I have been advising my patients to exercise, keep active, and walk as long as they can in order to stay mobile and healthy. However, seniors often tell me activities that require prolonged walking is limited by ankle pain from arthritis. They often ask, “What is arthritis of the ankle?” How does it happen? What can I do about it?
Your family physician will examine your ankle to determine if you have arthritis. In more advanced cases you may be referred to a specialist such as a podiatrist, orthopaedic surgeon or rheumatologist for further examination and treatment. X-rays will show if the joint space between the bones in the ankle is getting narrow from wear and tear arthritis. If rheumatoid arthritis is suspected, blood tests and an MRI may be ordered. The diagnosis will determine if you problem if minor, moderate or severe.
In the early stages your treatment will be a conservative, nonsurgical approach, which may include; anti-inflammatory medication, orthopedic physical therapy, exercise, activity modifications, supplements, bracing, etc. You and your family physician, podiatrist, orthopedic surgeon or rheumatologist will decide which choices are best.
When conservative measures no longer succeed in controlling pain and deformity, improving strength and function then more aggressive treatment may be necessary.
SOURCES: Rothman Institute, Philadelphia, PA and American Academy of Orthopaedic Surgeons
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Human beings were designed to move…walk, run, climb, lift, hunt, and gather. Contemporary man has suffered greatly from a technologically driven inactive and sedentary lifestyle. Inactivity is associated with many health problems; obesity, adult-onset diabetes, high blood pressure to name a few. The problems associated with lack of movement are many:
The more you move your body, the more you colon moves! A regular and consistent exercise and activity regime, results in a more consistent bowel schedule, especially with age. Healthy muscle tone in your abdominal muscles and diaphragm is also the key to moving waste through your digestive tract.
Osteoarthritis, rheumatoid arthritis and many inflammatory or auto-immune diseases can cause achy and stiff joints. However, even healthy joints can also stiffen when you don’t use them enough. Put them to work so they don't get tight and cause pain.
All muscles get weak from lack of use, including the muscles that help your lungs expand and contract as you breathe if you don’t work them out regularly. The less exercise or activity you do, the more you experience shortness of breath, even during easy daily tasks.
Physical problems are not the only complication of inactivity. A lack of movement can also increase feelings of anxiety and depression. Aerobic exercises like walking, biking, swimming, or running, have been proven to stimulate endorphins to boost and steady your mood, and even improve your self-esteem.
Many studies have found that regular movement improves energy. Exercise helps deliver oxygen and nutrients to your tissues. When you sit or are inactive, tissues are not getting the same amount of fuel they need to keep you going.
Movement stimulates your metabolism. Hyperactive people burn more calories…just by fidgeting! Even if you are not hyperactive, the more active you are, the more calories you burn each time you move.
One of the first recommendations sleep doctors make to their patients suffering from insomnia is exercise. When you keep a regular exercise routine, you fall asleep faster, and you sleep deeper once you drift off.
Regular exercise tells your body to make more chemicals called growth factors. They boost blood vessel production in your brain. The more blood that gets to your brain, the better you can think, remember, and make decisions.
Spending most of your time sitting raises your risk of heart disease, in great part due to the fact that partly you’re more likely to have high blood pressure. This is a big risk factor for heart issues like coronary artery disease and heart attack.
When physical activity is a regular part of your life, your body has an easier time keeping your blood glucose under control. Exercise can stabilize blood sugar levels and keep you out of the type 2 diabetes danger zone.
When your core muscles are weak from lack of use, they can’t support your back the way they should. This makes it much easier to tweak your back muscles during everyday movements like standing or reaching. Pilates, yoga, and other exercises that use stretching are good for building a stronger back. Schedule an appointment with a good orthopedic and sports PT.
Logically, one might think that you’d be hungry more often if you exercised more, but the opposite is usually true. Aerobic exercise like biking, swimming, walking, and running can actually decrease your appetite because it changes the levels of certain “hunger hormones” in your body.
Studies show the more moderate activity you get, the lower your chance of catching a cold or other germs. When you make exercise a habit, your immune system gets stronger.
If your skin looks duller than usual, a lack of movement may be to blame. Some studies show that moderate exercise boosts your circulation and your immune system, which helps your skin keep that youthful glow.
