Happy Independence Day! This summer try to think of your pleasure puddle in different light…a health spa! It may very well be the exercise of choice for many people. Many have discovered the benefits of moving their limbs in the warm water of a home pool following knee or shoulder surgery. Also, long distance runners who often look for cross training methods without joint compression and arthritis sufferers who are often limited in exercise choices by joint pain from compressive forces when bearing weight, can enjoy the buoyancy effects of water. These are good examples of the benefits or water exercise…aerobic and resistive exercise without joint compression.
Most doctors recommend some form of exercise with arthritis. Pain and fatigue are the most limiting factors for the person with arthritis. Pool exercise may be the answer. With proper technique, adequate rest periods, appropriate resistance and repetitions, water exercise can be very effective.
Visit your doctor regularly and listen to your body.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit: www.mackareyphysicaltherapy.com/forum
Research shows, those who prepare in advance for their physician visits, have more satisfaction than those who just show up for their appointment. Moreover, for patients seeing multiple physicians, such as specialists, often communication is poor and your participation in the process can be invaluable. There are things you can do to prepare for your physician visits:
Remember, your health is too important to rely on memory for accuracy…so be a proactive participant. With technology, it has never been easier to keep a medical journal to improve accuracy and communication. There are several “Apps” such as “mymedicalapp.com” that allow you to do this on your phone, tablet or lap-top computer and offer privacy code features.
SOURCES: www.webmd.com; National Institutes of Health – National Institute on Aging “A Guide for Older People - Talking With Your Doctor”

This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician.
For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit: http://www.mackareyphysicaltherapy.com/forum
Since 1949 May has been designated as National Mental Health Month for the purpose of eliminating the stigma associated with mental illness by raising awareness. One of the most common mental health conditions is depression. New research from Boston University School of Public Health has found that depression has been increasing in the United States and life with COVID for more than two years has accelerated it rapidly. In 2021 the number of people suffering from depression increased more than 32 percent, affecting 1 in every 3 American adults. However, research also has good news to offer: one of the most understated benefits of exercise is mental health! Specifically, aerobic exercise (exercise that increases your heart rate for 30 minutes or more) such as walking, biking, running, swimming, hiking, elliptical & stepper machines to name a few, is the secret to “runner’s high.” This exercise euphoria is not limited to runners alone, but all who engage in aerobic exercise are more likely to experience high energy, positive attitude, and mental wellness.
Physical activity, specifically aerobic exercise, is a scientifically proven useful tool for preventing and easing depression symptoms. Studies in the British Journal of Medicine and the Journal of Exercise and Sports Science found that depression scores were significantly reduced in groups that engaged in aerobic running, jogging or walking programs, 30-45 minutes 3-5 days per week for 10-12 weeks when compared to a control group and a psychotherapy counseling group.
Depression is the most common mental disorder and is twice as common among women as in men. Symptoms include: fatigue, sleeplessness, decreased appetite, decreased sexual interest, weight change, and constipation. Many of these symptoms are likely to bring an individual to their family physician.
According to research, exercise reduces depression in two ways, psychologically (mentally) and physiological (physically).
Psychological or Mental Benefits of Exercise on Depression:
Physiological or Physical Benefits of Exercise on Depression:
Work hard to recognize and overcome these symptoms to begin an exercise program. An aerobic exercise routine should eventually lessen these symptoms.
Despite a recent surge in Covid cases from the new variant, more than 70 percent of Americans anticipate high levels of enthusiasm for travel this summer. Moreover, travel abroad in 2022 is expected to exceed pre-pandemic levels, as isolation weary Americans take to the air!
Confession; I recently was on a long trip that required sitting on an airplane for more than six hours…and I wore compression stockings … guess I’m getting older (and wiser)!
Have you noticed that being in a car or on an airplane for more than three hours leads to neck and back pain? Soreness, stiffness and swelling in your legs? With a little planning preventing or limiting these problems on long trips, is possible. Also, as people age and/or develop other health problems, they are more vulnerable to develop a more serious problem associated with long trips; deep vein thrombosis (DVT) or blood clots. But problems from long-distance travel can be avoided. The following tips, based research and personal experience, can prevent neck, back and leg pain and stiffness and DVT.
