I wish I could tell you that after turning 50, there are health issues associated with age I plan to be mindful of and address proactively. Unfortunately, that ship has sailed for me well more than a decade ago. So, I share this medical information, not only as a health professional but also as an experienced senior.
Entering the fifth decade is not all dome and gloom. Often, this decade is associated with an established family, gratifying career, good health and acquired self-confidence…realizing that life does not have to be perfect to be wonderful!
However, research tells us that as the body ages, even small changes at the cellular level can be manifested into big changes and problems over time. Nine of ten older adults have some type of chronic disease and eight of ten have more than one. But the good news is that, with a modicum of effort, most of these illnesses can be controlled or prevented, including regular doctor visits, health screening and testing, and lifestyle changes.
While it is normal to experience some weight gain is expected with age. However, uncontrolled, the average person will gain 1-2 pounds per year, leading to 11 pounds per decade, according to the National Institutes of Health. Consequently, almost 45% of Americans between 40 to 60 are obese. Obesity is associated with at least 20 chronic illnesses such as high blood pressure, heart disease, diabetes, cancer, and arthritis.
SCREEN: Body Mass Index (BMI)
TREATMENT: Diet, Exercise, Lifestyle, Medications, Surgery
With age, the flexibility of blood vessels loses elasticity and, unchecked, two out of three adults over 60 have high blood pressure. While genetics is a factor, there are a few things that you can control such as diet (salt, calories), exercise, weight, stress, and smoking.
SCREEN: Blood Pressure Test, Lab Tests, Electrocardiogram (ECG/EKG)
TREATMENT: Diet, Exercise, Lifestyle, Medications
Plaque buildup in the arteries of the heart begins in childhood and advances rapidly with age. 6-7 percent of US adults between the ages of 40 and 60. 20% of men and almost 10% of women between the ages of 60 and 80 have heart disease.
SCREEN: Blood Pressure, Cholesterol testing, Blood Sugar Testing, Imaging (ECG/MRI)
TREATMENT: Diet, Exercise, Lifestyle, Medications, Surgery
10 % of Americans have diabetes and the percent only increases with age. Diabetes is associated with many serious chronic illnesses such as heart disease, blindness, kidney disease and others.
SCREEN: Blood Test for blood sugar levels such as A1C, fasting plasma glucose test and random plasma glucose test
TREATMENT: Diet, Exercise, Lifestyle, Medications
In many cases osteoarthritis (wear and tear of joints) is often associated with age. However, lifestyle, joint injuries, inactivity, obesity and diabetes play a significant role.
SCREEN: Physical Exam, Functional Scores, Xrays, MRI, CT, US
TREATMENT: Diet, Exercise, Physical Therapy, Lifestyle, Medications (NSAID’s, Steroids, Viscosupplementation), Bracing, Surgery
Loss of bone density and strength is associated with age and certain metabolic conditions such as early menopause, thyroid disease, prolonged use of blood thinners and steroids. However, a diet rich in vitamin D, regular weight bearing exercises such as walking, jogging, dancing etc can go a long way.
SCREEN: Fracture Risk Assessment Tool (FRAX), Dual-Energy X-Ray Absorptiometry (DEXA) TREATMENT: Diet, Exercise, Physical Therapy, Lifestyle, Medications (Oral and Injection)
Losing balance with age is a common problem due to changes in the vestibular system (balance system in the brain), loss of muscle strength and joint flexibility, and compromised vision and hearing. This can often lead to falls, head injuries and fractures.
SCREEN: Timed Up and Go (TUG) Test, Morse Fall Scale
TREATMENT: Physical Therapy – Falls Prevention Program/Balance Training , Diet, Exercise, Lifestyle, Environmental Modification, Vision/Hearing Testing
Almost 10% of adults between the ages of 55 and 65 have some form of vision and/or hearing loss. This can lead to many problems such as balance and falls as well as isolation and depression.
SCREEN: Regular Hearing Tests/Vision Testing
TREATMENT: Corrective Devices
Both men and women suffer from bladder problems with age... especially frequency and control. It can impact lifestyles in many ways. Often adults fail to hydrate properly, especially when traveling, to control urgency. This can lead to other health problems.
SCREEN: Urine Analysis, PSA, Imaging, CT Urogram, Urine Cystoscopy, Ultrasound,
TREATMENT: Diet, Exercise, Lifestyle, Avoid Caffeine and heavy lifting, Medications, Surgery
As the body ages, so too do the cells that make it up. Often these cells change into cancer different parts of the body. Skin, colon, breast, prostate, lung, throat, etc. Today, however, much progress has been made for early detection and treatment.
