October is National Physical Therapy Month! The American Physical Therapy Association (APTA) would like to recognize the thousands of physical therapists as dedicated health care providers. Moreover, physical therapists would like to thank the public for allowing us to participate in your health and wellness. While PT’s may not save lives…we do save LIFESYLES!
This column will address a question that is frequently asked by people of all ages and activity levels…stretching. First, it is important to keep in mind that stretching should NEVER be performed without warming up your body and muscles first. This can be done by running slowly in place or around the block for 5-10 minutes. Second, stretching should NEVER be painful. Third, a good stretch should be performed slowly and feel like slight tension in the muscle. NEVER bounce or jerk. First, perform the stretches by actively moving your muscles slowly and deliberately 5-10 times. Then, hold the stretch for 5-10 seconds, repeat 5-10 times, 2-4 times per week.
Remember, flexibility is only one aspect of complete health and wellness. Strength training, cardiovascular fitness, meditation and stress management and proper nutrition are also necessary for a healthy lifestyle. Also, be careful not to overstretch before competition as it may weaken the muscle.





MODEL: Sarah Singer, PTA, Mackarey Physical Therapy

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

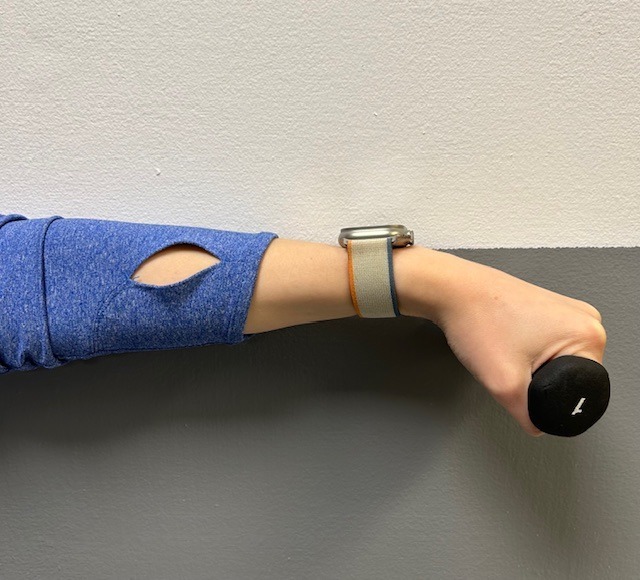
What medical problems do a carpenter, typist, truck driver, jackhammer operator, violinist, pianist and court stenographer have in common? Carpal tunnel syndrome! Over the past 10-15 years, carpal tunnel syndrome has moved to the forefront in medicine and has become water cooler conversation. So, what is carpal tunnel syndrome and how is it treated?
Carpal tunnel syndrome (CTS) is a nerve disorder caused by compression of the median nerve at the wrist. The median nerve is one of three main nerves that provide sensation to the hand. This nerve specifically supplies sensation to the thumb, index, middle, and half of the ring finger. In CTS, compression on the median nerve occurs as it travels through a narrow passage in the wrist called the carpal tunnel. The carpal tunnel is formed by eight bones in the wrist (the floor of the tunnel) and the transverse carpal ligament, a strong ligament traveling across the roof of the tunnel. Within the tunnel there are nine tendons, which are a bit smaller than a pencil. These tendons share this space with the median nerve. In the case where there is swelling on the structures in the carpal tunnel, a person can experience pins and needles, numbness, and aching in the hand.
To be properly diagnosed, a physician will discuss your symptoms and medical history and examine strength and sensation. A nerve conduction study, electromyography (EMG), and x-ray may be ordered to provide information regarding sensation in the median nerve distribution and confirm compression at the carpal tunnel.
Treatment focuses on the causes. Therefore, treatment suggestions may include activity modification and postural changes during activities. Other suggestions may include frequent rest periods, elevation, and exercises or stretching. Wrist splints are effective in relieving compression at the carpal tunnel and are typically recommended for night wear. Appropriate fit of the splint is vital. Occupational and physical therapists or certified hand therapists can check the fit of prefabricated splints or can fabricate a custom splint. The above-mentioned treatments all focus on decreasing inflammation and compression on the median nerve.