A DVT is a blood clot that forms in a deep vein. The deep veins pass through the muscles and cannot be seen like the veins just under your skin. While it may occur in your arms, it is much more common in the legs, especially the calf muscle when traveling. When a blood clot forms in a leg vein it usually sticks to the vein wall. Often, pain and swelling lead you to the doctor and treatment is rendered before serious complications develop. However, there are two possible complications. One, a pulmonary embolus, occurs when a part of the clot logged in your deep vein of the calf breaks off and gets lodged in the lung. This is a very serious problem that can be fatal. Two, post-thrombotic syndrome, occurs when you have pain and swelling in the calf after a DVT.
The following risk factors for DVT significantly increase the potential for problems when traveling on long trips by air more than 5 hours. Trains, cars and buses also create a risk, but air travel creates a greater risk for the following reasons: reduced cabin pressure, reduced cabin oxygen levels, dehydration and alcoholic drinks, which may increase dehydration and immobility.
health
Airplane seats are “C” shaped and force you to round your neck and back forwards. These exercises are designed to stretch and extend your back in the opposite direction. Please perform slowly, hold for 3-5 seconds and repeat 10 times each hour.
When sitting in an airplane seat, take the neck pillow in the overhead compartment and place it in the small of your lower back. While sitting or standing up, perform postural exercises every 30-45 minutes.
NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
The last two columns in “Health & Exercise Forum” have been dedicated to the health benefits of exercise for Parkinson’s disease. Specifically, the use of dance was featured as a method to promote strength, balance, coordination and agility in this population. However, dance as a form of exercise and for the promotion of balance, coordination and agility, is not limited to those with neurological conditions…it is beneficial for everyone! In fact, my wife, Esther and I, have always enjoyed our dance classes with Vince Brust!
Like most forms of exercise, if done regularly, dance can have multiple health benefits. If dance is your only form of exercise, make it your goal to sustain the activity for about 30 minutes a day, 3-4 days per week for the most value.
If you have any doubt or reservations about the ability of dance to improve your health and wellness, take notice of the muscle tone, flexibility, agility and coordination of a professional dancer...ballet, modern, hip hop, jazz, etc. They are incredible athletes and artists!
It is common to lose agility and flexibility with age especially if you regularly perform the same limited movements throughout your day and lifetime. This will lead to stiffness and lack of flexibility, especially for new or season activities which can make you more vulnerable for injury and pain. Lower back pain and calf or hamstring strains are most common. Research suggests that dance can help.
For example, in one study it was found that cross-country skiers who received months of dance training showed improvements in joint mobility and muscle flexibility of the spine, as well as their speed and agility.
It is also expected that balance and coordination are also compromised with age. It’s one of the reasons that older adults are so prone to falls. The research also supports the value of dance to offset this problem.
One particular study found that in people over the age of 80 years, social dancing helped improve balance and walking speed, as well as contributing to a more stable walking pattern.
Moderate-intensity dance, performed continuously for at least 30 minutes on a regular basis has been found to reduce the risk of death from cardiovascular disease in some studies. Moreover, it has been more effective in prevention than average-pace walking ...and is less boring!
Most activities of daily living (walking, climbing stairs) occur in a linear and forward directon. However, dance has not set direction and can move in multiple planes (forwards, backwards, and sideways with diagonal and rotational components.
These unlimited movements, not only improves agility, coordination, and balance, but also strengthens muscles that often get forgotten like your core and abdominals.
As with any cardiovascular exercise, dance is a form of aerobic exercise which burns calories. This is especially true if performed a minimum of moderate-intensity for 30 minutes or longer.
According to the American Diabetes Association, aerobic exercise can support weight loss.
Weight-bearing exercise is the cornerstone for any osteoporosis prevention program and dance is a prime example.
