Happy Father’s Day! It is my hope that this information will be helpful to all the fathers who enjoy working in the yard! It is not too late to buy dad a new cart or kneeling pads for the yard. Last week, Health & Fitness Forum presented tips for gardeners for preventing hand and arm injuries such as carpal tunnel syndrome. This week’s column is dedicated to prevention of lower back and lower body injuries when working in the yard and for gardeners with disabilities.
A relaxing and enjoyable activity for many, gardening can turn dangerous without proper precaution as repetitive stress injuries, back pain, muscle pulls, can stem from raking, weeding, digging and pruning, can turn into serious problems if not treated appropriately. Since prevention is the best approach, the US Dept of Agriculture promotes warm-up exercises and injury prevention tips to help all levels of gardeners avoid serious and long-term injuries while enjoying this popular outdoor activity.
People with various disabilities enjoy gardening at different levels. For example, those suffering from neurological diseases with muscle weakness, paralysis and poor balance as well as those with musculoskeletal problems such as neck and LBP or hip and knee arthritis can safely enjoy gardening at some level. This outdoor labor of love is very therapeutic.
Warm up and stretching is important. Don’t garden first thing in the morning before you have a chance to warm up. Get up, go for a short walk, have breakfast and maybe warm up with a hot shower before working in the garden. Some stretches include;
Note: These exercises should never be painful when completing them. You should only feel a gentle stretch. Hold the stretch10 seconds and repeat 5 times before you garden and every 2-3 hours while working. Should you experience pain, please consult your family physician or physical therapist.
The following guidelines to prevent injury and foster healthy gardening for those with and without disability:
Source: Karen Funkenbusch, MA; Willard Downs, PhD.: U. S. Department of Agriculture - Agricultural Engineering Extension