Your physician may order pain relievers or anti-inflammatory medication. A cortisone injection into the carpal tunnel may also be recommended to assist with decreasing inflammation near the carpal tunnel.
A referral to an occupational or physical therapist or certified hand therapist may be made. A therapist can provide information regarding the diagnosis, appropriate treatment, and symptom reduction. They can make recommendations to introduce into daily activities to allow appropriate positioning of the upper extremities. A therapist will also instruct individuals on helpful stretching exercises or fabricate a wrist splint. Other treatments include ultrasound, iontophoresis, and massage. The focus of therapy is to introduce changes and interventions that reduce inflammation at the carpal tunnel to assist with symptom relief.
Surgery, referred to as a carpal tunnel release, may be indicated if symptoms are significant and impair functional activity performance.
To reduce your chances of getting CTS:
Guest Contributor: Nancy Naughton, OTD, CHT, is a Doctor of Occupational Therapy and certified hand therapist, specializing in the rehabilitation of the hand and upper extremity at Hand Surgery Associates, Olyphant, PA.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

As most sports enthusiasts know, in 2021 Tiger Woods acquired an Achilles tendon rupture while training at home and in 2023 Aaron Rodgers, a former Green Bay Packer quarterback, did the same in the first game of the 2023/24 NFL season with the New York Jets. As with many sports injuries, it is painful and devastating and best managed by PREVENTION!
Spring is here! Many overjealous fitness enthusiasts will rush to pound the pavement and barely “fit in” a warm-up before participating. But, no matter how limited time is, skipping the warm-up is risky. This time of year, one can expect to feel a little cold and stiff, especially if you are over 40, and therefore a little caution and preparation are in order to avoid muscle/tendon strain, or worse yet, muscle/tendon tears. The Achilles tendon is one of the more common tendons torn. Prevention of muscle tears, including the Achilles tendon includes; gradual introduction to new activities, good overall conditioning, sport specific training, pre-stretch warm-up, stretch, strengthening, proper shoes, clothing, and equipment for the sport and conditions.
This is the second of two columns on Achilles tendon rupture. Last week, I discussed the definition, sign and symptoms of the problem. This week will present examination, treatment and outcomes.
A thorough history and physical exam is the first and best method to assess the extent of the Achilles tendon rupture and/or injury and determine accurate diagnosis. While a complete tear is relatively easy to determine, a partial or incomplete tear is less clear. Ultrasound and MRI are valuable tests in these cases. X-rays are not usually used and will not show tendon damage.
Consultation with an orthopedic or podiatric surgeon will determine the best treatment option for you. When conservative measures fail and for complete Achilles tendon ruptures, surgical intervention is usually considered to be the best option with a lower incidence of re-rupture. Surgery involves reattaching the two torn ends. In some instances, a graft using another tendon is required. A cast or walking boot is used post-operatively for 6-8 weeks followed by physical therapy.
Most people return close to normal activity with proper management. In the competitive athlete or very active individual, surgery offers the best outcome for those with significant or complete tears, to withstand the rigors of sports. Also, an aggressive rehabilitation program will expedite the process and improve the outcome. Walking with full weight on the leg after surgery usually begins at 6 -8 weeks and often requires a heel lift to protect the tendon. Advanced exercises often begin at 12 weeks and running and jumping 5-6 months. While a small bump remains on the tendon at the site of surgery, the tendon is well healed at 6 months and re-injury does not usually occur.
Prevention of muscle and tendon tears is critical for healthy longevity in sports and activities. In addition to the Achilles tendon, the tendons of the quadriceps (knee) and rotator cuff (shoulder) are also vulnerable. A comprehensive prevention program includes; gradual introduction to new activities, good overall conditioning, sport specific training, pre-stretch warm-up, stretch, strengthening, proper shoes, clothing, and equipment for the sport and conditions. Also, utilizing interval training, eccentric exercise (lowering body weight slowly against gravity and proprioceptive and agility drills are essential.