According to the National Osteoporosis Foundation, high-impact, weight-bearing exercises, such as certain forms of dance, can help maintain bone strength and even build new bone mass. This slows the development and progression of osteoporosis. It is also well established that low-impact weight-bearing exercise (dancing with the impact of jumping etc.) is effective in bone loss prevention. Dance can be whatever intensity you want it to be, depending on your mood, energy level, and physical limitations.
Like most forms of exercise, especially aerobic, dance can improve cognitive health. In addition to releasing special hormones, it can also improve circulation and oxygenation to the brain to enhance brain health.
Some research suggests that dance can help create new connections between brain regions involved in long-term memory and improve mood, cognitive acuity and mental energy.
Physicians and physical therapists often recommend dance as a form of rehabilitation following brain injury, stroke or dementia.
One study found that out of many different types of exercise (including dance, swimming, golf, cycling, tennis, and others) dance was the only one associated with a lower risk of dementia for people in the study. Experts believe the benefit was due to a combo of social interaction and mental focus...that is not to say that the aforementioned types of exercise do not have value.
Dancing can contribute to your mental health by improving mood and reducing stress. As Morrie advised in Mitch Albom’s best-selling book, Tuesdays with Mori, “dance like nobody’s watching”...it can be very invigorating!
Dance participants ranked mood enhancement as the number one reason for participation! One study examining people’s motivation for dancing, “mood enhancement” ranked top on the list. The dancers felt that the activity is expressive and allows you to escape and “let your hair down.”
Some studies also suggest that dance therapy might also reduce depression, especially in those who have serious illnesses, such as breast cancer or Parkinson’s (read last week’s column). Researchers feel that this may be due to increased endorphins and lower cortisol levels.
The pandemic has taught most of us a valuable lesson ... some of us have a serious need to socialize and some do not. For those like me, who thrive on being among others, dance classes and dance-style workouts often take place in groups, which allows for social bonding in a fun, light and breezy environment.
Depending on your marital status and the specific style of dance you choose (salsa, tango or swing dancing), you may even be paired up with a partner every week!
While exercise on treadmill, bike or elliptical can be great exercise, it also can be boring and repetitive. Research suggests that any form of exercise can boost self-esteem.
When dancing, however, you get all the benefits of exercise, while simultaneously learning a new skill. It can be incredibly rewarding and satisfying to master the skill, especially with others such as learning the tango.
SOURCE: “Greatest” Debra Sullivan, Ph.D., MSN, R.N., CNE, COI

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.comPaul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine GCSOM.
For all of Dr. Mackarey's articles visit www.mackareyphysicaltherapy.com/forum
Parkinson’s disease (PD) is a chronic, degenerative disease that leads to slowness of movement, balance disorders, tremors, and difficulty walking. PD results from the loss of dopamine-producing nerve cells in the brain. Dopamine is critical to stimulate the nerves of the muscular system in the body. PD affects approximately 1.5 million people in the USA with 60,000 new cases each year according to the National Parkinson Foundation. Most people know someone affected by PD. PD typically affects those over 65 years of age and only 15% are under 50. However, actor, Michael J. Fox brought national attention to the disease in 1991 when he was only 30 years old. Juvenile Parkinson’s, those diagnosed under the age of 40, is rare and only represents 7% of all those with PD.
While there is no current cure for PD, exercise can relieve some of its symptoms. Although PD affects an individual’s ability to move, exercise can help keep muscles strong, joints mobile, and tissues flexible. Exercise will not stop PD from progressing, but it will improve balance, enhance walking ability, reduce muscle weakness, and minimize joint stiffness. In 2007, a study published in the Journal of Neuroscience revealed that exercise will benefit individuals with PD because exercise encourages the remaining dopamine cells to work harder to produce more dopamine. Also, the researchers discovered that exercise decreases the rate at which dopamine is removed from the brain.