SOURCE: WebMD

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
June is migraine and headache awareness month! According to the World Health Organization about half of the world’s adult population has had a headache at least once in the past year. Prolonged use of electronic devices has greatly contributed to this problem. For many people, these headaches are infrequent and do not often affect daily life. But what about when your headache occurs frequently or is so severe it prevents you from going about your day to day activities? Some types of headaches are more easily treated and managed than others.
There are two types of headaches: primary and secondary. Primary headaches occur without an underlying disease and include migraines and tension-type headaches. Secondary headaches can be associated with serious disease, requiring emergency care, or can be referred from other structures of the body such as the cervical spine (neck).
Headaches symptoms that may constitute a medical emergency are: vomiting, seizures, fever, muscle pain, night sweat, weight loss, and neurologic symptoms such as blurred vision. If you are experiencing any of these symptoms, if your headache worsens, or your symptoms change it is recommended that you seek medical attention. Any headache that is unusual for you and does not resolve itself in a reasonable time should be brought to your primary care physician’s attention.
Migraines: Migraines are a primary form of headache that typically lasts from four to seventy two hours, can range from moderate to severe pain, and typically are located on only one side of the head. Often they can be accompanied by an aura, nausea or vomiting, sensitivity to sound, or light sensitivity. Migraines can be aggravated by routine physical activity such as going up stairs. This type of headache is thought to occur in the central nervous system.
Tension-type: Tension-type headaches are the most common primary headache disorder and can last anywhere from thirty minutes to seven days. These can often have a pressing or tightening quality that occurs on both sides of the head. Typically, there is no nausea, vomiting, or aggravation with physical activity, however, light or sound sensitivity can occur. This type of headache is thought to occur in the central nervous system but can have a hereditary component and is usually associated with muscle tender points. Tension – type headaches can be treated with relaxation techniques such as Progressive Muscle Relaxation (PMR), medications, and physical therapy.
The most common secondary headache that is not related to a serious medical condition is a cervicogenic headache (originating from the neck).
Cervicogenic Headache: The length of time a cervicogenic headache can last varies. Here the pain is on one side and usually starts in the neck. This type of headache is aggravated or preceded by head postures or movements of the neck. Due to the nerves of the neck and face sharing common connections, pain signals sent from one region can lead to discomfort in the other. Physical therapy can be an effective treatment to help relieve symptoms. For example: posture, exercise, ergonomics, massage, manual techniques, traction, trigger point, and acupressure.
A cervicogenic headache can be caused by an accident or trauma or can stem from neck movement or sustained postures. Sustained postures could mean sitting in front of a computer at work or looking down at your phone. Changing these postures throughout the day could help reduce symptoms. Changing postures could mean bringing your phone closer to you using pillows or another supportive surface when reading or checking social media. If you are someone who works at a desk, it could involve taking breaks or getting a standing desk. However your life requires you to move, there are some simple and effective exercises you can perform throughout the day to help cervicogenic headache symptoms.
Progressive Muscle Relaxation: PMR is an effective method for reducing tension throughout the body. With this method you first tense a muscle group, such as at the neck or shoulder, and then relax the muscles noting the difference between the two. This helps reduce both stress and tension. For more information or to learn how to do PMR, refer to podcast at: https://www.psychologies.co.uk/try-progressive-muscle-relaxation
Manage your stress level: While stressors vary from person to person, one method for managing stress is with exercise. Any form of exercise can help reduce stress, but a cost free method is aerobic exercise such as walking or running. A less time consuming method could be to perform deep breathing exercises throughout the day.
Heat or cold: When feeling sore or stiff, applying a hot or cold pack or taking a hot shower can help ease a tension headache.
Posture: Some tips for posture are to make sure your head is over your shoulders rather than sitting forward and making sure you are sitting or standing up straight with your shoulders back.
Over the counter medications: Talk to your doctor or pharmacist for additional information.
Posture: See tips listed under tension headaches.