SCREEN: Physical Exam (Skin Exams), Lab Tests (blood work, PSA), Imaging (CT, Mammography, MRI), Genetic Testing, Pap Smears, HPV Tests, Colonoscopies/Stool Tests, Multi-Cancer Early Detection (MCED)
TREATMENT: Diet, Exercise, Physical Therapy, Lifestyle, Medications, Chemotherapy, Radiation, Immunotherapy and Targeted Therapy Surgery specific to the cancer type.
Age related mental health issues are vastly unreported and diagnosed. Medical problems can contribute to mental health such as high blood sugar levels and some infections. Overall, lifestyle, environmental factors and family structure and support are particularly important.
SCREEN: No Single Test – Combination of Tools including - Neurological and Cognitive Tests, Brain Scans (CT/MRI), Blood tests, Genetic Testing
TREATMENT: Diet, Exercise, Physical Therapy, Lifestyle, (avoid excessive toxins like alcohol and nicotine), Medications, Environmental Modifications.
SOURCES: WebMD, NIH, Mayo Clinic, Alzheimer’s Association, American Cancer Society, American Heart Association, American Diabetes Association

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

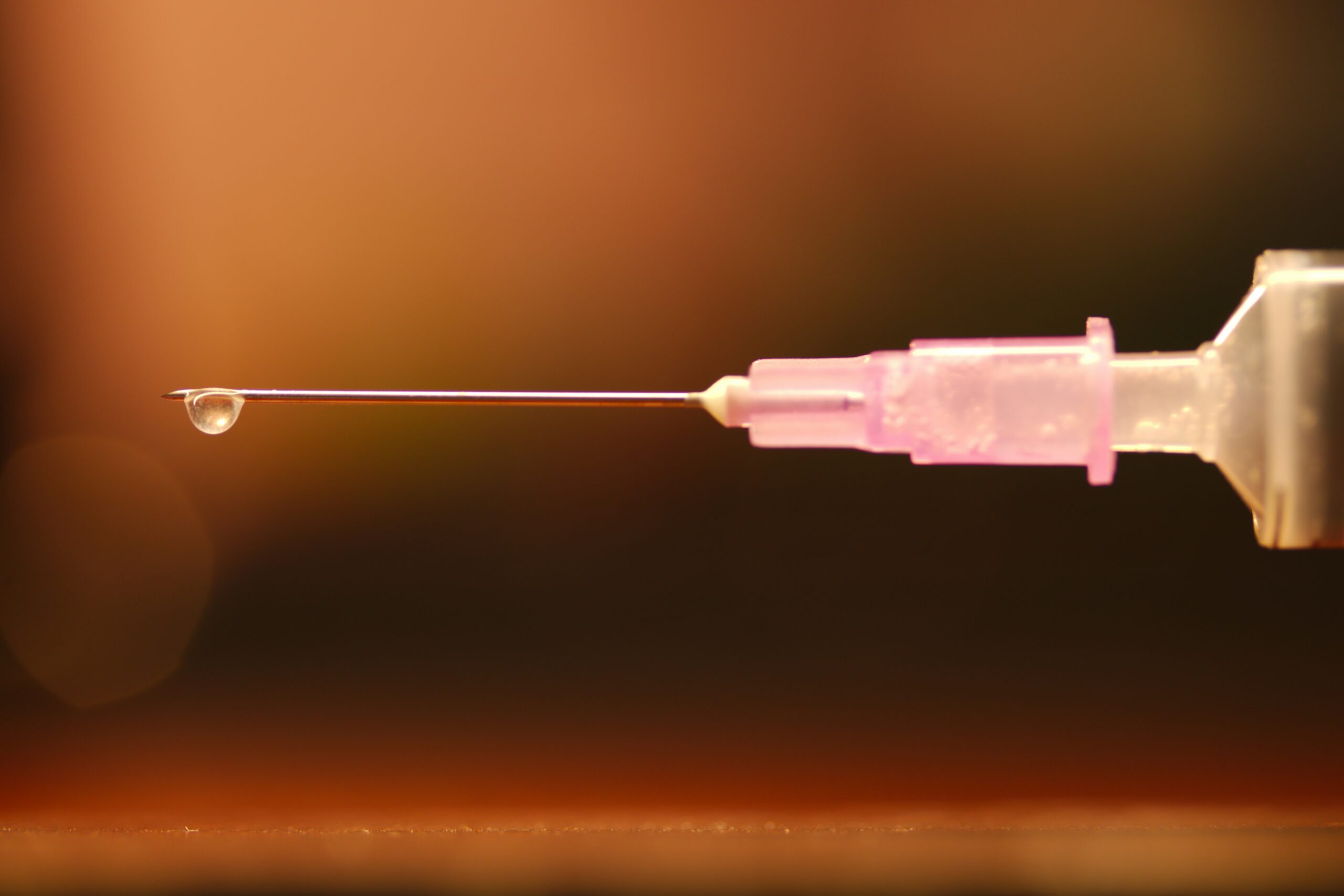
At least once a week, a patient jokingly asks if they can get a “lube job” to loosen up their stiff knee joint. I respond by providing them with information about osteoarthritis and viscosupplementation, a conservative treatment administered by injection and approved by the FDA for the treatment of osteoarthritis of the knee.
