction and hormonal changes in women can cause vaginal dryness. Stiff and painful joints add to the challenge. However, with a little effort, most healthy people can continue to be sexually active well into their 70’s and 80’s. Communication with your partner is important. Try new positions. Discuss hormone supplements and ED medications with your doctor. Try over-the-counter lubricants. Remember, exercise improves blood flow and stimulates sex hormones!
Like the other muscles in your body, pelvic and bladder muscles also weaken with age. This problem can be worsened for men by an enlarged prostate and for women following multiple births. However, the muscles can be strengthened by performing specific exercises that target the area called Kegel exercises. These exercises involve squeezing the muscles that control urine flow. For example, while urinating try to stop midstream and hold your urine flow for a few seconds. Repeat 10 times and do this 3-5 times a day. Other recommendations include eating foods high in fiber, avoiding carbonated drinks and limiting caffeine.
People often fall into a rigid routine with age. While this predictable pattern often provides comfort, it can also lead to boredom. Try changing your routine or schedule. Learn a new skill (baking, painting, golf) or visit a new place (museums, libraries, community centers). Getting a part-time job or volunteering can be rewarding and stimulating.
There are a number of reasons for one to feel lonely with age…children relocate, loss of a spouse, divorce. Experts say that it is important to take control by initiating contact with others. Call upon neighbors, friends, relatives, and former coworkers to chat or get together. Volunteer for a charity; join a book club or fitness group. Take classes at a local college and consider getting a pet.
Most health problems associated with aging can be treated. Regular checkups and routine diagnostic tests (blood work, colonoscopy, cardiac tests) will assure that health issues do not get out of control. Be sure to organize your medications and take them as directed. Keep a health journal or use and app on your phone to list meds, allergies and record tests and doctor visits.
SOURCES: National Institutes of Health; Mayo Clinic, WebMD

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician.
For further inquires related to this topic email: drpmackarey@msn.com
For all of Dr. Mackarey's articles visit: www.mackareyphysicaltherapy.com/forum
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
I have a vested interest in this column…I just had a big birthday! It is a BIG birthday because it is the one before I get health care insurance from Uncle Sam! Consequently, the “aging process” is very much on my mind!
In the book, “Being Mortal,” Atul Gawande discusses the role of medical care placing emphasis on “well-being” rather than survival, especially as it relates to end-of-life care. It is a “must read” for health care providers as well as the general public. The book also describes, in great detail, the process of aging; the physiology of bone and muscle mass loss, factors affecting balance and coordination, changes in mental acuity, memory, and mood. As depressing as it sounds (many of the changes begin as early as mid to late thirties), it is also a “call to arms!”
To prepare for the inevitable aging process one must be proactive, not reactive. From an early age, challenge yourself mentally by taking classes and learning things for which you may not have an interest. Try new physical activities and sports even if you feel unable to excel. Find balance in your diet by trying to eat fruits and vegetables that you don’t find appealing. Engage in daily exercise and physical activities even if you would rather be indoors playing video games. Lastly, get professional advice on matters beyond your scope. See your physician regularly for routine care and diagnostic tests, find a mental health professional if you are not at peace, consult with a physical therapist to help you design an exercise routine appropriate for your individual needs.
While it is never too late, remember, slowing down the aging process should not begin at 60, it begins at 30!
While aching joints are expected with age, inactivity is not the cure. Controlled movement, exercise and sport modification, supportive devices, and non-prescription supplements and medicines can go a long way.
Controlled movement may include lifting lighter weights or doing squats at ½ or ¾ through your available range of motion. Sport modification includes playing pickle ball instead of tennis or brisk walking or biking instead of running. Supportive devices can be wrist or knee supports or enlarging your racket or golf club grips to lessen the impact on your hands. Over-the-counter treatments include; hot and cold packs, paraffin wax, topical ointments or medications, and nonsteroidal anti-inflammatory drugs (NSAIDs). When all else fails, see a physical therapist for professional advice and treatment and discuss other more aggressive options with your family physician.