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

While I normally do not address the topic of shoveling snow until January, considering recent weather events, I thought it might be valuable to present it sooner. Much has been written about the dangers of snow shoveling for your heart. However, while not fatal, low back pain is the most common injury sustained while shoveling snow. Heart attacks are also more common following wet and heavy snow.
Snow shoveling can place excessive stress on the structures of the spine. When overloaded and overstressed, these structures fail to support the spine properly. The lower back is at great risk of injury when bending forward, twisting, lifting a load, and lifting a load with a long lever. When all these factors are combined simultaneously, as in snow shoveling, the lower back is destined to fail. Low back pain from muscle strain or a herniated disc is very common following excessive snow shoveling.
Sources: The Colorado Comprehensive Spine Institute; American Academy of Orthopaedic Surgeons
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Fall has arrived in NEPA and walking is a great way to enjoy the fall foliage. Moreover, a new study has found that walking can reduce lower back pain. Researchers in Australia followed more than 700 adults who had a recent onset of lower back pain (and were able to bear full weight without associated leg symptoms) and enrolled them in a walking program under the supervision of a physical therapist. One group walked for 30 minutes, 3-5 times per week and the control group remained inactive. Both groups were followed for more than three years and discovered that the inactive control group was twice as likely to suffer from repeated flare-ups of lower back pain when compared to the walking group.
It is good news for those who enjoy walking, however, for many who have not maintained an active lifestyle or have health issues, it is challenging to know where to begin. Also, beginning without a good plan can lead to injury and leave you discouraged. For example, those overweight and de-conditioned should not start a walking program too aggressively. Walking at a fast pace and long distance without gradually weaning yourself into it will most likely lead to problems.
There is probably nothing more natural to human beings than walking. Ever since Australopithecus, an early hominin (human ancestor) who evolved in Southern and Eastern Africa between 4 and 2 million years ago, our ancestors took their first steps as committed bipeds. With free hands, humans advanced in hunting, gathering, making tools etc. while modern man uses walking as, not only a form of locomotion, but also as a form of exercise and fitness. It is natural, easy and free...no equipment or fitness club membership required!
Walking to reduce or control lower back pain is only one of many important reasons to begin a program. According to the American Heart Association, walking as little as 30 minutes a day can provide the following benefits:
Anything is better than nothing! However, for most healthy adults, the Department of Health and Human Services recommends at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous aerobic activity, or an equivalent combination of moderate and vigorous aerobic activity. The guidelines suggest that you spread out this exercise during the course of a week. Also aim to do strength training exercises of all major muscle groups at least two times a week.
As a general goal, aim for at least 30 minutes of physical activity a day. If you can't set aside that much time, try several short sessions of activity throughout the day (3 ten or 2 fifteen-minute sessions). Even small amounts of physical activity are helpful, and accumulated activity throughout the day adds up to provide health benefit.
Remember it's OK to start slowly — especially if you haven't been exercising regularly. You might start with five minutes a day the first week, and then increase your time by five minutes each week until you reach at least 30 minutes.
For even more health benefits, aim for at least 60 minutes of physical activity most days of the week. Once you are ready for a challenge, add hills, increase speed and distance.
Keeping a record of how many steps you take, the distance you walk and how long it takes can help you see where you started from and serve as a source of inspiration. Record these numbers in a walking journal or log them in a spreadsheet or a physical activity app. Another option is to use an electronic device such as a smart watch, pedometer or fitness tracker to calculate steps and distance.
Make walking part of your daily routine. Pick a time that works best for you. Some prefer early morning, others lunchtime or after work. Enter it in your smart phone with a reminder and get to it!
Studies show that compliance with an exercise program is significantly improved when an exercise buddy is part of the equation. It is hard to let someone down or break plans when you commit to someone. Keep in mind that your exercise buddy can also include your dog!
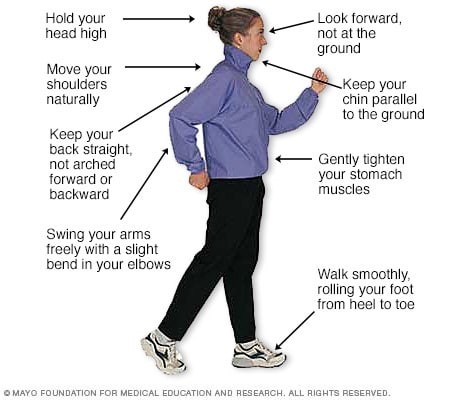
Like everything, there is a right way of doing something, even walking. For efficiency and safety, walking with proper stride is important. A fitness stride requires good posture and purposeful movements. Ideally, here's how you'll look when you're walking:
Sources : Sapiens.org; WebMD; Mayo Clinic, “Health & Science New”
Visit your doctor regularly and listen to your body

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

“When is it safe for my child to start weight training?” This is a very common question asked by parents of young athletes who are looking for advice regarding their children’s participation in weight training. This month, for example, I received three such inquiries. While some who are eager to get a “competitive edge” may not be satisfied with the answer, these recommendations are grounded in the scientific literature and medical specialist with the hope to prevent injury and dispel fear and fallacy.
Weight training, weight lifting or resistive training all describes the use of a resistive force on a muscle to improve strength. While much attention has been given to the benefits of weight training in adults, much less has been written about its application in children.
According to the Journal of Pediatric Orthopedics, children less than 12 years old are considered prepubescent or before puberty. Teenagers who are between 12 and 19 are considered to be adolescents. Studies consistently demonstrate that strength gains are much more significant in adolescents than in preadolescents. It is important to note that these strength gains are not only from the enlargement of muscle fibers (hypertrophy), but also from the improvement in the coordination and efficiency in muscle contraction and the recruitment of motor units and fibers within the muscle.
Preadolescents lack the hormones necessary to develop masculine characteristics. Adolescents begin to produce the hormones of testosterone and androsterone to develop secondary sexual characteristics such as pubic hair and enlarged genitalia. In view of this, age 13-14 is the optimal age to safely begin and benefit from a well-designed weight training program.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