Eccentric Lowering and Lengthening: for the Achillies tendon during exercise. Beginning on the ball of both feet (1a), bend the strong knee to shift the weight onto the weak leg (1b). Slowly lowering the ankle/heel to the ground over 5-6 seconds. Repeat.
Proprioceptive Training: for the Achillies tendon. Standing on a Bosu Ball while exercising the upper body (for example, biceps curls, shrugs, rows, lats) while maintaining balance on the ball.
Agility Drills: for the Achilles tendon involves stepping through a “gait ladder” in various patterns and at various speeds.
Sources: MayoClinic.com;Christopher C Nannini, MD, Northwest Medical Center;Scott H Plantz, MD, Mount Sinai School of Medicine

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Osteochondritis dissecans, also called OCD, is the most common cause of a loose body or fragment in the knee and is usually found in young males between the ages of ten and twenty. While this word sounds like a mouth full, breaking down its Latin derivation to its simplest terms makes it understandable: “osteo” means bone, “chondro” means cartilage, “itis” means inflammation, and “dissecans” means dissect or separate. In OCD, a flap of cartilage with a thin layer of bone separates from the end of the bone. As the flap floats loosely in the joint, it becomes inflamed, painful and disrupts the normal function of the joint.
Typically, OCD is found in the knee joint of active young men who participate in sports which involve jumping or full contact. Although less common, it is also found in other joints such as the elbow.
Often, the exact cause of OCD is unknown. For a variety of reasons, blood flow to the small segment at the end of the bone lessens and the weak tissue breaks away and becomes a source of pain in the joint. Long term, OCD can increase the risk of osteoarthritis in the involved joint.
To properly diagnose OCD a physician will consider onset, related activities, symptoms, medical history, and examine the joint involved for pain, tenderness, loss of strength and limited range of motion. Often, a referral to a specialist such as an orthopedic surgeon for further examination is necessary. Special tests specifically detect a defect in the bone or cartilage of the joint such as:
Radiograph (X-ray) may be performed to assess the bones.
Magnetic Resonance Imaging (MRI) may be performed to assess bones and other soft tissues such as cartilage, ligaments, muscles and tendons.
The primary goal of treatment for OCD is to relieve pain, control swelling, and restore the complete function (strength and range of motion) of the joint. The age of the patient and severity of the injury determine the treatment methods. For example, medications assist with pain and inflammation reduction.
Young patients who are still growing have a good chance of healing with conservative treatment. Rest and physical therapy are the conservative treatments of choice. Rest entails avoiding any activity that compresses the joint such as jumping, running, twisting, squatting, etc. In some cases, using a splint, brace and crutches to protect the joint and eliminate full weight bearing, may be necessary for a few weeks. Physical therapy, either as a conservative or post operative treatment, involves restoring the range of motion with stretching exercises and improving the strength and stability of the joint through strengthening exercises. Modalities for pain and swelling such as heat, cold, electrical stimulation, ultrasound, compression devices assist with treatment depending on the age of the patient and severity of the problem.
Conservative treatment can often require 3 to 6 months to be effective. However, if it fails, arthroscopic surgery stimulates healing or reattaches the loose fragment of cartilage and bone. In some cases if the defect is small, surgery involves filling in the defect with small bundles of cartilage. In other cases, the fragment is reattached directly to the defect using a small screw or bioabsorbable device. More recently, surgeons are using the bone marrow of the patient to repair the deficit by stimulating the growth of new tissue (bone marrow stimulation).
In other cases, a plug of healthy tissue from the non-weight bearing surface of a patient's knee relocated to the defect to stimulate healing (osteochondral autograft transplantation OATS). While there are many surgical options for OCD, an orthopedic surgeon will help the patient decide the most appropriate procedure based on age, size of defect, and other factors.