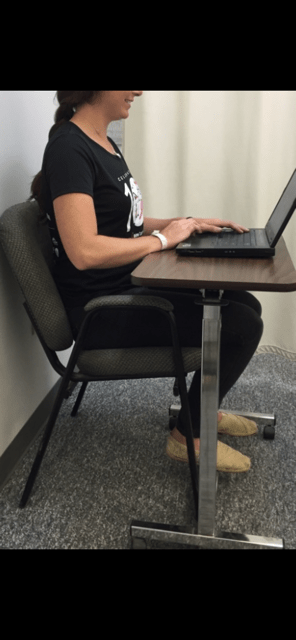
Ergonomics: If your job or hobbies require you to sit for extended periods it may be beneficial to change positions throughout the day or consider getting a standing desk. Also, limit time on electronic devices. When sitting make sure the monitor is at eye level, your legs are able to fit under your desk, and you are close to the keyboard and monitor. If you are working with a laptop or phone, avoid putting it on your lap. Instead, bring your laptop closer to you by putting pillows on your lap or using an ergonomic desktop. See photo below.
Exercise: Some exercises to help relieve symptoms are chin tucks, shoulder blade pinches, and back extension. These exercises can be performed multiple times throughout the day in sitting or standing.
Physical Therapy: Physical therapy may include massage, manual techniques, stretching, traction/ decompression and exercise. A physical therapist can assess your posture and provide strategies specific to you.
Over the counter medications: While medication may not cure cervicogenic headaches, they may help relieve pain. Talk to your doctor or pharmacist for additional information.
Visit your doctor regularly and listen to your body.

Dr. Chua is a neurologist and headache specialist at Geisinger Health System in Northeast Pennsylvania. In addition to caring for people with headache and facial pain disorders, Dr. Chua also serves as: Director of Headache Medicine at Geisinger, Clinical Director of Neurology at Geisinger Wyoming Valley, faculty at Thomas Jefferson University’s Advanced Headache Diagnosis and Management Post-Graduate Certificate Program, and Treasurer and Executive Board Member of the Association of Migraine Disorders. In her spare time, she enjoys going on adventures with her husband and toddler, learning new skills (she is now certified in battlefield acupuncture), and buying great books she will never have time to read!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
We’ve all heard it before – encouragement to exercise to trim our waistline or to speed up our metabolism. However, there may be more benefit to lacing up those sneakers than you’d think. Recent studies have established a link between exercise and cognition, making physical activity even more important.
Exercise has been shown to improve sleep and mood, decrease stress, and even increase libido. It also can bolster our self-esteem and ability to problem-solve and to remember details. In fact, strength training has even been shown to reverse cognitive decline to a degree in aging adults with mild impairment. Though the medical community is still trying to elucidate exactly how exercise boosts our brains physiologically, increased circulation to the brain and modulation of the hypothalamus-pituitary-adrenal axis that regulates the body’s response to stress have been implicated as the bearers of benefit. While exercise can be advantageous for everyone, it perhaps is even more valuable to those struggling with mood disorders. Exercise can help combat anxiety and depression and quell the symptoms of Attention Deficit Hyperactivity Disorder and Post Traumatic Stress Disorder as it helps the brain to pump out neurotransmitters and pain-fighting endorphins. Exercise makes addiction management easier, as well, and has recently been shown to help alcoholics lessen consumption.
So, how much exercise exactly is enough to illicit tangible cognitive benefit, you ask? Any amount of weight lifting, running, walking, or yoga helps, but habitual activity helps the most. Studies cite that a few consecutive weeks of participation in a fitness regimen yielded notable, positive results in subjects. Try to make exercise part of your daily routine to encourage good fitness habits. If you find the idea of adopting a strenuous new fitness program intimidating or off-putting, have no fear. Moderate exercise is enough to do the trick. The Mayo Clinic cites both brisk walking and mowing the lawn as examples of moderate activity, so an average fitness level is adequate for yielding positive mental results.