Osteoarthritis (OA) is also known as degenerative arthritis. It is the most common form of arthritis in the knee. OA is usually a gradual, slow and progressive process of “wear and tear” to the cartilage in the knee joint which eventually wears down to the bony joint surface. It is most often found in middle-aged and older people and in weight bearing joints such as the hip, knee and ankle. Symptoms include: pain, swelling, stiffness, weakness and loss of function.
Your family physician will examine your knee to determine if you have arthritis. In more advanced cases you may be referred to an orthopedic surgeon or rheumatologist for further examination and treatment. It will then be determined if you are a candidate for viscosupplementation. While this procedure is the most commonly used in the knee, it has also been used for osteoarthritis in the hip, shoulder and ankle.
Viscosupplementation is a procedure, usually performed by an orthopedic surgeon or rheumatologist, in which medication injected into the knee joint acts like a lubricant.
The medication is hyaluronic acid is a natural substance that normally lubricates the knee. This natural lubricant allows the knee to move smoothly and absorbs shock. People with osteoarthritis have less hyaluronic acid in their knee joints. Injections of hyaluronic acid substances into the joint have been found to decrease pain, improve range of motion and function in people with osteoarthritis of the knee.
When conservative measures, such as anti-inflammatory drugs, physical therapy, steroid injections fail to provide long lasting relief, viscosupplementation may be a viable option. Often, physical therapy and exercise are more effective following this injection to provide additional long-term benefit. Unfortunately, if conservative measures, including viscosupplementation fails, surgery, including a joint replacement may be the next alternative.
In 1997 the FDA approved viscosupplementation for osteoarthritis of the knee. Presently, there are several products on the market. One type is a natural product made from the comb of a rooster. However, if you are allergic to eggs or poultry products or feathers, you should not use the natural product. The other medication is best used for patients with allergies because it is manufactured as a synthetic product.
The long-term effects of viscosupplementation is much greater when other conservative measures are employed:
SOURCES: Genzyme Co, Sanofi-Synthelabo Inc, Seikagaku Co. and American Academy of Orthopaedic Surgeons
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Patients often tell me that they would like to exercise but hesitate due to their knee or hip pain. They want to know what type of exercise is best for those suffering from osteoarthritis (OA). Osteoarthritis is also known as degenerative arthritis. It is the most common form of arthritis in the knee. It is usually a gradual, slow and progressive process of “wear and tear” to the cartilage in the joint which eventually wears down to the bony joint surface. It is most often found in middle-aged and older people and in weight bearing joints such as the hip, knee and ankle. It causes gradual onset of pain, swelling and stiffness in the involved joint, especially after increased activity and weakness with loss of function due to disuse.
However, OA is not an excuse to avoid exercise but it is important to be smart about it. Regular exercise is essential to maintain a normal lifestyle for those with OA. However, if you do the wrong exercise, use poor technique, or are too aggressive, you could flare-up your joints and do more harm than good.
When performed correctly, exercise for those with OA has many benefits:
Pain Control
Exercise controls OA pain by releasing natural pain control chemicals in the body called endorphins. It also controls pain by assisting in weight loss and improving range of motion.
Weight Control
We all know how well exercise burns calories and that increased body weight creates increase stress on the joints.
Prevention of Joint Stiffness
Exercise will help maintain joint range of motion. A stiff joint is a painful joint.
Prevention of Muscle Weakness
Exercise will help maintain muscle strength. Weak muscles will allow or increase in joint wear and tear.
Maintain Lifestyle
If a joint is stiff and weak, then they become painful which negatively impacts your lifestyle. Exercise can prevent this problem.
Start Slowly
Wean into exercise because if you advance too quickly, you will flare up the joint and have increased pain. For example, walk for 5-10 minutes the first session. If you do not have pain, add 1-2 minutes each session.
Lose Weight
Every pound lost equates to less stress on your joints. For example, a loss of 5 pounds of body weight translates to 20-30 pounds of stress through the knee, according to David Borenstein, MD, President of the American College of Rheumatology. Also, body weight has a direct impact on daily activities. For example, walking upstairs creates stress through the knee equal to 4 times body weight and seven times body weight going downstairs. Therefore, less body weight equals less stress.