While prevention is not always possible, some measures can be taken to limit risk. For example, if a child playing sports has a father and older brother who had OCD, then it would be wise to consider the following: Avoid or make modifications for sports requiring constant jumping. Cross-train for a sport to avoid daily trauma (run one day and bike the next). Also, do not play the sport all year round (basketball in the fall/winter and baseball in the spring/summer). Seek the advice from an orthopedic or sports physical therapist to learn proper strength and conditioning techniques. Learn proper biomechanics of lifting, throwing, squatting, running, jumping and landing.
Sources: Mayo Clinic

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

While many people celebrate the Labor Day holiday by firing up the grill, others will be shopping to get their students ready for the school year. One item on the shopping list should be a good quality and well-fitted backpack…to prevent lower back pain!
In 2018, the government of India announced a ban on homework and recently in Poland; the government ministers did the same. Can you imagine…a ban on homework? In an effort to promote student health and address recent surges in the incidence of back pain in the young, there will be no homework for students in grades one and two.
It was estimated that the majority of students ages 7 – 13 in India were carrying almost half their body weight. Not surprisingly, medical practitioners noticed a dramatic increase in reported cases of back pain among this group and decided to take action. In addition to the homework ban for grades one and two, Indian authorities have also implemented a limit of 10% of the student’s body weight.
Back pain in students seems to be universal. Each year, as students in the United States prepare to return to school from summer vacation, the subject of backpacks arises. The good news: when compared to purses, messenger bags, or shoulder bags, backpacks are the best option to prevent lower back pain. The bad news is, most of the 40 million students in the USA using backpacks, are doing so incorrectly.
Studies have found more than 33% of children had LBP that caused them to miss school, visit a doctor, or abstain from activity. Also, 55% of children surveyed carried backpacks heavier than the 10-15% of their body weight, which is the maximum weight recommended by experts. Additionally, the study noted that early onset of LBP leads to greater likelihood of recurrent or chronic problems. Backpacks that are too heavy are particularly harmful to the development of the musculoskeletal system of growing youngsters. It can lead to poor posture that may lead to chronic problems.
The following information on backpack safely is based, in part, by guidelines from The American Physical Therapy Association. Parents and teachers would be wise to observe the following warning signs of an overloaded and unsafe backpack:
Consider the following suggestions to promote backpack safely and prevent back injury:

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Tennis elbow, also called lateral epicondylitis, is an inflammation of the lateral (outside) bony protuberance at the elbow. It is at this protuberance that the tendon of the long muscles of the hand, wrist and forearm attach to the bone. As the muscles repeatedly and forcefully contract, they pull on the bone, causing inflammation. The trauma is irritating when working the muscles in an awkward position with poor leverage like hitting a backhand in tennis.
It is not unusual for a patient to come to my office with severe pain on the outside of their elbow. Especially, after intensifying their tennis workouts or changing the racquet string tension. Others come to me with pain on the inside of the elbow (“golfer’s elbow”) from wrist action that advanced golfer’s use at impact. However, this problem is not only for tennis players and golfers. Laborers working with wrenches or screwdrivers with an awkward or extended arm can also develop tennis elbow. Others who are vulnerable are: those working for hours at a computer using a mouse as well as those working hard maintaining their lawns and gardens.
In a more chronic problem, lateral elbow pain may arise by a degenerative condition of the tendon fibers on the bony prominence at the lateral elbow. Sporadic scar tissue forms from a poor attempt by the body to overcompensate and heal without eliminating the cause.
While symptoms may vary, pain on the outside of the elbow is almost universal. Patients also report severe burning pain that begins slowly and worsens over time when lifting, gripping or using fingers repetitively. In more severe cases, pain can radiate down the forearm.
Conservative treatment is almost always the first option and is successful in 85-90 percent of patients with tennis elbow. Your physician may prescribe anti-inflammatory medication (over the counter or prescribed). Physical/Occupational therapy, rest, ice, and a tennis elbow brace to protect and rest may be advised. Ergonomic changes in equipment, tools, technique and work-station may be necessary. Improvement should occur in 4-6 weeks. If not, a corticosteroid injection may be needed to apply the medication directly to the inflamed area. Physical therapy, range of motion, and stretching exercises may be necessary prior to a gradual return to activity. Deep friction massage can assist healing.