Unfortunately, your skin also suffers from the aging process by getting thinner, drier, and less elastic. Avoid the things that can make them worse such as; smoking and ultraviolet rays from the sun or a tanning bed. Protect your skin from the sun, and if you smoke, quit. Consider skin products like moisturizers or prescription retinoids that might make wrinkles less noticeable over time. However, if it is really an issue for you, see a dermatologist.
Aging also makes your skin more vulnerable to drying but there are some things you can do. Use sun screen and wear sun resistant clothing and quitting smoking will go a long way. Drink alcohol in moderation because it can dehydrate you. Also, keep showers or baths to less than 10 minutes and use warm water instead of hot followed by applying oil-based moisturizer.
Loss of strength and endurance is common in seniors. The loss of bone density in women (and men) is also expected. The aging process is only partially responsible. Lack of exercise and activity can also contribute to the problem. Make time to exercise daily (or every other day). Weight training for your arms and legs can be easily performed using light to medium dumbbells or resistance bands. Aerobic exercise can include biking, walking, or swimming, gardening, or swimming for at least 30 minutes a day (or 15-minutes twice a day).
The loss of balance and coordination with age is a serious matter because it can lead to falls that impact long term health and independence. Studies show that those who continue to challenge themselves by riding a bike, dancing, or engage in traditional exercise are much less likely to suffer from early balance problems and are less likely to fall…so get to it! If you can’t do these activities safely, try holding onto your countertop and walk forwards, backwards and sideways, preferably when someone is home with you. See your doctor to be sure that you don’t have a medical condition or taking a medication that contributes to this problem.
Sleep problems are part of aging in many ways; difficulty falling asleep, staying asleep, lack of deep sleep, waking up and not being able to return to sleep, etc. Sleep deprivation can have a negative impact on physical and mental performance. There are some things you can do to improve your sleep such as avoiding coffee and alcohol. Also, try to avoid napping during the day. Talk to your doctor to keep problems that can impact sleeping like high blood pressure or GERD, under control and ask about melatonin supplements.
SOURCES: National Institutes of Health; Mayo Clinic, WebMD

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” Next Week: Part 2 of 2 on Slowing the Aging Process. This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician.
For further inquires related to this topic email: drpmackarey@msn.com
For all of Dr. Mackarey's articles visit: http://www.mackareyphysicaltherapy.com/forum
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
Happy Independence Day! This summer try to think of your pleasure puddle in different light…a health spa! It may very well be the exercise of choice for many people. Many have discovered the benefits of moving their limbs in the warm water of a home pool following knee or shoulder surgery. Also, long distance runners who often look for cross training methods without joint compression and arthritis sufferers who are often limited in exercise choices by joint pain from compressive forces when bearing weight, can enjoy the buoyancy effects of water. These are good examples of the benefits or water exercise…aerobic and resistive exercise without joint compression.
Most doctors recommend some form of exercise with arthritis. Pain and fatigue are the most limiting factors for the person with arthritis. Pool exercise may be the answer. With proper technique, adequate rest periods, appropriate resistance and repetitions, water exercise can be very effective.
Visit your doctor regularly and listen to your body.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit: www.mackareyphysicaltherapy.com/forum
The last two columns in “Health & Exercise Forum” have been dedicated to the health benefits of exercise for Parkinson’s disease. Specifically, the use of dance was featured as a method to promote strength, balance, coordination and agility in this population. However, dance as a form of exercise and for the promotion of balance, coordination and agility, is not limited to those with neurological conditions…it is beneficial for everyone! In fact, my wife, Esther and I, have always enjoyed our dance classes with Vince Brust!
Like most forms of exercise, if done regularly, dance can have multiple health benefits. If dance is your only form of exercise, make it your goal to sustain the activity for about 30 minutes a day, 3-4 days per week for the most value.
If you have any doubt or reservations about the ability of dance to improve your health and wellness, take notice of the muscle tone, flexibility, agility and coordination of a professional dancer...ballet, modern, hip hop, jazz, etc. They are incredible athletes and artists!
It is common to lose agility and flexibility with age especially if you regularly perform the same limited movements throughout your day and lifetime. This will lead to stiffness and lack of flexibility, especially for new or season activities which can make you more vulnerable for injury and pain. Lower back pain and calf or hamstring strains are most common. Research suggests that dance can help.