While many people celebrate the Labor Day holiday by firing up the grill, others will be shopping to get their students ready for the school year. One item on the shopping list should be a good quality and well-fitted backpack…to prevent lower back pain!
In 2018, the government of India announced a ban on homework and recently in Poland; the government ministers did the same. Can you imagine…a ban on homework? In an effort to promote student health and address recent surges in the incidence of back pain in the young, there will be no homework for students in grades one and two.
It was estimated that the majority of students ages 7 – 13 in India were carrying almost half their body weight. Not surprisingly, medical practitioners noticed a dramatic increase in reported cases of back pain among this group and decided to take action. In addition to the homework ban for grades one and two, Indian authorities have also implemented a limit of 10% of the student’s body weight.
Back pain in students seems to be universal. Each year, as students in the United States prepare to return to school from summer vacation, the subject of backpacks arises. The good news: when compared to purses, messenger bags, or shoulder bags, backpacks are the best option to prevent lower back pain. The bad news is, most of the 40 million students in the USA using backpacks, are doing so incorrectly.
Studies have found more than 33% of children had LBP that caused them to miss school, visit a doctor, or abstain from activity. Also, 55% of children surveyed carried backpacks heavier than the 10-15% of their body weight, which is the maximum weight recommended by experts. Additionally, the study noted that early onset of LBP leads to greater likelihood of recurrent or chronic problems. Backpacks that are too heavy are particularly harmful to the development of the musculoskeletal system of growing youngsters. It can lead to poor posture that may lead to chronic problems.
The following information on backpack safely is based, in part, by guidelines from The American Physical Therapy Association. Parents and teachers would be wise to observe the following warning signs of an overloaded and unsafe backpack:
Consider the following suggestions to promote backpack safely and prevent back injury:

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Human beings were designed to move…walk, run, climb, lift, hunt, and gather. Contemporary man has suffered greatly from a technologically driven inactive and sedentary lifestyle. Inactivity is associated with many health problems; obesity, adult-onset diabetes, high blood pressure to name a few. The problems associated with lack of movement are many:
The more you move your body, the more you colon moves! A regular and consistent exercise and activity regime, results in a more consistent bowel schedule, especially with age. Healthy muscle tone in your abdominal muscles and diaphragm is also the key to moving waste through your digestive tract.
Osteoarthritis, rheumatoid arthritis and many inflammatory or auto-immune diseases can cause achy and stiff joints. However, even healthy joints can also stiffen when you don’t use them enough. Put them to work so they don't get tight and cause pain.
All muscles get weak from lack of use, including the muscles that help your lungs expand and contract as you breathe if you don’t work them out regularly. The less exercise or activity you do, the more you experience shortness of breath, even during easy daily tasks.
Physical problems are not the only complication of inactivity. A lack of movement can also increase feelings of anxiety and depression. Aerobic exercises like walking, biking, swimming, or running, have been proven to stimulate endorphins to boost and steady your mood, and even improve your self-esteem.
Many studies have found that regular movement improves energy. Exercise helps deliver oxygen and nutrients to your tissues. When you sit or are inactive, tissues are not getting the same amount of fuel they need to keep you going.
Movement stimulates your metabolism. Hyperactive people burn more calories…just by fidgeting! Even if you are not hyperactive, the more active you are, the more calories you burn each time you move.
One of the first recommendations sleep doctors make to their patients suffering from insomnia is exercise. When you keep a regular exercise routine, you fall asleep faster, and you sleep deeper once you drift off.
Regular exercise tells your body to make more chemicals called growth factors. They boost blood vessel production in your brain. The more blood that gets to your brain, the better you can think, remember, and make decisions.
Spending most of your time sitting raises your risk of heart disease, in great part due to the fact that partly you’re more likely to have high blood pressure. This is a big risk factor for heart issues like coronary artery disease and heart attack.
When physical activity is a regular part of your life, your body has an easier time keeping your blood glucose under control. Exercise can stabilize blood sugar levels and keep you out of the type 2 diabetes danger zone.
When your core muscles are weak from lack of use, they can’t support your back the way they should. This makes it much easier to tweak your back muscles during everyday movements like standing or reaching. Pilates, yoga, and other exercises that use stretching are good for building a stronger back. Schedule an appointment with a good orthopedic and sports PT.
Logically, one might think that you’d be hungry more often if you exercised more, but the opposite is usually true. Aerobic exercise like biking, swimming, walking, and running can actually decrease your appetite because it changes the levels of certain “hunger hormones” in your body.
Studies show the more moderate activity you get, the lower your chance of catching a cold or other germs. When you make exercise a habit, your immune system gets stronger.
If your skin looks duller than usual, a lack of movement may be to blame. Some studies show that moderate exercise boosts your circulation and your immune system, which helps your skin keep that youthful glow.
SOURCE: WebMD