Exercises performed in a particular manner to isometrically hold and eccentrically lengthen the muscle with contraction.
New Conservative Treatment: Platelet-Rich-Plasma (PRP) is a new treatment for the conservative management of degenerated soft tissues that has recently received great media attention. In great part, due to its success in several high profile athletes. According to the Journal of the American Academy of Orthopaedic Surgeons,(JAAOS), platelet-rich plasma (PRP) is autologous (self-donated) blood with an above normal concentration of platelets. Normal blood contains both red and white blood cells, platelets and plasma. Platelets promote the production and revitalization of connective tissue by way of various growth factors on both a chemical and cellular level.
The actual PRP injection requires the patient to donate a small amount of their own blood. The blood is placed into a centrifuge (a machine that spins the blood at a high velocity to separate the different components of blood such as plasma, white and red blood cells), for approximately 15 minutes. Once separated, the physician draws the platelet-rich plasma to be injected directly into the damaged tissue. In theory, the high concentration of platelets, with its inherent ability to stimulate growth and regeneration of connective tissue, will promote and expedite healing.
Surgery for tennis elbow is only considered in patients with severe pain for longer than 6 months without improvement from conservative treatment. One surgical technique involves removing the degenerated portion of the tendon and reattaching the healthy tendon to bone. Recently, arthroscopic surgery developed to perform this technique. However, research does not support the value of one over the other at this point. Physical/occupational therapy is used after surgery. Return to work or athletics may require 4-6 months. More recently, a surgical technique using ultrasound to guide a needle to debride (clean) the area of scar tissue has been developed. If eligible for this procedure, the time required for healing, rehabilitation and return to activity is much shorter.
If you feel you suffer from tennis elbow, ask your family physician which of these treatment options are best for you.
Visit your doctor regularly and listen to your body.
EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy

This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
I have been advising my patients to exercise, keep active, and walk as long as they can in order to stay mobile and healthy. However, seniors often tell me activities that require prolonged walking is limited by ankle pain from arthritis. They often ask, “What is arthritis of the ankle?” How does it happen? What can I do about it?
Your family physician will examine your ankle to determine if you have arthritis. In more advanced cases you may be referred to a specialist such as a podiatrist, orthopaedic surgeon or rheumatologist for further examination and treatment. X-rays will show if the joint space between the bones in the ankle is getting narrow from wear and tear arthritis. If rheumatoid arthritis is suspected, blood tests and an MRI may be ordered. The diagnosis will determine if you problem if minor, moderate or severe.
In the early stages your treatment will be a conservative, nonsurgical approach, which may include; anti-inflammatory medication, orthopedic physical therapy, exercise, activity modifications, supplements, bracing, etc. You and your family physician, podiatrist, orthopedic surgeon or rheumatologist will decide which choices are best.
When conservative measures no longer succeed in controlling pain and deformity, improving strength and function then more aggressive treatment may be necessary.
SOURCES: Rothman Institute, Philadelphia, PA and American Academy of Orthopaedic Surgeons
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
June is migraine and headache awareness month! According to the World Health Organization about half of the world’s adult population has had a headache at least once in the past year. Prolonged use of electronic devices has greatly contributed to this problem. For many people, these headaches are infrequent and do not often affect daily life. But what about when your headache occurs frequently or is so severe it prevents you from going about your day to day activities? Some types of headaches are more easily treated and managed than others.
There are two types of headaches: primary and secondary. Primary headaches occur without an underlying disease and include migraines and tension-type headaches. Secondary headaches can be associated with serious disease, requiring emergency care, or can be referred from other structures of the body such as the cervical spine (neck).