Low Impact Workouts
Low impact exercise creates less stress on the joints while strengthening leg muscles and those who those who maintain leg muscle strength have less stress on their joints. It is even important not to load your arms with heavy objects when walking or using stairs to limit joint stress.
Some examples of low-impact exercises are: walking, swimming, elliptical trainer, and biking. Strength training is also low-impact and should be performed with low weight and high repetitions. Water therapy is great for those with OA, especially in a heated pool. It is a great low-impact exercise with less gravity and stress on the joints. Walk, swim and do mild resistance exercises in the water. Use a snorkel and mask for swimming to limit excessive neck turning and back extension.
Walking is a great form of exercise; however, walking softly is important for those with OA. Wear good running shoes and orthotics if necessary. Discuss this with your physical therapist or podiatrist. When possible, use soft surfaces like cinder, mulch or rubber. Avoid grass and soft stand due to instability and torsion that may irritate your joints.
Warm-Up
Warming up your body is critical to prevent injury to the muscles and tendons. This can be done by marching in place or using aerobic equipment such as a bike for 5 to 10 minutes before exercise. Always perform the warm-up activity at ½ your normal pace.
Balance & Relaxation Techniques
Tai Chi and ballroom dancing are two good examples of activities which promote balance and relaxation. Studies showed that those with OA who participated in Tia Chi two times a week for eight weeks reported less pain, increased range of motion and improved daily activities and function. They also noted less low back pain and better sleeping.
Proper Clothing
Stay warm in winter and consider wearing compression shorts. Be cool in the summer months with DrytechR type material.
Pre/Post Exercise First Aid
If you are sore for longer than 12 to 24 hours after exercise, then you overdid it and must make adjustments next time. Otherwise, use hot packs, bath or shower before you exercise to loosen up and apply ice to your joints after exercise, especially if they are sore.
Post Exercise Stretch
Gentle, active range of motion stretches after exercise is important to maintain mobility. Do not bounce or cause pain. For example: Low Back – knees to chest; Arms – row –the – boat, arms behind head, arms behind back; Legs – wall lean calf stretch, bend and extend knees, open and close hips.
SOURCES: Rothman Institute, Philadelphia, PA and American Academy of Orthopaedic Surgeons; www.lifescript.com
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
I have been advising my patients to exercise, keep active, and walk as long as they can in order to stay mobile and healthy. However, seniors often tell me activities that require prolonged walking is limited by ankle pain from arthritis. They often ask, “What is arthritis of the ankle?” How does it happen? What can I do about it?
Your family physician will examine your ankle to determine if you have arthritis. In more advanced cases you may be referred to a specialist such as a podiatrist, orthopaedic surgeon or rheumatologist for further examination and treatment. X-rays will show if the joint space between the bones in the ankle is getting narrow from wear and tear arthritis. If rheumatoid arthritis is suspected, blood tests and an MRI may be ordered. The diagnosis will determine if you problem if minor, moderate or severe.
In the early stages your treatment will be a conservative, nonsurgical approach, which may include; anti-inflammatory medication, orthopedic physical therapy, exercise, activity modifications, supplements, bracing, etc. You and your family physician, podiatrist, orthopedic surgeon or rheumatologist will decide which choices are best.
When conservative measures no longer succeed in controlling pain and deformity, improving strength and function then more aggressive treatment may be necessary.
SOURCES: Rothman Institute, Philadelphia, PA and American Academy of Orthopaedic Surgeons
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Human beings were designed to move…walk, run, climb, lift, hunt, and gather. Contemporary man has suffered greatly from a technologically driven inactive and sedentary lifestyle. Inactivity is associated with many health problems; obesity, adult-onset diabetes, high blood pressure to name a few. The problems associated with lack of movement are many:
The more you move your body, the more you colon moves! A regular and consistent exercise and activity regime, results in a more consistent bowel schedule, especially with age. Healthy muscle tone in your abdominal muscles and diaphragm is also the key to moving waste through your digestive tract.
Osteoarthritis, rheumatoid arthritis and many inflammatory or auto-immune diseases can cause achy and stiff joints. However, even healthy joints can also stiffen when you don’t use them enough. Put them to work so they don't get tight and cause pain.
All muscles get weak from lack of use, including the muscles that help your lungs expand and contract as you breathe if you don’t work them out regularly. The less exercise or activity you do, the more you experience shortness of breath, even during easy daily tasks.