For example, in one study it was found that cross-country skiers who received months of dance training showed improvements in joint mobility and muscle flexibility of the spine, as well as their speed and agility.
It is also expected that balance and coordination are also compromised with age. It’s one of the reasons that older adults are so prone to falls. The research also supports the value of dance to offset this problem.
One particular study found that in people over the age of 80 years, social dancing helped improve balance and walking speed, as well as contributing to a more stable walking pattern.
Moderate-intensity dance, performed continuously for at least 30 minutes on a regular basis has been found to reduce the risk of death from cardiovascular disease in some studies. Moreover, it has been more effective in prevention than average-pace walking ...and is less boring!
Most activities of daily living (walking, climbing stairs) occur in a linear and forward directon. However, dance has not set direction and can move in multiple planes (forwards, backwards, and sideways with diagonal and rotational components.
These unlimited movements, not only improves agility, coordination, and balance, but also strengthens muscles that often get forgotten like your core and abdominals.
As with any cardiovascular exercise, dance is a form of aerobic exercise which burns calories. This is especially true if performed a minimum of moderate-intensity for 30 minutes or longer.
According to the American Diabetes Association, aerobic exercise can support weight loss.
Weight-bearing exercise is the cornerstone for any osteoporosis prevention program and dance is a prime example.
According to the National Osteoporosis Foundation, high-impact, weight-bearing exercises, such as certain forms of dance, can help maintain bone strength and even build new bone mass. This slows the development and progression of osteoporosis. It is also well established that low-impact weight-bearing exercise (dancing with the impact of jumping etc.) is effective in bone loss prevention. Dance can be whatever intensity you want it to be, depending on your mood, energy level, and physical limitations.
Like most forms of exercise, especially aerobic, dance can improve cognitive health. In addition to releasing special hormones, it can also improve circulation and oxygenation to the brain to enhance brain health.
Some research suggests that dance can help create new connections between brain regions involved in long-term memory and improve mood, cognitive acuity and mental energy.
Physicians and physical therapists often recommend dance as a form of rehabilitation following brain injury, stroke or dementia.
One study found that out of many different types of exercise (including dance, swimming, golf, cycling, tennis, and others) dance was the only one associated with a lower risk of dementia for people in the study. Experts believe the benefit was due to a combo of social interaction and mental focus...that is not to say that the aforementioned types of exercise do not have value.
Dancing can contribute to your mental health by improving mood and reducing stress. As Morrie advised in Mitch Albom’s best-selling book, Tuesdays with Mori, “dance like nobody’s watching”...it can be very invigorating!
Dance participants ranked mood enhancement as the number one reason for participation! One study examining people’s motivation for dancing, “mood enhancement” ranked top on the list. The dancers felt that the activity is expressive and allows you to escape and “let your hair down.”
Some studies also suggest that dance therapy might also reduce depression, especially in those who have serious illnesses, such as breast cancer or Parkinson’s (read last week’s column). Researchers feel that this may be due to increased endorphins and lower cortisol levels.
The pandemic has taught most of us a valuable lesson ... some of us have a serious need to socialize and some do not. For those like me, who thrive on being among others, dance classes and dance-style workouts often take place in groups, which allows for social bonding in a fun, light and breezy environment.
Depending on your marital status and the specific style of dance you choose (salsa, tango or swing dancing), you may even be paired up with a partner every week!
While exercise on treadmill, bike or elliptical can be great exercise, it also can be boring and repetitive. Research suggests that any form of exercise can boost self-esteem.
When dancing, however, you get all the benefits of exercise, while simultaneously learning a new skill. It can be incredibly rewarding and satisfying to master the skill, especially with others such as learning the tango.
SOURCE: “Greatest” Debra Sullivan, Ph.D., MSN, R.N., CNE, COI

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.comPaul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine GCSOM.
For all of Dr. Mackarey's articles visit www.mackareyphysicaltherapy.com/forum
“Dance like nobody’s watching!” This is one of my favorite quotes from Mitch Albom’s book, Tuesdays With Mori, because it represents interesting facts about human behavior. One, of course, is the ability to be comfortable in your own skin. The other, maybe less obvious benefit is that challenging your balance through dancing, even if it’s not pretty, is very effective in maintaining or improving quality of life for those with challenges in gait and balance, as found in Parkinson’s disease (PD). In fact, “Dance for PDR”, a new and popular treatment for PD, has recently been validated in the scientific literature as a valuable treatment tool for those with PD.
