I enjoy the privilege of working with people recovering from a wide variety of medical conditions. Many of these conditions can directly affect activities of daily living, particularly, the ability to drive safely: orthopedic and sports injuries, fractures, sprains and strains, joint replacements, hip fractures, shoulder and elbow surgeries and spinal fusions. Despite the many different types of problems, there is one question that is invariably asked, “When can I return to driving?” Unfortunately, the answer is not as simple as the question because it depends on many factors. Furthermore, the implications, such as a serious accident causing further damage to the injury or surgical site or harm to someone else, are significant and possibly critical. So, the next time you ask your physician this question, please follow instructions and be patient…remember, it could be your child or grandchild running into traffic to chase a ball and you would want the driver to be at optimal function to apply the brakes!
In our culture, the inability to drive has a significant impact on lifestyle and livelihood. A study published in the Journal of Bone and Joint Surgery, found that 74% of those unable to drive due to injury or surgery are dependent on family and most of the remainder depend on friends. 4% of those unable to drive have no help at all and more than 25% suffer major financial hardship.
The report also found that family physicians, orthopedic surgeons, podiatrists, and physical therapists are keenly aware of this dilemma but often fail to communicate effectively to patients about driving. Most medical professionals express serious concerns about liability regarding return to driving following an injury or surgery. They feel that there is a lack of data to support decisions and inadequate communication among each other. They agree that they must do a better job communicating with patients and their families so they can better prepare for a period of time during their recovery in which they cannot drive.
Recent studies published in the Journal of the American Academy of Orthopaedic Surgeons (JAAOS) and the Journal of Foot and Ankle Surgery (JFAS),determined that there are two significant components in the decision of safely returning to driving after an injury or surgery; the time required for healing and the time required for a return of function. Additionally, it was found that those wearing a surgical shoe or walking boot demonstrated a significantly slower braking response time even in healthy/non-injured individuals wearing the shoe/boot.
During the time required for healing, in addition to the fear of an additional trauma from a motor vehicle accident to the healing body part, there is a general concern about the potential damage that may come from over using the body part to drive before it is adequately healed. For example, a healing fracture in the right lower leg might be compromised or delayed if one must suddenly and forcefully apply the brakes. Also, during this time, it is not unusual for post-injury or post-surgery patients to use pain medications, including narcotics. This will also compromise judgment and reaction time while driving.
Most orthopedic conditions heal in 6 to 8 weeks. However, as many of you may fully know, once a cast or splint is removed, you are not ready to run or jump. Depending on the severity of the injury, it may take many weeks of aggressive physical therapy to regain strength, range-of-motion, agility and dexterity to function at a safe level for a full return to daily activities, including driving.
The current research reinforces the fact that driving safely requires good function of the entire body. For example, just because you broke your shoulder bone but did not fracture your right leg does not mean that you are able to drive safely. Wearing a sling after arm surgery also compromises driving. First, you need a stabilized and healed injury prior to driving. Then, you must work in rehab to make modifications to return to safe driving. Apply the same scenario to injuries or surgery to the spine (neck and lower back).
*Based on research using driving simulators
7 TIPS TO KNOW WHEN YOU ARE READY TO DRIVE:
Remember, every case is unique and there is no substitute for communication with your orthopedic surgeon, podiatrist, family physician and physical therapist.
Visit your doctor regularly and listen to your body.
Keep moving, eat healthy foods, exercise regularly, and live long and well!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Injuries due to falling are a very common problem in the elderly. Hip fractures are the most common injury due to falling in the seniors. According to the American Academy of Orthopaedic Surgeons, each year more than 300,000 people are hospitalized for hip fractures in the United States. These fractures represent 72% of all fracture costs, totaling more than 12 billion dollars in 2005 and, not surprisingly, 90% occurred in those 65 and older. Most hip fracture patients who previously lived independently will require family assistance, home or long term care and 50% will require a cane or walker.
A recent study by the American Physical Therapy Association found that patients benefited from a physical therapy evaluation to determine their risk level for falling. If a high-risk level is found on a falls assessment, physical therapy interventions can be successfully employed to improve strength, balance, and coordination and falls prevention. Also, a well-balanced diet, exercise, Calcium with vitamin D supplements and medications can help prevent or retard osteoporosis and prevent hip fractures.
***Always perform slowly, alternate right and left sides, limit other distractions and concentrate on the exercise to retrain the brain, 10-20 times each 2-3 times per day.
***Caution: Do not do standing exercises without assistance or supervision if needed
Face a countertop and hold onto it with both hands. Hike your hip and knee up to 90 degrees as if you are marching. Hold the position for 3-5 seconds on one leg and lower slowly. Repeat this on the other leg and alternate 10 times.