Depending on the stage of the disease and the level of assistance required, exercise to improve strength, balance, flexibility and ambulation for those with PD, can be performed independently at home or supervised at a rehab or fitness facility. Supervised exercise can include physical therapy, recreational therapy, water therapy, yoga, and Tai Chi… AND DANCE! Physical therapy can improve walking ability, enhance balance, reduce fatigue, increase strength, promote flexibility and minimize pain. Physical therapy uses movement techniques and strategies as well as various pieces of equipment to enhance an individual’s level of independence and improve his quality of life. Recreational therapy incorporates leisure activities (e.g. golfing and ballroom dancing) to reduce the symptoms and associated limitations of PD. Recreational therapy adapts these activities to meet the specific needs of the person with PD. The modified activities are taught by professionals who have significant knowledge and experience in this area. Water therapy is especially helpful to people with PD because the water provides enough buoyancy to lessen the amount of balance required to perform essential exercises. The cushioning effect of the water allows for freedom of movement while providing the appropriate level of resistance necessary to achieve the desired results. Using a combination of physical and mental exercises, yoga promotes flexibility, reduces stress levels, and increases stamina and strength in individuals with PD. Tai Chi, a total mind and body workout, and is a series of individual dance-like movements linked together in a continuous flowing sequence. Particular benefits for people with PD include reduced stress, increased energy, improved concentration and focus, better circulation and muscle tone, and significant improvements in balance.
If you choose the convenience of a home exercise program, consult your physician or physical therapist for recommendations regarding: (1) the types of exercise best suited for you and those which you should avoid, (2) the intensity of the workout, (3) the duration of your workout, and (4) any physical limitations you may have.
The type of exercise that works best for you depends on your symptoms, fitness level, and overall health. Your exercise program should address not only strength but also flexibility and endurance and should include all body parts: face, mouth, neck, torso, arms, legs, hands, and feet. Some general exercise suggestions include:
Since individuals with PD are at risk for falling and freezing (becoming rigid), work out in a safe environment and, if possible, when someone is present. Avoid slippery floors, poor lighting, throw rugs, and other potential dangers (e.g., watch out for the pooch because he might want to join in the fun). If you have difficulty balancing, exercise sitting down, lying on the bed or within reach of a grab bar or securely installed rail. Stop and rest if you feel tired during your exercise program since overexertion can make your PD symptoms worse.
Contributions: Janet Caputo, DPT, OCS,

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” Next Week: Part II of II: Dance for Parkinson ’s Disease.
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.comPaul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit: http://www.mackareyphysicaltherapy.com/forum
In 2000, President Bill Clinton dedicated March as National Colorectal Cancer Awareness Month. The purpose of this designation is to increase public awareness of the facts about colon cancer – a cancer that is preventable, treatable and has a high survival rate. Regular screening tests, expert medical care and a healthy lifestyle, which includes a proper diet and exercise, are essential for prevention. Several studies have demonstrated that exercise can also help prevent colon cancer.
The American Cancer Society estimates that there will be approximately 150,000 new cases of colorectal cancer in 2021. Of these, 52,980 men and women will succumb to the disease. It is the second-leading cause of U.S. cancer deaths for both men and women combined. The good news is incidence and mortality rates are dropping both nationally as well as in northeast Pennsylvania. The bad news is northeast Pennsylvania still has increased incidence and mortality rates when compared to the national average.
Studies show that prevention of this disease is multifaceted and includes: engaging in daily exercise, eating a low-fat diet with little red meat, avoiding smoking, drinking in moderation and having regular colonoscopy screenings.
Early detection is the key to survival. Death from colorectal cancer can be eliminated if caught at the earliest signs of disease. Colorectal cancer progresses very slowly, usually over years. It often begins as non-cancerous polyps in the lining of the colon. In some cases, these polyps can grow and become cancerous, often without any symptoms. Some symptoms that may develop are: blood in stool, changes in bowel movement, feeling bloated, unexplained weight loss, feeling tired easily, abdominal pain or cramps, and vomiting. Contact your physician if you have any of these symptoms.
The risk of colon cancer increases with age, as 90 percent of those diagnosed are older than age 50. A family history of colon cancer increases risk. Also, those with benign polyps, inflammatory bowel disease, ulcerative colitis or Crohn’s disease are at greater risk and should be screened more frequently.