Research published in the Journal of Neural Transmission, shows that dancing is shown to help people with PD improve their ability to walk and enhances their quality of life. The program was applicable to those at various stages of PD, including those using walkers. Moreover, the results found that, in addition to physical improvements, participants also had psychological and social benefits through camaraderie, joy of movement and less isolation.
Participants, none of whom had ever engaged in a dance class before, performed a structured dance program for 16 sessions over 8 weeks. Each class was 75 minutes long with seated warm-up activities 50% of the time. Results showed: 10%improvement in overall movement, 26% improvement in walking and 18% improvement in tremor.
Parkinson’s disease is a chronic, degenerative disease that leads to slowness of movement, balance disorders, tremors, and difficulty walking. PD results from the loss of dopamine-producing nerve cells in the brain. Dopamine is critical to stimulate the nerves of the muscular system in the body. PD affects approximately 1.5 million people in the USA with 60,000 new cases each year according to the National Parkinson Foundation. Most people know someone affected by PD. PD typically affects those over 65 years of age and only 15% are under 50.
While there is no current cure for PD, exercise is well documented to relieve some of its symptoms. Specifically, exercise can help keep muscles strong, joints mobile, and tissues flexible. Exercise will not stop PD from progressing, but it will improve balance, enhance walking ability, reduce muscle weakness, and minimize joint stiffness. In 2007, a study published in the Journal of Neuroscience revealed that exercise may benefit individuals with PD because exercise encourages the remaining dopamine cells to work harder to produce more dopamine. Also, the researchers discovered that exercise decreases the rate at which dopamine is removed from the brain.
Exercise to improve strength, balance, and flexibility can be performed independently at home or supervised at a rehab or exercise facility. Supervised exercise can include physical therapy, recreational therapy, water therapy, yoga, and Tai Chi. Physical therapy can improve walking ability, enhance balance, reduce fatigue, increase strength, promote flexibility and minimize pain. Physical therapy uses movement techniques and strategies as well as various pieces of equipment to enhance an individual’s level of independence and improve his quality of life. PT can also incorporate leisure activities (e.g. golfing and ballroom dancing) to reduce the symptoms and associated limitations of PD. Tai Chi, a total mind and body workout, is a series of individual dance-like movements linked together in a continuous flowing sequence. Particular benefits for people with PD include reduced stress, increased energy, improved concentration and focus, better circulation and muscle tone, and significant improvements in balance.
According to Dance for PDR,their programoffers internationally acclaimed dance classes for people with Parkinson’s disease in Brooklyn, New York and, through a network of partners and associates, in more than 120 other communities and 16 countries. In Dance for PD classes, participants are empowered to explore movement and music in ways that are refreshing, enjoyable, stimulating and creative. For more information visit: www.danceforpd.org
So, if you like to dance, “keep on dancing!” If you don’t dance and notice some changes in balance and coordination, or if you have PD…it’s a good time to start! “Dance like nobody’s watching!”

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com. Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit www.mackareyphysicaltherapy.com/forum
Injuries due to falling are a very common problem in the elderly. Hip fractures are the most common injury due to falling in the seniors. According to the American Academy of Orthopaedic Surgeons, each year more than 300,000 people are hospitalized for hip fractures in the United States. These fractures represent 72% of all fracture costs, totaling more than 12 billion dollars in 2005 and, not surprisingly, 90% occurred in those 65 and older. Most hip fracture patients who previously lived independently will require family assistance, home or long term care and 50% will require a cane or walker.
A recent study by the American Physical Therapy Association found that patients benefited from a physical therapy evaluation to determine their risk level for falling. If a high-risk level is found on a falls assessment, physical therapy interventions can be successfully employed to improve strength, balance, and coordination and falls prevention. Also, a well-balanced diet, exercise, Calcium with vitamin D supplements and medications can help prevent or retard osteoporosis and prevent hip fractures.
***Always perform slowly, alternate right and left sides, limit other distractions and concentrate on the exercise to retrain the brain, 10-20 times each 2-3 times per day.