Face a countertop and hold onto it with both hands. Lift your leg up 30 degrees as if you are spreading your legs apart. Hold the position for 3-5 seconds on one leg and lower slowly to cross over the middle. Repeat this on the other leg and alternate 10 times.
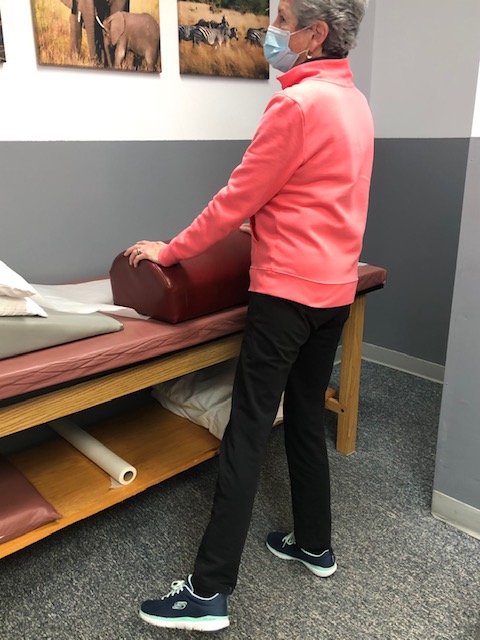
Face a countertop and hold onto it with both hands. Bend your hip and knee down to 45 degrees to a squatting position. Hold the position for 3-5 seconds on both legs and return to standing slowly. Repeat this 10 times. Once strong enough try on one leg at a time and alternate.
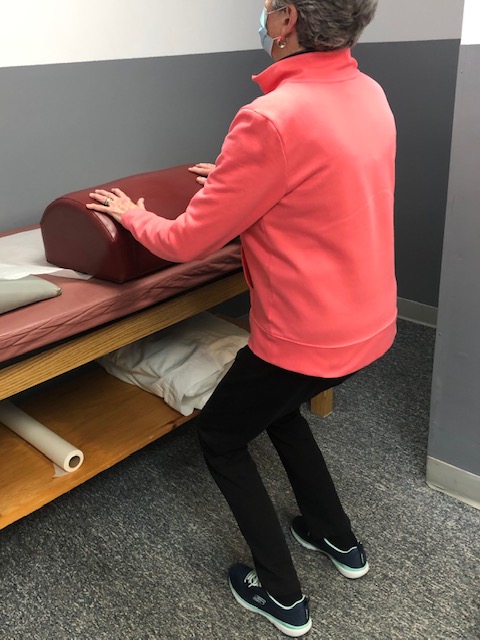
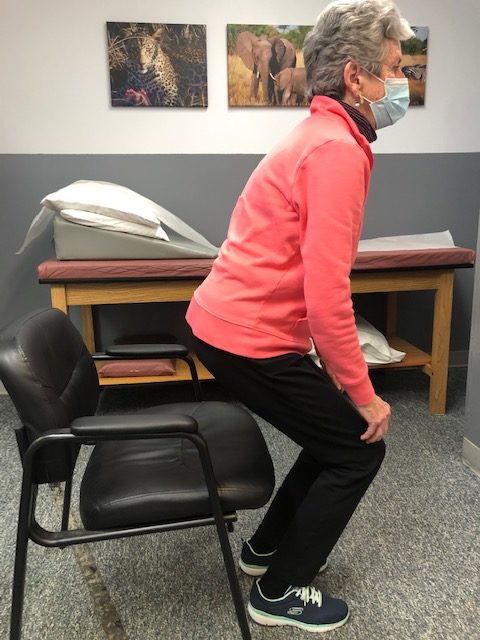
Sit in a chair with arm rests. Get out of chair only using your legs. Hold the position for 3-5 seconds and return to sitting. If necessary, use 1 or 2 arms to assist. Repeat this 10 times. Focus on trunk core stabilization and leg strength. Use more leg muscles and less arm muscles as strength improves.
Place a straight line on the floor and practice “walking the line” with the right then left foot on the line.
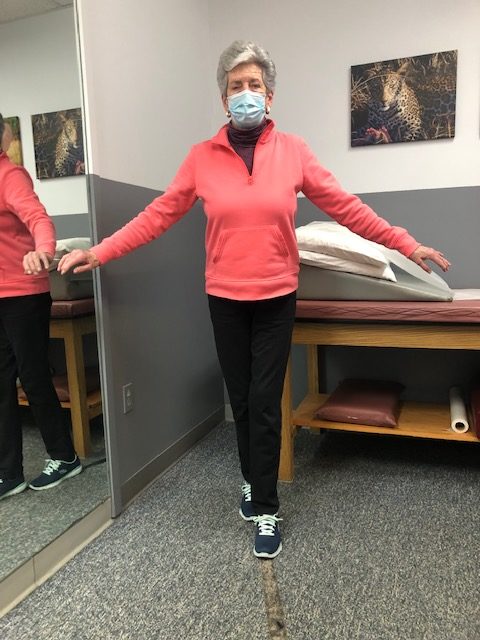
Hold onto a chair while bending one knee and shifting your weight to the other leg. Hold for 3-5 seconds and repeat with the other leg. Increase time 10 -15 -20 seconds as tolerated.

If you feel you or a loved one may be at risk for falling or a hip fracture, ask your family physician if a physical therapy consultation for a falls prevention program to prevent hip fractures may benefit you.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit www.mackareyphysicaltherapy.com/forum
When an older loved one sustains a serious injury it is traumatic for the entire family and mine is no exception. My grandmother and father enjoyed 90 wonderfully active years; however, their independence was lost the same way more than one-third of a million people lose their independence each year… hip fractures! As a doctor of orthopedic physical therapy, I feel remise that I could not prevent this from happening. What most of us fail to realize is that his fracture, like many, was more than just an orthopedic problem …it involves age, gender, diet, exercise, vision, leg strength, medications, environmental risks, and vestibular problems (inner ear problems effecting balance).
Injuries due to falling are a very common problem in the elderly. Hip fractures are the most common injury due to falling in the seniors. According to the American Academy of Orthopaedic Surgeons, each year more than 300,000 people are hospitalized for hip fractures in the United States. These fractures represent 72% of all fracture costs, totaling more than 12 billion dollars in 2005 and, not surprisingly, 90% occurred in those 65 and older. Most hip fracture patients who previously lived independently will require family assistance, home or long term care and 50% will require a cane or walker.
Several risk factors for hip fractures have been identified. While some factors are somewhat controllable and may improve bone quality, (diet, exercise, smoking, alcohol) others are not.
Vestibular or inner ear problems
Preventing a fall can not only save your independence but also your life! Preventing injuries from falls reduces the need for nursing home placement.
NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” Hip Fractures - Part II of II

This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's Articles visit: www.mackareyphysicaltherapy.com/forum