The intestine works like a sewage plant, recycling the food and liquid needed by your body. However, it also stores waste prior to disposal. The longer the wastes remain idle in your colon or rectum, the more time toxins have to be absorbed from you waste into the surrounding tissues. One method in which exercise may help prevent colon cancer is to get your body moving, including your intestines. Exercise stimulates muscular contraction called peristalsis to promote movement of waste through your colon.
Exercise to prevent colon cancer does not have to be extreme. A simple increase in daily activity for 15 minutes, two times per day or 30 minutes, once per day is adequate to improve the movement of waste through your colon. This can be simply accomplished by walking, swimming, biking or playing golf, tennis or basketball. For those interested in a more traditional exercise regimen, perform aerobic exercise for 30-45 minutes four to five days per week, with additional sports and activities for the remainder of the time. For those in poor physical condition, begin slowly. Start walking for five to 10 minutes, two to three times per day. Then, add one to two minutes each week until you attain a 30-45 minute goal.
Dr. Christopher Peters is a partner of Radiation Medicine Associates of Scranton (RAMAS) and serves as medical director of Northeast Radiation Oncology Centers (NROC). He is an associate professor of clinical medicine at GCSOM.
Sources: American Cancer Society/Northeast Regional Cancer Institute, and CA Cancer J Clin.

This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
More than 65 million people, almost 30% of the population in the United States, are actively involved in providing 20 or more hours of care for a chronically ill, disabled, or aged family member or friend each week. As our population continues to age, this number is expected to grow rapidly.
The role of a caregiver is multifaceted and often involves tasks and skills beyond the education or comfort level of most providers. Some examples include; managing money, paying bills, shopping, cleaning, maintaining and repairing a home, dispensing and injecting medications, cleaning wounds, changing dressings, catheter management, bed baths, assisting in position changes, transferring from the bed to the chair, ambulation, stair climbing, bathroom assistance for toileting and showering and many other responsibilities. Consequently, a caregiver is often at risk for mental, spiritual and physical fatigue or breakdown. It is no surprise that depression, illness and injury often plague a caregiver and eventually, the caregiver is in need of a caregiver. One of the most common injuries suffered by a caregiver is back pain.
Lower back pain (LBP) is one of the most common problems in our society. Over 90% of all Americans will suffer from it at least once in their lives. It is generally agreed that prevention is the best treatment for LBP.
As little as 10 extra pounds puts great stress on your lower back. It also makes it more difficult to maintain good posture. Eat well and exercise regularly.
Aerobic exercise will help prevent weight gain and stiffness for a healthier lower back. It will also help with the stress and depression associated with providing care for a loved one. Perform mild aerobic exercise such as walking 3-5 times per week for 30-45 minutes. You can also use an elliptical or bike at home while your loved one is resting. Get outdoors and take multiple short walks …go around the block a few times per day.
Core stabilization exercises designed to strengthen the abdominal and lower back muscles will help prevent injury. Some examples of core exercises are:
Pelvic Tilt - lying on your back and performing a pelvic tilt as you flatten you lower back into the floor.
Pelvic Tilt and Heel Slide - lying on your back, hold a pelvic tilt as you slide your one heel up and down and repeat with the other heel.
Core on Ball - Perform arm exercises such as biceps and triceps with light weight while sitting on a therapeutic ball while simultaneously trying to hold an isometric contraction of your abdominal and lower back muscles.
Smoking effects natural healing because it constricts the small blood vessels. Smokers have a much higher incidence of LBP and failure from lower back surgery.
Good posture is critical for a healthy back. When sitting, standing or walking maintain a slight arch in your lower back, keep shoulders back, and head over your shoulders. In sitting, use a towel roll or small pillow in the small of the back.
Caregivers spend much of the day with their spine bent over a bed or chair feeding, bathing, and lifting a loved one. Postural exercises are designed to stretch your back in the opposite direction of this forward flexed position. Examples include:
Bend your knees, maintain an arch in the back with head up, and bend over as little as possible. Bend the knees of your loved one; roll their trunk toward you to get their legs over the edge of the bed as you pivot their weight on their butt to get them sitting upright.