Physical problems are not the only complication of inactivity. A lack of movement can also increase feelings of anxiety and depression. Aerobic exercises like walking, biking, swimming, or running, have been proven to stimulate endorphins to boost and steady your mood, and even improve your self-esteem.
Many studies have found that regular movement improves energy. Exercise helps deliver oxygen and nutrients to your tissues. When you sit or are inactive, tissues are not getting the same amount of fuel they need to keep you going.
Movement stimulates your metabolism. Hyperactive people burn more calories…just by fidgeting! Even if you are not hyperactive, the more active you are, the more calories you burn each time you move.
One of the first recommendations sleep doctors make to their patients suffering from insomnia is exercise. When you keep a regular exercise routine, you fall asleep faster, and you sleep deeper once you drift off.
Regular exercise tells your body to make more chemicals called growth factors. They boost blood vessel production in your brain. The more blood that gets to your brain, the better you can think, remember, and make decisions.
Spending most of your time sitting raises your risk of heart disease, in great part due to the fact that partly you’re more likely to have high blood pressure. This is a big risk factor for heart issues like coronary artery disease and heart attack.
When physical activity is a regular part of your life, your body has an easier time keeping your blood glucose under control. Exercise can stabilize blood sugar levels and keep you out of the type 2 diabetes danger zone.
When your core muscles are weak from lack of use, they can’t support your back the way they should. This makes it much easier to tweak your back muscles during everyday movements like standing or reaching. Pilates, yoga, and other exercises that use stretching are good for building a stronger back. Schedule an appointment with a good orthopedic and sports PT.
Logically, one might think that you’d be hungry more often if you exercised more, but the opposite is usually true. Aerobic exercise like biking, swimming, walking, and running can actually decrease your appetite because it changes the levels of certain “hunger hormones” in your body.
Studies show the more moderate activity you get, the lower your chance of catching a cold or other germs. When you make exercise a habit, your immune system gets stronger.
If your skin looks duller than usual, a lack of movement may be to blame. Some studies show that moderate exercise boosts your circulation and your immune system, which helps your skin keep that youthful glow.
SOURCE: WebMD

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
It is four months since many people have made their health and fitness resolutions and hopefully some have stayed the course. If you are looking for another reason to stick to your New Year’s Resolution to get fit and lose weight in 2024 try this…to improve or prevent hip and knee pain!
There are three major weight-bearing joints in the body, the hip, knee and ankle/foot. Consequently, wear and tear and arthritis are common among these joints. There are almost 800,000 knee replacements and 450,000 hip replacements annually in the United States alone. While there are many recommended methods to avoid or delay joint replacement, only a few are within our control. Genetics, trauma, degenerative diseases such as rheumatoid arthritis and osteoarthritis are difficult to control. However, body weight, aggressive weight bearing sports and overdoing exercises as you age like excessive running, jumping, lifting and squatting can be modified or eliminated to limit the progression of joint damage. According to WebMD, “your knees are powerhouses. They’re the biggest, strongest, joints in your body, and most people use them throughout the day to sit, stand, walk, jump, and bend. They bear 80% of your body weight when you stand still and 150% or more when you walk across the room. In a 160-pound person, that’s 240 pounds of force!”
According to the National Institutes of Health, body weight or body mass index (BMI) has a direct impact on hip and knee degeneration, pain and dysfunction. In fact, one study found that people with or at risk of significant hip/knee osteoarthritis had a 2-3% reduction in risk of hip or knee replacement for every 1% reduction in weight, regardless of the baseline BMI.
It is commonly known that the primary cause of osteoarthritis is normal wear and tear, especially for those over 50. However, extra body weight can accelerate this process. As the joint degenerates, the cartilage at the end and in between your joints gets compressed and dehydrated which leads to deterioration. Eventually, the bones rub directly on each other as the cushion wears away, leading to pain, swelling, and stiffness, loss of motion, strength and function.
While it may seem obvious that extra weight will put more strain and stress on the hip and knee joints; another mechanism involved in this degenerative process. Excess body fat can increase chemicals in your blood stream that can cause inflammation in your joints.
If you need a goal and a motive, how about this: losing even 10 pounds will equate to 40 pounds less force compressing and stressing your hips and knees. Moreover, reducing body fat will limit the hormones that cause inflammation in your joints. Talk to your primary care physician or visit www.cdc .gov to find a BMI calculator. Just plug in your height and weight and it calculates it for you. For example, a 155-pound male at 5 feet 8 inches tall has a BMI of 23.6. (A BMI of 18.5 to 24.9 is considered a healthy weight for this person).