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Several years ago, while hiking to the bottom of the Grand Canyon with my family, my wife Esther developed “canyon knee,” also known as “hiker’s knee” or in medical terms, “patellar tendonitis.” Regardless of the term, the end result was that she had severe pain in the tendon below her knee cap and was unable to walk up the trail to get out of the canyon. In addition to ice, rest, bracing, and non-steroidal anti inflammatory medications, the National Park Ranger insisted that she use two trekking poles on her ascent to the rim.
Prior to that experience, I always thought that “walking, hiking sticks or trekking poles” were for show or those in need of a walking aide. Well, I could not have been more incorrect. Needless to say, Esther made it out of the canyon safely and, with the use of our life saving trekking poles; we have lived “happily ever after!” Now, 15 years later, I rarely walk more than 5 miles without my poles.
As a result of this experience, I have been recommending walking or trekking poles to my patients. These poles are an essential part of hiking or distance walking gear, for the novice and expert alike. Specifically, for those over 50 who have degenerative arthritis and pain in their lower back, hips, knees, ankles or feet, these simple devices have been shown to improve the efficiency of the exercise and lessen the impact on the spine and lower extremities. Additionally, using poles reduces the likelihood of ankle sprains and falls during walking. Trekking poles are also a safe option for those with compromised balance. If you want to walk distances for exercise and need a little stability but don’t want the stigma of a cane, trekking poles are for you.
Early explorers, Europeans and Native Americans have been using walking sticks for centuries. More recently, in the 1968 classic hiker’s bible, “The Complete Walker,” Colin Fletcher praised his “walking staff” for its multipurpose use: for balance and assistance with walking and climbing, protection from rattlesnakes, and for use as a fishing rod. Today, these sticks are now versatile poles made from light-weight materials.
Trekking poles are made of light-weight aluminum and vary in cost and quality. But, like most things, “you get what you pay for!” These hollow tubes can telescope to fit any person and collapse to pack in luggage for travel. Better poles offer multiple removable tips for various uses, conditions and terrains. For example, abasket to prevent sinking too deeply in snow, mud or sand; a blunt rubber tip for hard surfaces like asphalt or concrete, or the pointed metal tip to grip ice or hard dirt/gravel. Better quality poles offer an ergonomic hand grip and strap and a spring system to absorb shock through your hands, wrists and arms upon impact.

The poles should be properly adjusted to fit each individual. When your hand is griping the handle the elbow should be at a 90 degree angle. Proper use is simple; just walk with a normal gait pattern of opposite arm and leg swing. For example, left leg and right arm/pole swings forward to plant while the left arm/pole remain behind with the right leg .
This pattern is reciprocated with as normal gait advances (opposite arm and leg). I have been very pleased with my moderately priced poles (Cascade Mountain Tech from Dick’s Sporting Goods ($34.99 per pole). Prices range from $19.99 to 79.95 per pole. dickssportinggoods.com; montem.com; leki.com; rei.com. However, if you travel frequently to hike the State and National Parks, you may want to purchase more expensive poles that collapse and retighten more efficiently. (montem.com; leki.com;)
Montem Trekking Poles - with close-up of easy adjustable locking clasp.

