It is four months since many people have made their health and fitness resolutions and hopefully some have stayed the course. If you are looking for another reason to stick to your New Year’s Resolution to get fit and lose weight in 2024 try this…to improve or prevent hip and knee pain!
There are three major weight-bearing joints in the body, the hip, knee and ankle/foot. Consequently, wear and tear and arthritis are common among these joints. There are almost 800,000 knee replacements and 450,000 hip replacements annually in the United States alone. While there are many recommended methods to avoid or delay joint replacement, only a few are within our control. Genetics, trauma, degenerative diseases such as rheumatoid arthritis and osteoarthritis are difficult to control. However, body weight, aggressive weight bearing sports and overdoing exercises as you age like excessive running, jumping, lifting and squatting can be modified or eliminated to limit the progression of joint damage. According to WebMD, “your knees are powerhouses. They’re the biggest, strongest, joints in your body, and most people use them throughout the day to sit, stand, walk, jump, and bend. They bear 80% of your body weight when you stand still and 150% or more when you walk across the room. In a 160-pound person, that’s 240 pounds of force!”
According to the National Institutes of Health, body weight or body mass index (BMI) has a direct impact on hip and knee degeneration, pain and dysfunction. In fact, one study found that people with or at risk of significant hip/knee osteoarthritis had a 2-3% reduction in risk of hip or knee replacement for every 1% reduction in weight, regardless of the baseline BMI.
It is commonly known that the primary cause of osteoarthritis is normal wear and tear, especially for those over 50. However, extra body weight can accelerate this process. As the joint degenerates, the cartilage at the end and in between your joints gets compressed and dehydrated which leads to deterioration. Eventually, the bones rub directly on each other as the cushion wears away, leading to pain, swelling, and stiffness, loss of motion, strength and function.
While it may seem obvious that extra weight will put more strain and stress on the hip and knee joints; another mechanism involved in this degenerative process. Excess body fat can increase chemicals in your blood stream that can cause inflammation in your joints.
If you need a goal and a motive, how about this: losing even 10 pounds will equate to 40 pounds less force compressing and stressing your hips and knees. Moreover, reducing body fat will limit the hormones that cause inflammation in your joints. Talk to your primary care physician or visit www.cdc .gov to find a BMI calculator. Just plug in your height and weight and it calculates it for you. For example, a 155-pound male at 5 feet 8 inches tall has a BMI of 23.6. (A BMI of 18.5 to 24.9 is considered a healthy weight for this person).
The Mediterranean Diet is a solid start to eating healthy. It is less of a diet and more of a lifestyle. The foundation of this diet is plant foods built around vegetables, fruits, herbs, nuts, beans and whole grains. Moderate amounts of fish, dairy, poultry and eggs with limited consumption of red meat are paramount. The Mediterranean lifestyle also includes shared meals with family and friends, small portions, regular exercise, and wine in moderation with food and friends.
Exercise has many more benefits than just losing weight. Physical activity is one of the most important factors in improving a lifestyle in a positive way. A minimum of 30 minutes of physical activity, 5 days per week can greatly contribute to weight loss and longevity.
Researchers have found that the benefits of regular physical activity are numerous. Some of the more important benefits are:
Visit your doctor regularly and listen to your body.
Keep moving, eat healthy foods, exercise regularly, and live long and well
SOURCES: WebMD, National Institutes of Health; CDC, American Council on Exercise

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Injuries due to falling are a very common problem in the elderly. Hip fractures are the most common injury due to falling in the seniors. According to the American Academy of Orthopaedic Surgeons, each year more than 300,000 people are hospitalized for hip fractures in the United States. These fractures represent 72% of all fracture costs, totaling more than 12 billion dollars in 2005 and, not surprisingly, 90% occurred in those 65 and older. Most hip fracture patients who previously lived independently will require family assistance, home or long term care and 50% will require a cane or walker.
A recent study by the American Physical Therapy Association found that patients benefited from a physical therapy evaluation to determine their risk level for falling. If a high-risk level is found on a falls assessment, physical therapy interventions can be successfully employed to improve strength, balance, and coordination and falls prevention. Also, a well-balanced diet, exercise, Calcium with vitamin D supplements and medications can help prevent or retard osteoporosis and prevent hip fractures.
***Always perform slowly, alternate right and left sides, limit other distractions and concentrate on the exercise to retrain the brain, 10-20 times each 2-3 times per day.
***Caution: Do not do standing exercises without assistance or supervision if needed
Face a countertop and hold onto it with both hands. Hike your hip and knee up to 90 degrees as if you are marching. Hold the position for 3-5 seconds on one leg and lower slowly. Repeat this on the other leg and alternate 10 times.