***Caution: Do not do standing exercises without assistance or supervision if needed
Face a countertop and hold onto it with both hands. Hike your hip and knee up to 90 degrees as if you are marching. Hold the position for 3-5 seconds on one leg and lower slowly. Repeat this on the other leg and alternate 10 times.

Face a countertop and hold onto it with both hands. Lift your leg up 30 degrees as if you are spreading your legs apart. Hold the position for 3-5 seconds on one leg and lower slowly to cross over the middle. Repeat this on the other leg and alternate 10 times.
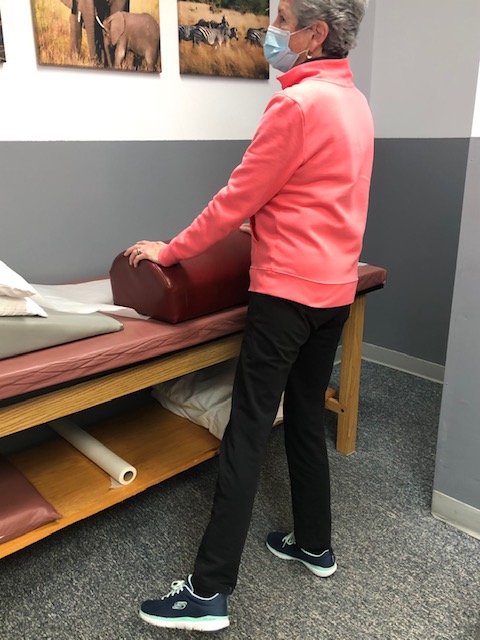
Face a countertop and hold onto it with both hands. Bend your hip and knee down to 45 degrees to a squatting position. Hold the position for 3-5 seconds on both legs and return to standing slowly. Repeat this 10 times. Once strong enough try on one leg at a time and alternate.
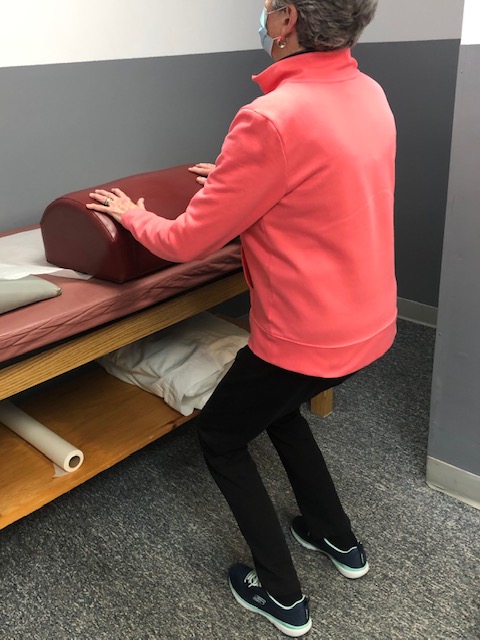
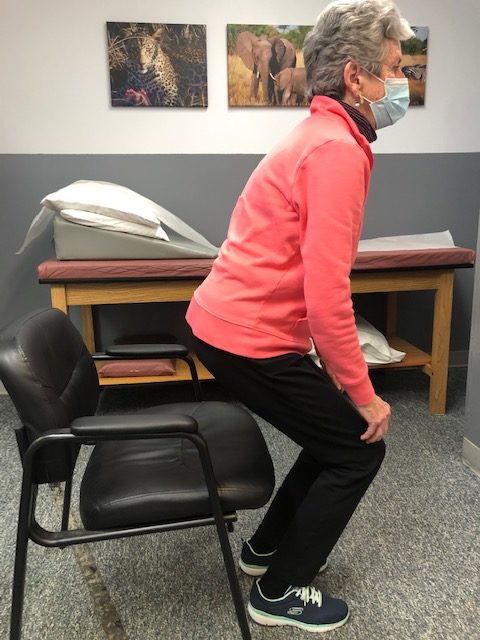
Sit in a chair with arm rests. Get out of chair only using your legs. Hold the position for 3-5 seconds and return to sitting. If necessary, use 1 or 2 arms to assist. Repeat this 10 times. Focus on trunk core stabilization and leg strength. Use more leg muscles and less arm muscles as strength improves.