There are numerous studies to support the use of trekking poles, especially research that supports their use for health and safety. One study compared hikers in 3 different conditions; no backpack, a pack with 15% body weight and a pack with 30% body weight. Biomechanical analysis was performed blindly on the three groups and a significant reduction in forces on lower extremity joints (hip, knee, and ankle) was noted for all three groups when using poles compared to those not using poles.
Another study confirmed that trekking poles reduced the incidence of ankle fractures through improved balance and stability. Additional studies support the theory that trekking poles reduce exercise induced muscle soreness from hiking or walking steep terrain and another study found that while less energy is expended in the lower body muscles using poles, increase energy is used in the upper body; therefore, the net caloric expenditure is equal as it is simply transferred from the legs to the arms.
In conclusion, it is important to remember that trekking poles for hiking or distance walking are much more than a style statement. They are proven to be an invaluable tool for health, safety and wellness by reducing lower extremity joint stress, improving stability and balance, and enhancing efficiency for muscle recovery.
Sources: Medicine and Science in Sports and Exercise. The Complete Walker, by Colin Fletcher
Model: Andrea Molitoris, PT, DPT at Mackarey Physical Therapy

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
There is little doubt that the workplace has been redefined since the pandemic as many employees continue to work from home. Sitting for many hours at a workstation that may not be optimal has also changed the way we define workplace health and safety. It may be more important than ever to pay close attention to designing an ergonomic workstation, changing position, and stretching regularly to prevent injury.
Since 1894 Labor Day has been designated as the national holiday that pays tribute to the contributions and achievements of American workers. Research supports the notion that healthier employees are happier and more productive. When employers encourage healthy behavior and safety at work, they benefit in many ways. For example, in addition to improving job satisfaction and productivity, healthy employees save money by using less sick time, worker’s compensation benefits and health benefits. For example, according to the Centers for Disease Control and Prevention, approximately 75 percent of employers” health care costs are related to chronic medical problems such as obesity, diabetes, high blood pressure, and high cholesterol. De-conditioned, overweight employees are more likely to suffer from these preventable conditions and are at greater risk for injury. Employers, please consider using this holiday as an opportunity to start a health promotion program at your workplace…have a health fair, offer healthy snacks, encourage walking, smoking cessation, exercising at lunch, and offer fitness club stipends.
Lower back pain, one of the costliest illnesses to employers, is one example of a problem which can be prevented with a good health and safety program. It is widely accepted in the medical community that the best treatment for lower back pain (LBP) is prevention. Keeping fit, (flexible and strong), practicing good posture, and using proper body mechanics are essential in the prevention of LBP. At our clinic, significant time and effort is spent emphasizing the importance of these concepts to our patients, employees, and the businesses we work with through industrial medicine programs. A comprehensive approach can produce significant reductions in LBP injuries through an onsite safety program which promotes education, wellness, body mechanics, lifting techniques, postural and stretching exercises and ergonomics.
As little as 10 extra pounds puts great stress on your lower back. It also makes it more difficult to maintain good posture. Eat well, exercise regularly and don’t smoke. Smokers have a much higher incidence of LBP and failure from lower back surgery.
Good posture is critical for a healthy back. When sitting, standing or walking maintain a slight arch in your lower back, keep shoulders back, and head over your shoulders. In sitting, use a towel roll or small pillow in the small of the back. Also, consider sitting on a physio ball, which promotes proper posture for part of the day.


Perform postural exercises throughout the day. Most of the day we sit, stand, and reaching forward and bend our spine. These exercises are designed to stretch your back in the opposite direction of flexion. Please perform slowly, hold for 3-5 seconds and repeat 6 times each 6 times per day.
Chin Tuck: Tuck your chin back to bring your head over shoulders.
Shoulder Blade Pinch: Pinch your shoulder blades together.
Standing Extension: While standing, put your hands behind back and extend lower back 10-20 degrees.
Good Body Mechanics and ergonomics are also important in the prevention of LBP. When lifting, think twice. Think about the weight, shape and size of the object. Think about where the object is going and the surface resistance of the floor. Does it require two people to lift? Can I safely lift that high or bend that low?
When bending to lift an object think about safety:
Proper Lifting Technique:
Visit your doctor regularly and listen to your body.
Model: Lexi DiGregorio, PTA