If you’re thinking about beginning an exercise program for the first time, start gradually. Begin with walking for 10 to 15 minutes twice daily, and add 1 or 2 minutes to your session every time you walk until you can walk continuously for 45 to 60 minutes. The same principle can be used when beginning other fitness routines involving biking, swimming, running, etc. Begin a weight training program to strengthen bones and tendons using 3 to 5 pound dumbbells, and increase the weight you use by a pound once you can easily perform 30 consecutive repetitions. Be careful to pay close attention to posture and form. Contact your physical therapist or a personal trainer for assistance with designing an appropriate exercise program. Don’t hesitate to contact your physician, either, if you have questions about whether a particular exercise program is safe and suitable for your age group or current fitness level. Consider these tips to make the most of your workout:
Guest Contributor: Leanne Woiewodski, MD, graduate, GCSOM
Sources:
US National Library of Medicine, National Institutes of Health, Helpguide.org, IDEA Health & Fitness Association, Mayo Clinic, Public Library of Science

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Spring is here! So, too, is allergy season and spring sports! It seems this every year at this time a young little league baseball player wheezes as they cross home plate and desperately tries to catch their breath. Players, coaches, umpires, parents watch in dismay, deciding whether they need to call an ambulance. Minutes later the player recovers from this scary situation…until the next time. Could this be an example of exercised-induced asthma (EIA)?
Dr. Gregory Cali, a local pulmonologist, (lung doctor) was gracious enough to participate in an interview about this problem…exercise-induced asthma (EIA). The topic was chosen in response to an email question from a concerned mother of an athlete with asthma. Dr. Cali informed me that the first thing to know about exercise induced asthma (EIA) is that EIA is not a distinct disease in itself-but is one manifestation or presentation of asthma. Putting it simply, EIA occurs in patients who have develop narrowing of the bronchial tubes ( bronchoconstriction) when they exercise. Some experts would rather we use the phrase exercise induced bronchoconstriction which is what happens when someone has an asthma attack. This bronchoconstriction occurs because of spasm of the tiny muscles of the airways, plugging of the airways with thick mucous, and swelling or edema of the cells lining the airways.
In fact, it is inflammation of the airways, mostly due to allergies, that is at the root of most cases of asthma. This inflammation causes the bronchial tubes to become over-reactive-and predisposed to narrowing- when exposed to certain triggers. Exercise is one of those triggers in susceptible people. The patient with EIA complains of chest tightness, wheezing, and shortness of breath when exercising. Some patients only experience coughing with exercise. Symptoms are usually worse in cold, dry air. This is believed to be due to the drying and cooling of the airways, which occurs with exercise, especially if the patient opens his or her mouth while exercising. Nasal breathing is much better at warming and humidifying air and may help to reduce EIA.
Dr. Cali feels that the most important point about EIA is to make sure a specific diagnosis is made. It is difficult at times to differentiate asthma from the normal breathlessness, which occurs with exercise. The feature of EIA that distinguishes it from normal breathing, or being "out of shape" is the fact that EIA is ALWAYS associated with a decrease in airflow. This can be measured with either a peak flow meter or a spirometer. It is also important that a specific diagnosis be made so that a person will not be labeled as asthmatic when they may be "normal" or have other conditions such as heart problems or anemia.
Dr. Cali also recommends before a person is labeled asthmatic, they have spirometric testing. An improvement in airflow after inhaling. A bronchodilator is an important indicator of asthma. Sometimes a bronchial challenge test is needed to diagnose asthma. In this test, the subject breathes in a known bronchoconstrictor in small quantities and the response is noted. Patients with asthma almost always respond to the inhaled agent by a reduction in airflow.
Inform Coaches – If coaches are made aware, than they can be prepared for the onset of EIA. Provide emergency contacts and medications with instructions, such as inhalers, should be available.
Warm and Moisten Air - Whatever the patient can do to warm and moisten the inhaled air can help prevent EIA. Nose breathing during exercise or wearing a loose covering over the mouth in cold weather may help. Sometimes, in severe cases, switching to an indoor sport like swimming may be necessary.
Start Out Slowly - It is important to start out slowly and warm up first before exercising at full tilt. Slowly jog around the track or field before practice or a game to prepare your lungs for full-speed.
Medications – are often necessary. Quick- acting bronchodilators like Albuterol, used 15-20 minutes before planned exercise, is recommended. This can be repeated once more during the exercise, but if tightness or wheezing occurs, the exercise should be stopped. Many patients with asthma require preventative treatment with anti-inflammatory medications. Inhaled steroids and/or leukotriene inhibitors may have to be added if the asthma is not controlled with Albuterol alone. In fact, some patients with asthma who are overly reliant on quick acting bronchodilator medications can get into serious trouble if they do not use inhaled steroids. Be sure to communicate your needs with your coaches.