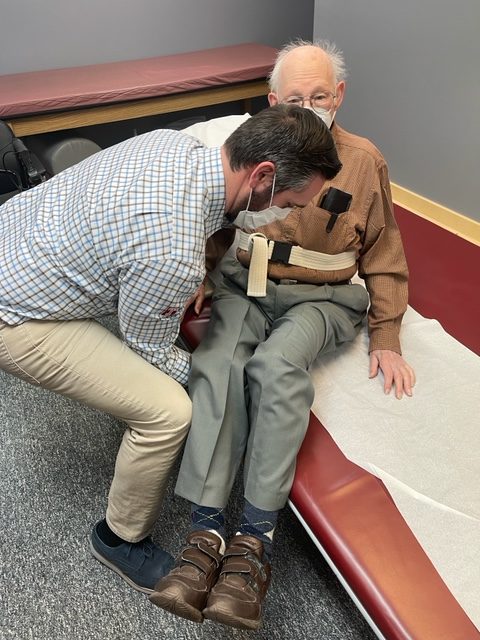
Bend your knees, maintain an arch in the back with head up, and bend over as little as possible. Place your hands around the waist or on a transfer belt. Use your legs, turn with feet, and do not twist spine. Block the feet and knees of your loved-one with your feet and knees and use them to pivot and transfer from the bed to the chair. Be sure the chair is along side of the bed and arm of chair removed if possible before the lift.
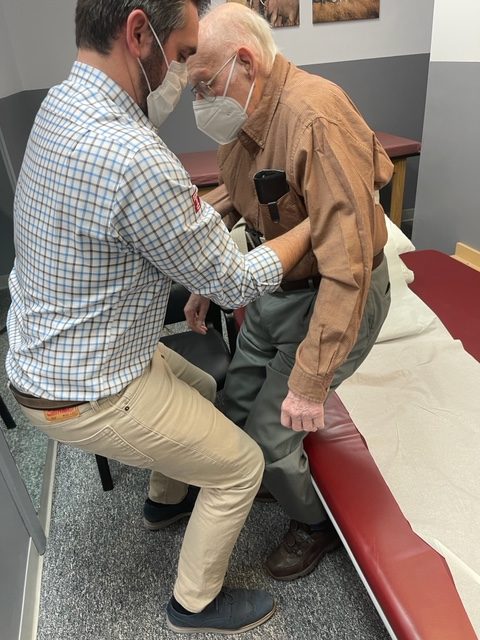
Transfer Belt - Use a transfer belt around the waist of the patient. Grip the transfer belt, instead of the patient or clothing, during the lift or when ambulating. Lower Back Lifting Belt - Also, if you have a back problem, consider using a lifting belt or back brace to protect your back when lifting the patient. Immediately following the lift, stand up straight and stretch lower back into extension.
Transfer belts and lower back lifting belts can be found online or at your local pharmacy.
Lift Chair – For patients that require maximum or moderate assistance and only one caregiver is available to lift or transfer, an electric lift chair should be considered.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice in downtown Scranton and is an associate professor of clinical medicine at GCSOM.
Visit your doctor regularly and listen to your body.
For all of Dr. Mackarey's articles visit: https://mackareyphysicaltherapy.com/forum/
You are never too old to exercise! This is the second of two columns dedicated to appropriate exercise for the elderly. Last week I discussed basic strengthening exercises. This column will address three additional components necessary for independence in the elderly: flexibility, balance and endurance. While it may not be as valuable for those fortunate to be over 75 years of age and capable of running, skiing and playing tennis, you may still find a noteworthy pearl of wisdom.
Why would someone 75 or 80 be interested in a basic exercise program? Well, one must maintain adequate flexibility, strength, balance and endurance to safely function in daily activities around the house. For example, the most common goals of elderly patients are: climbing stairs, getting in and out of a shower, putting on shoes and socks, tucking in a shirt or fastening a bra, cooking, cleaning, and carrying groceries or laundry.
Remember, for most people it is more harmful not to exercise, so contact you physician to discuss whether independent exercise is appropriate for you. You may need to consult with a physical therapist to get started.