Headaches symptoms that may constitute a medical emergency are: vomiting, seizures, fever, muscle pain, night sweat, weight loss, and neurologic symptoms such as blurred vision. If you are experiencing any of these symptoms, if your headache worsens, or your symptoms change it is recommended that you seek medical attention. Any headache that is unusual for you and does not resolve itself in a reasonable time should be brought to your primary care physician’s attention.
Migraines: Migraines are a primary form of headache that typically lasts from four to seventy two hours, can range from moderate to severe pain, and typically are located on only one side of the head. Often they can be accompanied by an aura, nausea or vomiting, sensitivity to sound, or light sensitivity. Migraines can be aggravated by routine physical activity such as going up stairs. This type of headache is thought to occur in the central nervous system.
Tension-type: Tension-type headaches are the most common primary headache disorder and can last anywhere from thirty minutes to seven days. These can often have a pressing or tightening quality that occurs on both sides of the head. Typically, there is no nausea, vomiting, or aggravation with physical activity, however, light or sound sensitivity can occur. This type of headache is thought to occur in the central nervous system but can have a hereditary component and is usually associated with muscle tender points. Tension – type headaches can be treated with relaxation techniques such as Progressive Muscle Relaxation (PMR), medications, and physical therapy.
The most common secondary headache that is not related to a serious medical condition is a cervicogenic headache (originating from the neck).
Cervicogenic Headache: The length of time a cervicogenic headache can last varies. Here the pain is on one side and usually starts in the neck. This type of headache is aggravated or preceded by head postures or movements of the neck. Due to the nerves of the neck and face sharing common connections, pain signals sent from one region can lead to discomfort in the other. Physical therapy can be an effective treatment to help relieve symptoms. For example: posture, exercise, ergonomics, massage, manual techniques, traction, trigger point, and acupressure.
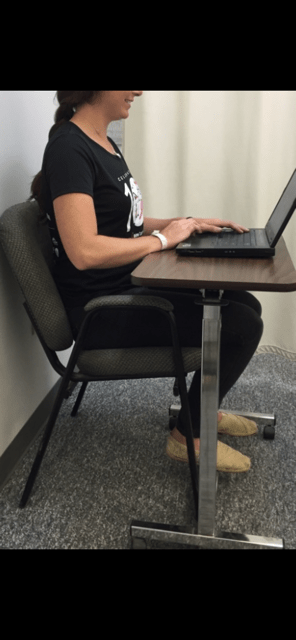
A cervicogenic headache can be caused by an accident or trauma or can stem from neck movement or sustained postures. Sustained postures could mean sitting in front of a computer at work or looking down at your phone. Changing these postures throughout the day could help reduce symptoms. Changing postures could mean bringing your phone closer to you using pillows or another supportive surface when reading or checking social media. If you are someone who works at a desk, it could involve taking breaks or getting a standing desk. However your life requires you to move, there are some simple and effective exercises you can perform throughout the day to help cervicogenic headache symptoms.
Progressive Muscle Relaxation: PMR is an effective method for reducing tension throughout the body. With this method you first tense a muscle group, such as at the neck or shoulder, and then relax the muscles noting the difference between the two. This helps reduce both stress and tension. For more information or to learn how to do PMR, refer to podcast at: https://www.psychologies.co.uk/try-progressive-muscle-relaxation
Manage your stress level: While stressors vary from person to person, one method for managing stress is with exercise. Any form of exercise can help reduce stress, but a cost free method is aerobic exercise such as walking or running. A less time consuming method could be to perform deep breathing exercises throughout the day.
Heat or cold: When feeling sore or stiff, applying a hot or cold pack or taking a hot shower can help ease a tension headache.
Posture: Some tips for posture are to make sure your head is over your shoulders rather than sitting forward and making sure you are sitting or standing up straight with your shoulders back.
Over the counter medications: Talk to your doctor or pharmacist for additional information.
Posture: See tips listed under tension headaches.