Face a countertop and hold onto it with both hands. Lift your leg up 30 degrees as if you are spreading your legs apart. Hold the position for 3-5 seconds on one leg and lower slowly to cross over the middle. Repeat this on the other leg and alternate 10 times.
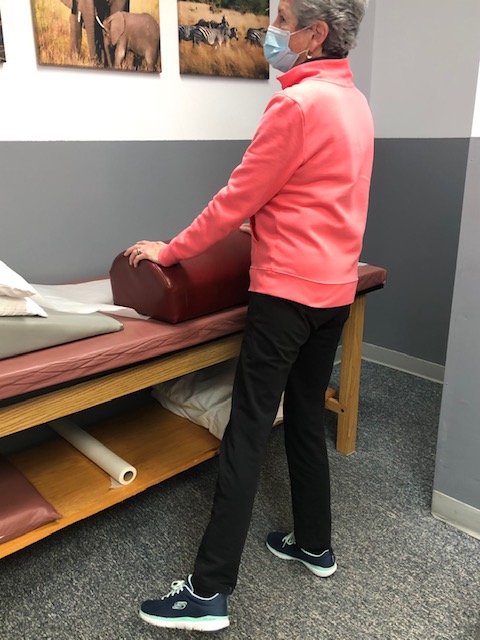
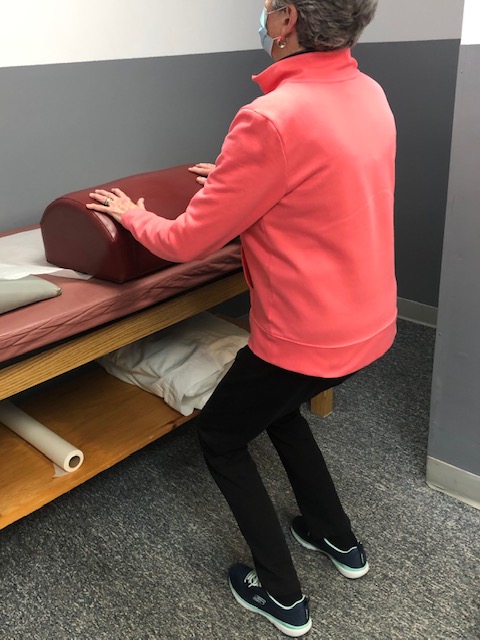
Face a countertop and hold onto it with both hands. Bend your hip and knee down to 45 degrees to a squatting position. Hold the position for 3-5 seconds on both legs and return to standing slowly. Repeat this 10 times. Once strong enough try on one leg at a time and alternate.
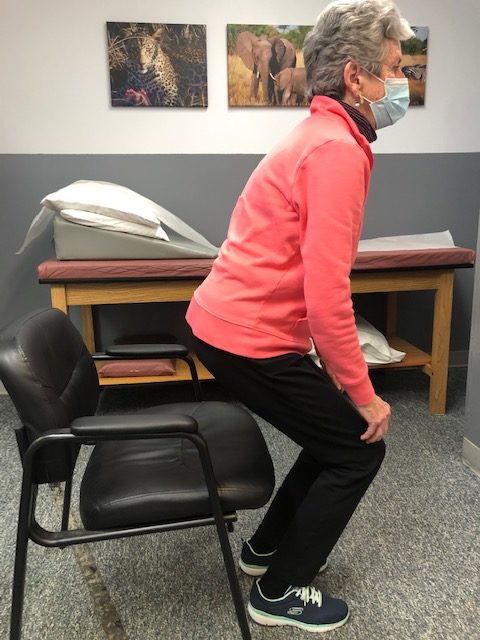
Sit in a chair with arm rests. Get out of chair only using your legs. Hold the position for 3-5 seconds and return to sitting. If necessary, use 1 or 2 arms to assist. Repeat this 10 times. Focus on trunk core stabilization and leg strength. Use more leg muscles and less arm muscles as strength improves.
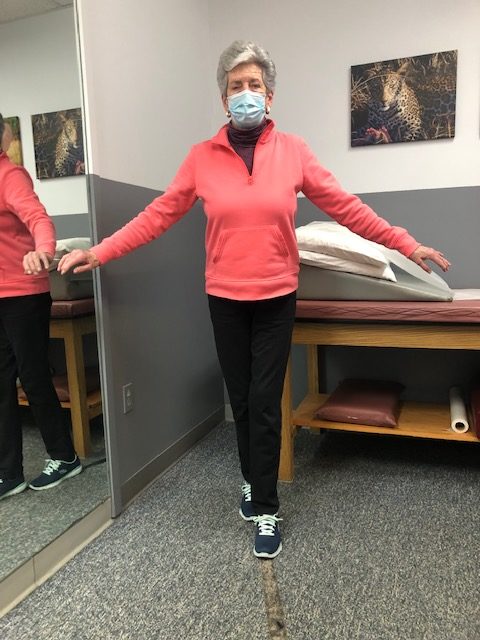
Place a straight line on the floor and practice “walking the line” with the right then left foot on the line.
Hold onto a chair while bending one knee and shifting your weight to the other leg. Hold for 3-5 seconds and repeat with the other leg. Increase time 10 -15 -20 seconds as tolerated.