Place a straight line on the floor and practice “walking the line” with the right then left foot on the line.
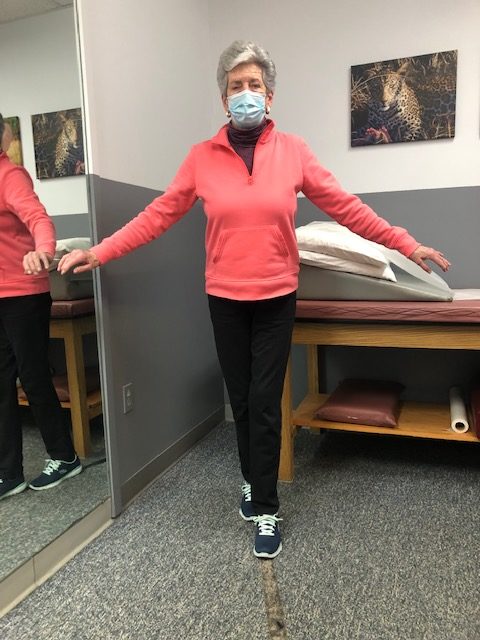
Hold onto a chair while bending one knee and shifting your weight to the other leg. Hold for 3-5 seconds and repeat with the other leg. Increase time 10 -15 -20 seconds as tolerated.

If you feel you or a loved one may be at risk for falling or a hip fracture, ask your family physician if a physical therapy consultation for a falls prevention program to prevent hip fractures may benefit you.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit www.mackareyphysicaltherapy.com/forum
More than 65 million people, almost 30% of the population in the United States, are actively involved in providing 20 or more hours of care for a chronically ill, disabled, or aged family member or friend each week. As our population continues to age, this number is expected to grow rapidly.
The role of a caregiver is multifaceted and often involves tasks and skills beyond the education or comfort level of most providers. Some examples include; managing money, paying bills, shopping, cleaning, maintaining and repairing a home, dispensing and injecting medications, cleaning wounds, changing dressings, catheter management, bed baths, assisting in position changes, transferring from the bed to the chair, ambulation, stair climbing, bathroom assistance for toileting and showering and many other responsibilities. Consequently, a caregiver is often at risk for mental, spiritual and physical fatigue or breakdown. It is no surprise that depression, illness and injury often plague a caregiver and eventually, the caregiver is in need of a caregiver. One of the most common injuries suffered by a caregiver is back pain.
Lower back pain (LBP) is one of the most common problems in our society. Over 90% of all Americans will suffer from it at least once in their lives. It is generally agreed that prevention is the best treatment for LBP.
As little as 10 extra pounds puts great stress on your lower back. It also makes it more difficult to maintain good posture. Eat well and exercise regularly.
Aerobic exercise will help prevent weight gain and stiffness for a healthier lower back. It will also help with the stress and depression associated with providing care for a loved one. Perform mild aerobic exercise such as walking 3-5 times per week for 30-45 minutes. You can also use an elliptical or bike at home while your loved one is resting. Get outdoors and take multiple short walks …go around the block a few times per day.
Core stabilization exercises designed to strengthen the abdominal and lower back muscles will help prevent injury. Some examples of core exercises are:
Pelvic Tilt - lying on your back and performing a pelvic tilt as you flatten you lower back into the floor.
Pelvic Tilt and Heel Slide - lying on your back, hold a pelvic tilt as you slide your one heel up and down and repeat with the other heel.
Core on Ball - Perform arm exercises such as biceps and triceps with light weight while sitting on a therapeutic ball while simultaneously trying to hold an isometric contraction of your abdominal and lower back muscles.
Smoking effects natural healing because it constricts the small blood vessels. Smokers have a much higher incidence of LBP and failure from lower back surgery.
Good posture is critical for a healthy back. When sitting, standing or walking maintain a slight arch in your lower back, keep shoulders back, and head over your shoulders. In sitting, use a towel roll or small pillow in the small of the back.