Ergonomics: If your job or hobbies require you to sit for extended periods it may be beneficial to change positions throughout the day or consider getting a standing desk. Also, limit time on electronic devices. When sitting make sure the monitor is at eye level, your legs are able to fit under your desk, and you are close to the keyboard and monitor. If you are working with a laptop or phone, avoid putting it on your lap. Instead, bring your laptop closer to you by putting pillows on your lap or using an ergonomic desktop. See photo below.
Exercise: Some exercises to help relieve symptoms are chin tucks, shoulder blade pinches, and back extension. These exercises can be performed multiple times throughout the day in sitting or standing.
Physical Therapy: Physical therapy may include massage, manual techniques, stretching, traction/ decompression and exercise. A physical therapist can assess your posture and provide strategies specific to you.
Over the counter medications: While medication may not cure cervicogenic headaches, they may help relieve pain. Talk to your doctor or pharmacist for additional information.
Visit your doctor regularly and listen to your body.

Dr. Chua is a neurologist and headache specialist at Geisinger Health System in Northeast Pennsylvania. In addition to caring for people with headache and facial pain disorders, Dr. Chua also serves as: Director of Headache Medicine at Geisinger, Clinical Director of Neurology at Geisinger Wyoming Valley, faculty at Thomas Jefferson University’s Advanced Headache Diagnosis and Management Post-Graduate Certificate Program, and Treasurer and Executive Board Member of the Association of Migraine Disorders. In her spare time, she enjoys going on adventures with her husband and toddler, learning new skills (she is now certified in battlefield acupuncture), and buying great books she will never have time to read!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
This column is dedicated to the memory of John R. O’Brien, Esq., who recently passed due to medical complications associated with multiple sclerosis (MS). John was a source of joy and inspiration for those fortunate to have known him. Twenty years ago, John hesitantly agreed to contribute to my column on MS with two requirements: one, if the column would be valuable to those affected by MS and two, he would remain anonymous. When speaking with his dedicated wife, Sally, it became very apparent that any discussion of John’s life would be diminished if it was defined by the disease because he was committed to turning his “DISABILITY INTO AN ABILITY!”
With the help of his loving wife, family, friends, and devices such as an electric scooter and adaptive car, John not only lived but thrived! He was a skilled lawyer, a respected member of the Bar, and an active member of the community. John served on the executive committee of the Lackawanna Bar Association. In addition, the Lackawanna Pro Bono honored him recently. He also taught business law and healthcare law and coached Prep’s mock trial team.
John shared his thoughts with me about the challenges of redefining life… from Golf Club Champion to living with a physically disabling disease. Anyone who knew him would agree that he succeeded in doing so through his keen intellect and sharp wit and humor…his heart and brain overcompensated for his body! In addition to reading books in Latin and Greek, he had his crossword puzzles published in The New York Times and Los Angeles Times. In September 2023, John conducted an interview with presidential historian Doris Kearns Goodwin before a full house at the Scranton Cultural Center. Ms. Goodwin later reported that John was the most knowledgeable, effective and enjoyable interviewer she’s encountered.
John’s absence will be deeply felt and his legacy will continue to shape our community for years to come!
Multiple Sclerosis is a chronic disease. While it may lay dormant and stable for a period of time, living a healthy lifestyle will make a positive contribution toward how you and your family live with Multiple Sclerosis. Studies show that a life of family, love, and support are essential to maintain a positive attitude with a chronic illness. This combined with a healthy diet and proper exercise can contribute greatly toward taking control and living a relatively normal life with MS.
As I have mentioned in many other columns, studies show that people with good attitudes and great faith live longer than others. This is especially helpful when living with chronic disease like Multiple Sclerosis. The Cleveland Clinic offers some suggestions how to maintain a positive attitude:
Many sources, including the Cleveland Clinic suggest that exercise, when performed properly, can have a positive impact on Multiple Sclerosis symptoms both physically and psychologically. However, because you have a chronic illness, you should consult with you family physician and physical therapist before beginning an exercise program. They will advise you on the proper type and amount of exercise.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
This column is dedicated to the memory of John R. O’Brien, Esq., who recently passed due to medical complications associated with multiple sclerosis (MS). John was a source of joy and inspiration for those fortunate to have known him. Twenty years ago, John hesitantly agreed to contribute to my column on MS with two requirements: one, if the column would be valuable to those affected by MS and two, he would remain anonymous. When speaking with his dedicated wife, Sally, it became very apparent that any discussion of John’s life would be diminished if it was defined by the disease because he was committed to turning his “DISABILITY INTO AN ABILITY!”