If you feel you or a loved one may be at risk for falling or a hip fracture, ask your family physician if a physical therapy consultation for a falls prevention program to prevent hip fractures may benefit you.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit www.mackareyphysicaltherapy.com/forum
When an older loved one sustains a serious injury it is traumatic for the entire family and mine is no exception. My grandmother and father enjoyed 90 wonderfully active years; however, their independence was lost the same way more than one-third of a million people lose their independence each year… hip fractures! As a doctor of orthopedic physical therapy, I feel remise that I could not prevent this from happening. What most of us fail to realize is that his fracture, like many, was more than just an orthopedic problem …it involves age, gender, diet, exercise, vision, leg strength, medications, environmental risks, and vestibular problems (inner ear problems effecting balance).
Injuries due to falling are a very common problem in the elderly. Hip fractures are the most common injury due to falling in the seniors. According to the American Academy of Orthopaedic Surgeons, each year more than 300,000 people are hospitalized for hip fractures in the United States. These fractures represent 72% of all fracture costs, totaling more than 12 billion dollars in 2005 and, not surprisingly, 90% occurred in those 65 and older. Most hip fracture patients who previously lived independently will require family assistance, home or long term care and 50% will require a cane or walker.
Several risk factors for hip fractures have been identified. While some factors are somewhat controllable and may improve bone quality, (diet, exercise, smoking, alcohol) others are not.
Vestibular or inner ear problems
Preventing a fall can not only save your independence but also your life! Preventing injuries from falls reduces the need for nursing home placement.
NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” Hip Fractures - Part II of II

This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's Articles visit: www.mackareyphysicaltherapy.com/forum
Rehabilitation is defined as the process of restoring something that has been damaged to its former condition. Recovering from joint replacement surgery involves intensive rehabilitation to attain full recovery. In recent years, however, the concept of rehabilitation “before” surgery or “prehabilitation” has been encouraged by most physical therapists and other rehab professionals as an opportunity to expedite the post operative rehabilitation process.
A recent study revealed that strength training before a surgical procedure can counteract muscle wasting associated with bed rest and limited mobility after a procedure. Two systematic reviews revealed that “prehab” exercise decreased pain and complication after the surgery and improved rehabilitation following the procedure. The studies also noted that individuals rehabilitated and attained goals faster, saving time and money. Due to these findings it is our opinion that prehab is an essential part of a comprehensive rehabilitation program for total knee (TKR) or total hip replacement (THR) surgery.
Therefore, it is important to plan ahead and discuss the best “prehab” program for you with your orthopedic surgeon and physical therapist.
“Prehabilitation” enables individuals preparing for a total joint replacement to maintain or improve range of motion, strength, and endurance prior to going for a surgical procedure. We recommend doing at least 4-6 of these exercises 2 times a day to help improve the conditioning of the body prior to surgery and the overall recovery and rehabilitation process following. When completing these exercises, it is important that the movements are symptom and pain free. Should you experience any pain or discomfort with an exercise, you should not continue to perform that exercise. The goal of “prehabilitation” is to prepare the body for your surgical procedure and improve the outcomes and success of the surgery, not further injure or hurt yourself in the process. Therefore, you may not be able to complete all the exercises listed, which is okay, just do your best and what you can! In conclusion, performing exercises prior to having a total joint replacement can enhance your recovery and post-op rehabilitation, so put your best foot forward and take the right steps toward a better total joint replacement with “prehabilitation!”
More Information: For a complete list of these exercises, visit our website at www.mackareyphysicaltherapy.com or call to see how Mackarey Physical Therapy can help you!
Guest Authors: Paul Mackarey, Jr, PT, DPT, clinic director at Mackarey & Mackarey Physical Therapy and Andrea Molitoris, PT, DPT, associate at Mackarey & Mackarey Physical Therapy.

Read Dr. Mackarey’s Health & Exercise Forum – Every Monday
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.