Caregivers spend much of the day with their spine bent over a bed or chair feeding, bathing, and lifting a loved one. Postural exercises are designed to stretch your back in the opposite direction of this forward flexed position. Examples include:
Bend your knees, maintain an arch in the back with head up, and bend over as little as possible. Bend the knees of your loved one; roll their trunk toward you to get their legs over the edge of the bed as you pivot their weight on their butt to get them sitting upright.
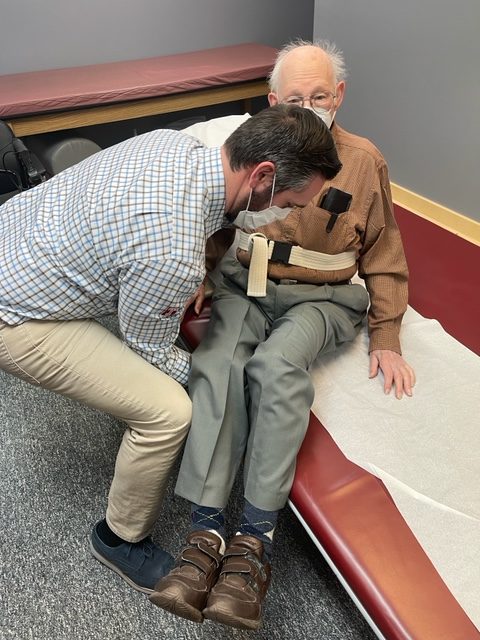
Bend your knees, maintain an arch in the back with head up, and bend over as little as possible. Place your hands around the waist or on a transfer belt. Use your legs, turn with feet, and do not twist spine. Block the feet and knees of your loved-one with your feet and knees and use them to pivot and transfer from the bed to the chair. Be sure the chair is along side of the bed and arm of chair removed if possible before the lift.
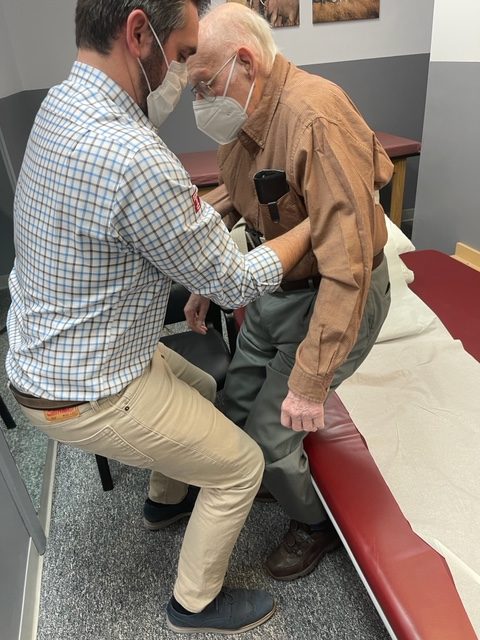
Transfer Belt - Use a transfer belt around the waist of the patient. Grip the transfer belt, instead of the patient or clothing, during the lift or when ambulating. Lower Back Lifting Belt - Also, if you have a back problem, consider using a lifting belt or back brace to protect your back when lifting the patient. Immediately following the lift, stand up straight and stretch lower back into extension.
Transfer belts and lower back lifting belts can be found online or at your local pharmacy.
Lift Chair – For patients that require maximum or moderate assistance and only one caregiver is available to lift or transfer, an electric lift chair should be considered.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice in downtown Scranton and is an associate professor of clinical medicine at GCSOM.
Visit your doctor regularly and listen to your body.
For all of Dr. Mackarey's articles visit: https://mackareyphysicaltherapy.com/forum/
You are never too old to exercise! This is the second of two columns dedicated to appropriate exercise for the elderly. Last week I discussed basic strengthening exercises. This column will address three additional components necessary for independence in the elderly: flexibility, balance and endurance. While it may not be as valuable for those fortunate to be over 75 years of age and capable of running, skiing and playing tennis, you may still find a noteworthy pearl of wisdom.
Why would someone 75 or 80 be interested in a basic exercise program? Well, one must maintain adequate flexibility, strength, balance and endurance to safely function in daily activities around the house. For example, the most common goals of elderly patients are: climbing stairs, getting in and out of a shower, putting on shoes and socks, tucking in a shirt or fastening a bra, cooking, cleaning, and carrying groceries or laundry.