The Mediterranean Diet is a solid start to eating healthy. It is less of a diet and more of a lifestyle. The foundation of this diet is plant foods built around vegetables, fruits, herbs, nuts, beans and whole grains. Moderate amounts of fish, dairy, poultry and eggs with limited consumption of red meat are paramount. The Mediterranean lifestyle also includes shared meals with family and friends, small portions, regular exercise, and wine in moderation with food and friends.
Exercise has many more benefits than just losing weight. Physical activity is one of the most important factors in improving a lifestyle in a positive way. A minimum of 30 minutes of physical activity, 5 days per week can greatly contribute to weight loss and longevity.
Researchers have found that the benefits of regular physical activity are numerous. Some of the more important benefits are:
Visit your doctor regularly and listen to your body.
Keep moving, eat healthy foods, exercise regularly, and live long and well
SOURCES: WebMD, National Institutes of Health; CDC, American Council on Exercise

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
“Everybody talks about the weather, but nobody does anything about it,” said Mark Twain. Just ask 93% of the arthritis sufferers who believe that the weather affects their pain level. History tells us that Benjamin Franklin, Leonardo da Vinci, and Christopher Columbus also felt this way about the weather.
Patients at our clinic have been particularly sensitive to joint pain on cold, damp days, especially during the past few weeks. In my clinical practice of orthopedic and sports physical therapy, an informal survey found that 95 out of 100 patients (95%) with arthritis reported increased pain with weather changes. While most people report that the coldness and dampness seem to irritate their joints, they also report more pain with weather changes in the summer. There is a reasonable explanation…
Joints in the body have a lining called synovium that secretes a lubricating fluid called synovial fluid. In joints with arthritis, there is an overproduction of synovial fluid. In theory, when the barometric pressure changes, so to will the pressure inside your joints, especially if it is already overfull with extra fluid from arthritis. This added pressure stimulates the nerve endings in the joint to produce inflammation and pain.
Despite this overwhelming response from patients, scientific studies vary in their support of this claim. According to the Mayo Clinic, in 1961, a famous arthritis doctor (rheumatologist), built a climate chamber and discovered that when high humidity was combined with low barometric pressure, patients reported increased joint pain and stiffness. A recent study found that changes in barometric pressure and cooler temperatures are associated with joint pain. However, other studies have found increased joint pain with high barometric pressure in both warm and cold weather while another study found pain with low pressure.
What does this mean? It means that patients with arthritis consistently report pain with weather changes but science has not found an accurate method to consistently support these claims. Some of these inconsistencies may be attributed to the fact that there are differences in sensitivity among individuals. For example, some patients have symptoms before the weather changes, while others notice symptoms during or after the weather changes. Still yet, some report more pain in colder conditions while others notice more pain in warmer weather. It appears that changes in the weather, such as a high to a low or warm dry to cold damp and vice versa is the culprit when it comes to irritating arthritis in a joint.
If I have arthritis, should you move to Arizona? Yes and no! Yes, the warm and dry climate of Arizona will probably make you feel better overall. However, it will not cure the degenerative changes in your joints and you may still have pain when CHANGES in the weather occur. This is proven to be true by the fact that there are many very busy rheumatologists in Arizona!
In conclusion, it is safe to say that there is some evidence to support the claim that most patients with arthritis have increased symptoms of joint pain and stiffness with CHANGES in the weather:
Therefore, each patient must be individually evaluated by their physician to determine the extent of their arthritis and its relationship to the changes in the weather. While the cause of their increased symptoms with changes in the weather may not be completely understood, each patient must determine the adjustments in their lifestyle and/or medications according to the particular weather patterns that affect their problem most.
Visit your doctor regularly and listen to your body.

NEXT SUNDAY IN THE PAPER AND EVERY MONDAY'S BLOG – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's articles, visit our exercise forum!
Memorial Day is the unofficial kickoff to summer…outdoor furniture is out, the grill is fired up and the pool is open! This summer try to think of your pleasure puddle in different light…a health spa! It may very well be the exercise of choice for many people. Many have discovered the benefits of moving their limbs in the warm water of a home pool following knee or shoulder surgery. Also, long distance runners who often look for cross training methods without joint compression and arthritis sufferers who are often limited in exercise choices by joint pain from compressive forces when bearing weight, can enjoy the buoyancy effects of water. These are good examples of the benefits or water exercise…aerobic and resistive exercise without joint compression.
Most doctors recommend some form of exercise with arthritis. Pain and fatigue are the most limiting factors for the person with arthritis. Pool exercise may be the answer. With proper technique, adequate rest periods, appropriate resistance and repetitions, water exercise can be very effective.
The following are some of the benefits of water exercise:
Visit your doctor regularly and listen to your body.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's articles, visit our Health and Exercise Forum!