NEXT SUNDAY IN THE PAPER AND EVERY MONDAY'S BLOG – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Paul's articles, check out our exercise forum!
Covid-19 has certainly redefined the workplace as many employees continue to work from home. Prolonged hours sitting at a workstation that may not be optimal has also changed the way we define workplace health and safety. It may be more important than ever to pay close attention to designing an ergonomic workstation, changing position, and stretching regularly to prevent injury.
Since 1894 Labor Day has been designated as the national holiday that pays tribute to the contributions and achievements of American workers. Research supports the notion that healthier employees are happier and more productive. When employers encourage healthy behavior and safety at work, they benefit in many ways. For example, in addition to improving job satisfaction and productivity, healthy employees save money by using less sick time, worker’s compensation benefits and health benefits. For example, according to the Centers for Disease Control and Prevention, approximately 75 percent of employers” health care costs are related to chronic medical problems such as obesity, diabetes, high blood pressure, and high cholesterol. Deconditioned, overweight employees are more likely to suffer from these preventable conditions and are at greater risk for injury. Employers, please consider using this holiday as an opportunity to start a health promotion program at your workplace…have a health fair, offer healthy snacks, encourage walking, smoking cessation, exercising at lunch, and offer fitness club stipends.
Lower back pain, one of the costliest illnesses to employers, is one example of a problem which can be prevented with a good health and safety program. It is widely accepted in the medical community that the best treatment for lower back pain (LBP) is prevention. Keeping fit, (flexible and strong), practicing good posture, and using proper body mechanics are essential in the prevention of LBP. At our clinic, significant time and effort is spent emphasizing the importance of these concepts to our patients, employees, and the businesses we work with through industrial medicine programs. A comprehensive approach can produce significant reductions in LBP injuries through an onsite safety program which promotes education, wellness, body mechanics, lifting techniques, postural and stretching exercises and ergonomics.