With the help of his loving wife, family, friends, and devices such as an electric scooter and adaptive car, John not only lived but thrived! He was a skilled lawyer, a respected member of the Bar, and an active member of the community. John served on the executive committee of the Lackawanna Bar Association and was recently honored by the Lackawanna Pro Bono. He also taught business law and healthcare law and coached Prep’s mock trial team.
John shared his thoughts with me about the challenges of redefining life… from Golf Club Champion to living with a physically disabling disease. Anyone who knew him would agree that he succeeded in doing so through his keen intellect and sharp wit and humor…his heart and brain overcompensated for his body! In addition to reading books in Latin and Greek, he had his crossword puzzles published in The New York Times and Los Angeles Times. In September 2023, John conducted an interview with presidential historian Doris Kearns Goodwin before a full house at the Scranton Cultural Center. Ms. Goodwin later reported that John was the most knowledgeable, effective and enjoyable interviewer she’s encountered.
John’s absence will be deeply felt and his legacy will continue to shape our community for years to come!
According to the National Multiple Sclerosis Society, Multiple Sclerosis affects approximately 400,000 people in the United States. Multiple Sclerosis is second only to trauma as the most common cause of neurological disability for those in early to middle adulthood. MS is almost three times as common in women. Multiple Sclerosis is very uncommon before adolescence or after 50. However, the risk increases from teen years to age 50.
Multiple sclerosis is considered to be an autoimmune disease. The immune system of the body does not work properly when it fails to attack and protect the body against substances foreign to the body such as bacteria. Instead, the system allows the body to attack normal tissues and create diseases such as MS, rheumatoid arthritis and lupus.
In MS, the immune system attacks the brain and spinal cord of the central nervous system. Each nerve has an outer covering of a fatty material (myelin) for insulation to improve the transmission and conductivity of impulses or messages to and from the brain. The damage to the myelin of the nervous system interrupts the ability of messages to travel to and from the brain, through the spinal cord and to other areas of the body such as the muscles in the arms and legs. Due to this “short circuiting” the brain becomes unable to send or receive messages. In multiple sclerosis, scar tissue or plaques (sclerosis) replaces the fatty myelin in “multiple” areas. This is also called demyelination.
The symptoms associated with MS vary greatly from person to person. The amount, frequency and speed of the demyelination process vary greatly and are directly related to the loss of strength and function in daily activities. Some people are independent and ambulatory with mild and infrequent episodes of weakness and disability and live a relatively normal life. Others suffer from frequent and aggressive episodes that significantly weaken and disable. Some common symptoms in the early stages include: muscle weakness, loss of coordination, blurred vision, pain in the eyes, double vision. Some common symptoms as the disease progresses are: muscle stiffness with muscle spasms, pain, difficulty controlling urination, difficulty thinking clearly.
The diagnosis of MS can be very difficulty in the early stages because the symptoms are often vague and temporary. Also, MS symptoms are very similar to other neurological problems. A neurologist will run several tests to rule out other possible problems. However, an MRI showing demyelination of the nerves is a primary confirmation.
Treatment for MS depends upon many factors and requires consultation with your physician. Some medications can control the frequency and severity of MS symptoms such as pain, weakness, and spasticity. Also, some drugs can slow the progression of certain types of MS. Additional treatments for MS include: diet, exercise, physical therapy, support groups, and counseling for the MS patient and their family. Part II of Multiple Sclerosis will discuss these options in further detail next week.
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy - NEXT WEEK: PART II OF II - MULTIPLE SCLEROSIS
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!