Osteoarthritis, the most common type of arthritis, is often considered to be a normal part of aging. Usually by the age of forty our joints, especially those which are weight bearing (lower spine, hips, knees, ankles, feet) begin to show signs of wear and tear. The cartilage begins to thin, joint surfaces are not as smooth, and fluid which lubricates the joint becomes diluted, dehydrated and less protective. Consequently, these aging joints become stiff, sore, weak, and swollen. Most people with osteoarthritis report additional pain and stiffness in the winter and early spring due to cold, damp weather and NEPA has plenty of it! The cold, for example, restricts the flow of blood to the joints, leading to more pain and stiffness. While moving to a warmer and less humid climate is one solution, it is not practical for most. But all is not lost because there are other alternatives to protect and keep your joints healthier this winter and early spring. And, if you are looking for some practical gift ideas for your loved ones suffering from arthritis, these tips may be valuable.
1.Parafin Bath and Hot Packs:
A paraffin bath is one of the best methods to apply heat to your hands and feet to ease pain and stiffness associated with osteoarthritis. A special heating unit works like a crock pot to melt the wax to liquid form. The hands and/or feet are dipped into the wax several times to create a warm coating around the entire area. A 20 to 30 minute treatment while watching TV or listening to good music will provide pain relief, improve mobility in the joints and bring life back to winter damaged skin. $39.99 to $159.99 (www.bedbathandbeyond.com). Hot packs, electric and microwavable, offer heat to bring blood flow and lessen joint pain and stiffness. They are great for neck and lower back pain, depending on the shape of the pad. Consider rectangle for lower back and cylinder/round to wrap around neck and joints of arms and legs. SourceMed.com offers an electric pad which creates moist heat for $59.95 and a microwave “bed buddy” (herbal or nonherbal) can be found for $9.99 to $43.95 at TheWarmingStore.
2.Hand and Toe Warmers:
Hand and toe warmers are small packets placed in the gloves or boots of skiers, campers and hikers to keep the hands and feet warm. These throw away warmers can also be used by anyone with cold hands or feet whether you are shoveling snow, attending an outdoor event in the cold or sitting in a cold, drafty room watching TV. (Walmart, Dick’s, Gander Mountain, www.amazon.com)
3.Knee, Ankle, Wrist, Elbow, Wrist Sleeves:
Supportive sleeves for the joints can provide protection and warmth year round, but especially during the cold winter and early spring. Those made with neoprene material offer warmth and compression and can be valuable when participating in activities such as skiing, walking, running, basketball name a few. Additionally, it can be helpful for those having joint pain with daily activities such as grocery shopping or house work. These devices should not be used when sitting for prolonged periods of time or sleeping. There is no scientific evidence that supports the use of cooper or magnets weaved into the sleeves for additional pain relief. (available at most pharmacies and medical equipment stores)
4.Compression Shorts and Shirts:
Similar to neoprene sleeves, compression shorts, pants and shirts can be invaluable to those participating in outdoor activities in cold temps. UnderArmor, Reebok, Nike, and others make these products which can also be worn indoors for those working in cool, drafty environments.
5.Hot Tub:
It seems obvious how and why hot water and massaging water jets can soothe the sore joints and muscles. To ensure additional pain and stress relief, add a candle, soft music and a cocktail!
6.Low Impact Exercise for Legs:
If you suffer from osteoarthritis to the joints of your lower body, you would be well-advised to limit impact activities such as running and basketball. Instead, walk, swim, use the elliptical and bike to protect your joints.
7.Low Impact Exercise for Arms:
As above, if you have arthritis in the joints of the upper body, use low weights, avoid push-ups and dips, which transfer your body weight through the arms.
8.Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
These over-the-counter, non prescription drugs include aspirin and ibuprofen (Advil, Motrin) which are very effective in the treatment of the pain and inflammation associated with arthritis. However, like all drugs, they are not without their risks so one must consult with their primary care physician and pharmacist before using them. For example, NSAIDs can thin the blood, irritate the stomach and may interact with other medications.
9.Topical Creams: Lidocane, Capsacian
Topical analgesics or pain relievers can be rubbed into or sprayed on the skin over the affected area. Some products are counterirritants using menthol, methylsalicylate and camphor which provide a sensation on the skin other than pain. Salicylate based products can work like aspirin to provide relieve from mild pain and inflammation. Capsaicin based products can also provide temporary relief due to the counter stimulation of warmth and tingling. A few things to keep in mind when using these products: one, discuss it with your physician or pharmacist. Two, topical agents are more effective in superficial joints such as the fingers, toes, wrist, elbow, knee and shoulder than in the deep tissues of the hip, buttocks, or lower back. Three, wash your skin thoroughly ater using these products and before using heat, cold or electric stimulation.