Visit your doctor regularly and listen to your body.
NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit: mackareyphysicaltherapy.com
More than 65 million people, almost 30% of the population in the United States, are actively involved in providing 20 or more hours of care for a chronically ill, disabled, or aged family member or friend each week. As our population continues to age, this number is expected to grow rapidly.
The role of a caregiver is multifaceted and often involves tasks and skills beyond the education or comfort level of most providers. Some examples include; managing money, paying bills, shopping, cleaning, maintaining and repairing a home, dispensing and injecting medications, cleaning wounds, changing dressings, catheter management, bed baths, assisting in position changes, transferring from the bed to the chair, ambulation, stair climbing, bathroom assistance for toileting and showering and many other responsibilities. Consequently, a caregiver is often at risk for mental, spiritual and physical fatigue or breakdown. It is no surprise that depression, illness and injury often plague a caregiver and eventually, the caregiver is in need of a caregiver. One of the most common injuries suffered by a caregiver is back pain.
Lower back pain (LBP) is one of the most common problems in our society. Over 90% of all Americans will suffer from it at least once in their lives. It is generally agreed that prevention is the best treatment for LBP.
As little as 10 extra pounds puts great stress on your lower back. It also makes it more difficult to maintain good posture. Eat well and exercise regularly.
Aerobic exercise will help prevent weight gain and stiffness for a healthier lower back. It will also help with the stress and depression associated with providing care for a loved one. Perform mild aerobic exercise such as walking 3-5 times per week for 30-45 minutes. You can also use an elliptical or bike at home while your loved one is resting. Get outdoors and take multiple short walks …go around the block a few times per day.
Core stabilization exercises designed to strengthen the abdominal and lower back muscles will help prevent injury. Some examples of core exercises are:
Pelvic Tilt - lying on your back and performing a pelvic tilt as you flatten you lower back into the floor.
Pelvic Tilt and Heel Slide - lying on your back, hold a pelvic tilt as you slide your one heel up and down and repeat with the other heel.
Core on Ball - Perform arm exercises such as biceps and triceps with light weight while sitting on a therapeutic ball while simultaneously trying to hold an isometric contraction of your abdominal and lower back muscles.
Smoking effects natural healing because it constricts the small blood vessels. Smokers have a much higher incidence of LBP and failure from lower back surgery.
Good posture is critical for a healthy back. When sitting, standing or walking maintain a slight arch in your lower back, keep shoulders back, and head over your shoulders. In sitting, use a towel roll or small pillow in the small of the back.
Caregivers spend much of the day with their spine bent over a bed or chair feeding, bathing, and lifting a loved one. Postural exercises are designed to stretch your back in the opposite direction of this forward flexed position. Examples include:
Bend your knees, maintain an arch in the back with head up, and bend over as little as possible. Bend the knees of your loved one; roll their trunk toward you to get their legs over the edge of the bed as you pivot their weight on their butt to get them sitting upright.
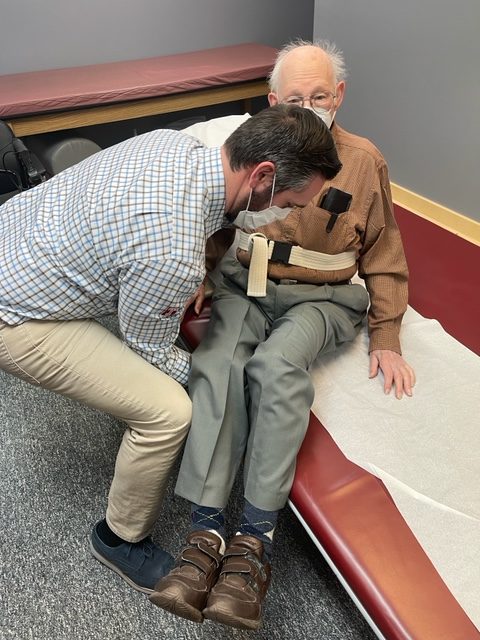
Bend your knees, maintain an arch in the back with head up, and bend over as little as possible. Place your hands around the waist or on a transfer belt. Use your legs, turn with feet, and do not twist spine. Block the feet and knees of your loved-one with your feet and knees and use them to pivot and transfer from the bed to the chair. Be sure the chair is along side of the bed and arm of chair removed if possible before the lift.
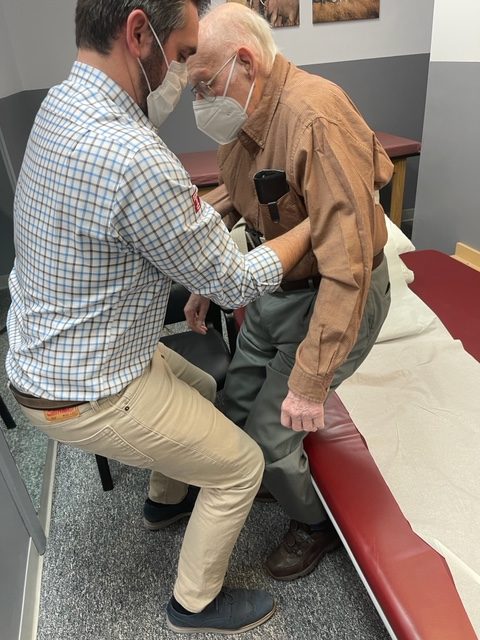
Transfer Belt - Use a transfer belt around the waist of the patient. Grip the transfer belt, instead of the patient or clothing, during the lift or when ambulating. Lower Back Lifting Belt - Also, if you have a back problem, consider using a lifting belt or back brace to protect your back when lifting the patient. Immediately following the lift, stand up straight and stretch lower back into extension.
Transfer belts and lower back lifting belts can be found online or at your local pharmacy.
Lift Chair – For patients that require maximum or moderate assistance and only one caregiver is available to lift or transfer, an electric lift chair should be considered.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice in downtown Scranton and is an associate professor of clinical medicine at GCSOM.
Visit your doctor regularly and listen to your body.
For all of Dr. Mackarey's articles visit: https://mackareyphysicaltherapy.com/forum/