Remember, for most people it is more harmful not to exercise, so contact you physician to discuss whether independent exercise is appropriate for you. You may need to consult with a physical therapist to get started.
Flexibility Exercises involve moving the arms, legs and trunk through comfortable range of motion to give you more mobility in order to improve your ability to perform daily activities such as tucking in a shirt, tying shoes or fastening a bra. Best if performed after strength exercises because the muscles and joints will be warm and limber. Always perform slowly with slight stretch sensation and no pain. No bouncing or over stretching!
These exercises are to be performed while sitting in a chair with a backrest, slowly, 5 repetitions, 3-5 times per week.
Balance Exercises involve strengthening muscles that keep the body upright and stable in standing in order to improve your ability to perform daily activities without falling. According to the NIH, 300,000 US hospital admissions for broken hips occur each year due to falls. Check with your physician if you have a history of dizziness before performing these exercises on your own. Best if performed with someone at home or some assistance. Always use a countertop or back of chair to hold onto for support.
Endurance Exercises involve any activity such as walking, swimming, biking or raking leaves that elevates your heart rate and breathing for an extended period of time. Check with your physician if you have a history of heart problems or dizziness before performing these exercises on your own. Best if performed with someone at home or some assistance. Start off slowly for only 5 minutes and add 1-2 minutes each week or 2. Wear good and comfortable shoes – no heels!
While not all of these endurance exercises may be appropriate for you, one or two of these may offer a good starting point.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate profession of clinical medicine at Geisinger Commonwealth School of Medicine.
For all of Dr. Mackarey's articles visit mackareyphysicaltherapy.com
You are never too old to exercise! A reader who described herself as “elderly” asked me if she was too old to exercise. Without knowing her age, I replied that she was not. I did qualify my response with the fact that exercise must be adjusted to meet the individual needs of a person based on age, health status and goals. Her question, however, led me to think of the many “elderly” who may be apprehensive to begin an exercise program for a variety of reasons. Fear of injury and lack of information may be two reasons. Another reason, according to this inquiry, is the fact that so many exercise programs featured in the media are geared to the young and healthy or baby boomers and few focuses on the needs of those over 75, home bound and weakened by age and inactivity. Those running, biking, skiing, golfing at 75 and over and do not fall into this category, please do not be offended, you are the exception. God bless you!
Why would someone 75 or 80 be interested in an exercise program? Well, one must maintain adequate flexibility, strength, balance and endurance to safely function in daily activities around the house. For example, the most common goals of elderly patients are: climbing stairs, getting in and out of a shower, putting on shoes and socks, walking safely for functional distances, tucking in a shirt or fastening a bra, cooking, cleaning, and carrying groceries or laundry.
The National Institute of Health (NIH) recommends four areas of concentration for elderly persons to concentrate on in order to maintain safety and independence: strength, flexibility, balance and endurance. It will be the purpose of this column to recommend safe, practical and easy exercises that focus on each of these categories.
Remember, for most people it is more harmful not to exercise, so contact your physician to discuss whether independent exercise is appropriate for you. You may need to consult with a physical therapist to get started.
Strength Exercises involve using the muscles to move the arms and legs against resistance such as a weighted object, dumbbells, resistance bands, and body weight against gravity. Strength is necessary to perform daily activities such as walking, lifting a ½ gallon of milk, transferring to a shower or chair safely.
These exercises are performed while sitting in a chair with backrest, slowly, 5 -10 repetitions, and 3-5 times per week. No weight is used in the beginning, only the weight of the arm against gravity. In 1-2 weeks a light 1-2 pound weight and light resistance band may be added.
Once you have mastered these exercises against gravity, then advance to using light weights or light resistance bands. Ankle weights are very inexpensive and can be purchased in 1 pound increments. Light resistance bands are available in yellow and red in colors.
Visit your doctor regularly and listen to your body.
Keep moving, eat healthy foods, exercise regularly, and live long and well!

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” Next Week: Never To Old To Exercise – Part II of II
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate profession of clinical medicine at Geisinger Commonwealth School of Medicine.
For all of Dr. Mackarey's articles visit http://mackareyphysicaltherapy.com/forum