10.Massage: The therapeutic benefits of massage are well documented. However, like most treatments, it is important to find a qualified professional that meets your needs. Licensed physical therapists, physical therapist assistants and massage therapists are the best choice. Benefits include; relief from pain, headaches, muscle spasm, and stress, improved relaxation, posture, and breathing.
SOURCES: www.apta.org; www.webmd.com

This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
For all of Dr. Mackarey's Articles visit https://mackareyphysicaltherapy.com/forum/
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
Patients often tell me that they would like to exercise but hesitate due to their knee or hip pain. They want to know what type of exercise is best for those suffering from osteoarthritis (OA). Osteoarthritis is also known as degenerative arthritis. It is the most common form of arthritis in the knee. It is usually a gradual, slow and progressive process of “wear and tear” to the cartilage in the joint which eventually wears down to the bony joint surface. It is most often found in middle-aged and older people and in weight bearing joints such as the hip, knee and ankle. It causes gradual onset of pain, swelling and stiffness in the involved joint, especially after increased activity and weakness with loss of function due to disuse.
However, OA is not an excuse to avoid exercise but it is important to be smart about it. Regular exercise is essential to maintain a normal lifestyle for those with OA. However, if you do the wrong exercise, use poor technique, or are too aggressive, you could flare-up your joints and do more harm than good.
When performed correctly, exercise for those with OA has many benefits:
Pain Control
Exercise controls OA pain by releasing natural pain control chemicals in the body called endorphins. It also controls pain by assisting in weight loss and improving range of motion.
Weight Control
We all know how well exercise burns calories and that increased body weight creates increase stress on the joints.
Prevention of Joint Stiffness
Exercise will help maintain joint range of motion. A stiff joint is a painful joint.
Prevention of Muscle Weakness
Exercise will help maintain muscle strength. Weak muscles will allow or increase in joint wear and tear.
Maintain Lifestyle
If a joint is stiff and weak, then they become painful which negatively impacts your lifestyle. Exercise can prevent this problem.
Start Slowly
Wean into exercise because if you advance too quickly, you will flare up the joint and have increased pain. For example, walk for 5-10 minutes the first session. If you do not have pain, add 1-2 minutes each session.
Lose Weight
Every pound lost equates to less stress on your joints. For example, a loss of 5 pounds of body weight translates to 20-30 pounds of stress through the knee, according to David Borenstein, MD, President of the American College of Rheumatology. Also, body weight has a direct impact on daily activities. For example, walking upstairs creates stress through the knee equal to 4 times body weight and seven times body weight going downstairs. Therefore, less body weight equals less stress.
Low Impact Workouts
Low impact exercise creates less stress on the joints while strengthening leg muscles and those who those who maintain leg muscle strength have less stress on their joints. It is even important not to load your arms with heavy objects when walking or using stairs to limit joint stress.
Some examples of low-impact exercises are: walking, swimming, elliptical trainer, and biking. Strength training is also low-impact and should be performed with low weight and high repetitions. Water therapy is great for those with OA, especially in a heated pool. It is a great low-impact exercise with less gravity and stress on the joints. Walk, swim and do mild resistance exercises in the water. Use a snorkel and mask for swimming to limit excessive neck turning and back extension.
Walking is a great form of exercise; however, walking softly is important for those with OA. Wear good running shoes and orthotics if necessary. Discuss this with your physical therapist or podiatrist. When possible, use soft surfaces like cinder, mulch or rubber. Avoid grass and soft stand due to instability and torsion that may irritate your joints.
Warm-Up
Warming up your body is critical to prevent injury to the muscles and tendons. This can be done by marching in place or using aerobic equipment such as a bike for 5 to 10 minutes before exercise. Always perform the warm-up activity at ½ your normal pace.
Balance & Relaxation Techniques
Tai Chi and ballroom dancing are two good examples of activities which promote balance and relaxation. Studies showed that those with OA who participated in Tia Chi two times a week for eight weeks reported less pain, increased range of motion and improved daily activities and function. They also noted less low back pain and better sleeping.
Proper Clothing
Stay warm in winter and consider wearing compression shorts. Be cool in the summer months with DrytechR type material.
Pre/Post Exercise First Aid
If you are sore for longer than 12 to 24 hours after exercise, then you overdid it and must make adjustments next time. Otherwise, use hot packs, bath or shower before you
EVERY MONDAY – Read Dr. Paul J. Mackarey NEW Article in“Health & Exercise Forum!”
For all of Dr. Mackarey articles visit https://mackareyphysicaltherapy.com/forum/
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.