Flexibility Exercises involve moving the arms, legs and trunk through comfortable range of motion to give you more mobility in order to improve your ability to perform daily activities such as tucking in a shirt, tying shoes or fastening a bra. Best if performed after strength exercises because the muscles and joints will be warm and limber. Always perform slowly with slight stretch sensation and no pain. No bouncing or over stretching!
These exercises are to be performed while sitting in a chair with a backrest, slowly, 5 repetitions, 3-5 times per week.
Balance Exercises involve strengthening muscles that keep the body upright and stable in standing in order to improve your ability to perform daily activities without falling. According to the NIH, 300,000 US hospital admissions for broken hips occur each year due to falls. Check with your physician if you have a history of dizziness before performing these exercises on your own. Best if performed with someone at home or some assistance. Always use a countertop or back of chair to hold onto for support.
Endurance Exercises involve any activity such as walking, swimming, biking or raking leaves that elevates your heart rate and breathing for an extended period of time. Check with your physician if you have a history of heart problems or dizziness before performing these exercises on your own. Best if performed with someone at home or some assistance. Start off slowly for only 5 minutes and add 1-2 minutes each week or 2. Wear good and comfortable shoes – no heels!
While not all of these endurance exercises may be appropriate for you, one or two of these may offer a good starting point.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate profession of clinical medicine at Geisinger Commonwealth School of Medicine.
For all of Dr. Mackarey's articles visit mackareyphysicaltherapy.com
You are never too old to exercise! A reader who described herself as “elderly” asked me if she was too old to exercise. Without knowing her age, I replied that she was not. I did qualify my response with the fact that exercise must be adjusted to meet the individual needs of a person based on age, health status and goals. Her question, however, led me to think of the many “elderly” who may be apprehensive to begin an exercise program for a variety of reasons. Fear of injury and lack of information may be two reasons. Another reason, according to this inquiry, is the fact that so many exercise programs featured in the media are geared to the young and healthy or baby boomers and few focuses on the needs of those over 75, home bound and weakened by age and inactivity. Those running, biking, skiing, golfing at 75 and over and do not fall into this category, please do not be offended, you are the exception. God bless you!
Why would someone 75 or 80 be interested in an exercise program? Well, one must maintain adequate flexibility, strength, balance and endurance to safely function in daily activities around the house. For example, the most common goals of elderly patients are: climbing stairs, getting in and out of a shower, putting on shoes and socks, walking safely for functional distances, tucking in a shirt or fastening a bra, cooking, cleaning, and carrying groceries or laundry.
The National Institute of Health (NIH) recommends four areas of concentration for elderly persons to concentrate on in order to maintain safety and independence: strength, flexibility, balance and endurance. It will be the purpose of this column to recommend safe, practical and easy exercises that focus on each of these categories.
Remember, for most people it is more harmful not to exercise, so contact your physician to discuss whether independent exercise is appropriate for you. You may need to consult with a physical therapist to get started.
Strength Exercises involve using the muscles to move the arms and legs against resistance such as a weighted object, dumbbells, resistance bands, and body weight against gravity. Strength is necessary to perform daily activities such as walking, lifting a ½ gallon of milk, transferring to a shower or chair safely.
These exercises are performed while sitting in a chair with backrest, slowly, 5 -10 repetitions, and 3-5 times per week. No weight is used in the beginning, only the weight of the arm against gravity. In 1-2 weeks a light 1-2 pound weight and light resistance band may be added.
Once you have mastered these exercises against gravity, then advance to using light weights or light resistance bands. Ankle weights are very inexpensive and can be purchased in 1 pound increments. Light resistance bands are available in yellow and red in colors.
Visit your doctor regularly and listen to your body.
Keep moving, eat healthy foods, exercise regularly, and live long and well!

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” Next Week: Never To Old To Exercise – Part II of II
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate profession of clinical medicine at Geisinger Commonwealth School of Medicine.
For all of Dr. Mackarey's articles visit http://mackareyphysicaltherapy.com/forum