Play Smart - In conclusion, people with asthma should not shy away from exercise. With proper precautions, people with asthma should be able to participate in all kinds of sports activities: baseball, football, soccer, swimming, tennis and running (even a marathon)! The key point is that the asthma needs to be under control and monitored by the patient, parents, coaches and doctor as a team.
Visit your doctor regularly and listen to your body.
Medical Contributor: Gregory Cali, DO, pulmonary specialist, Dunmore, PA

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Most would agree that this spring has a little cloudy, rainy and cool in NEPA. However, warm sunny days are soon to come. While protection from the sun is very important, too much time indoors playing computer games and watching television, can lead to potential problems from lack of exposure to the sun. One must use good judgment and have balance as the potential exists for Vitamin D deficiency due to lack of sun exposure. This problem may be true for individuals who use too much protection or spend most of their day indoors due to occupation or poor health. Therefore, it will be the purpose of this column to discuss the importance of Vitamin D for health and wellness.
Vitamin D, a fat soluble vitamin, is found in food and can be made by your body after exposure to ultraviolet (UV) rays from the sun. The liver and kidney help convert it to its active form. Therefore, vitamin D assists calcium absorption, which is essential for normal development and in forming and maintaining strong bones and teeth. Without it, bones can become thin, brittle and soft. The classic Vitamin D deficiency diseases are rickets in children and osteomalacia in adults. Rickets results in skeletal deformities. Osteomalacia is the softening of bones. Therefore, it is essential for normal bone health and may diminish or prevent the onset of osteoporosis in the elderly.
The requirement for Vitamin D is dependent on age, sex, degree of sun exposure and the amount of pigmentation in the skin. Since it can be produced by the body and retained for long periods of time by the body’s tissues, the precise daily requirement has been difficult to determine. Instead, an Adequate Intake (AI) level has been established. AI is a level of intake sufficient to maintain healthy blood levels of an active form of Vitamin D.
Vitamin D deficiency can occur when dietary intake is inadequate, when there is limited sunlight exposure, when the kidney cannot convert Vitamin D to its active form or when Vitamin D is inadequately absorbed from the gastrointestinal tract. Season, geographic location, time of day, cloud cover, air pollution, sunscreens, living indoors and living in cities where tall buildings block adequate sunlight from reaching the ground affect UV ray exposure. Therefore, individuals with limited sun exposure are at risk of this deficiency. Homebound individuals, people living in northern latitudes (e.g. New England, Alaska), individuals who cover their bodies for religious reasons and people whose occupations prevent exposure to sunlight may need to supplement in other forms.
Sunscreens with a sun protection factor of 8 or greater will block UV rays that produce Vitamin D. Older adults have a higher risk for this deficiency because the skin’s ability to convert Vitamin D to its active form decreases with age and the kidneys, which help convert Vitamin D to its active form, do not work as well when people age. Individuals with pancreatic enzyme deficiency, Chron’s disease, cystic fibrosis, sprue, liver disease, surgical removal of part or all of the stomach or small bowel disease may need extra intake because Vitamin D is a fat soluble and they have reduced ability to absorb dietary fat. Supplements are often recommended for exclusively breast-fed infants because human milk may not contain adequate Vitamin D. Consult with your pediatrician on this issue.
SOURCES: The National Institutes of Health; CDC

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
It is four months since many people have made their health and fitness resolutions and hopefully some have stayed the course. If you are looking for another reason to stick to your New Year’s Resolution to get fit and lose weight in 2024 try this…to improve or prevent hip and knee pain!
There are three major weight-bearing joints in the body, the hip, knee and ankle/foot. Consequently, wear and tear and arthritis are common among these joints. There are almost 800,000 knee replacements and 450,000 hip replacements annually in the United States alone. While there are many recommended methods to avoid or delay joint replacement, only a few are within our control. Genetics, trauma, degenerative diseases such as rheumatoid arthritis and osteoarthritis are difficult to control. However, body weight, aggressive weight bearing sports and overdoing exercises as you age like excessive running, jumping, lifting and squatting can be modified or eliminated to limit the progression of joint damage. According to WebMD, “your knees are powerhouses. They’re the biggest, strongest, joints in your body, and most people use them throughout the day to sit, stand, walk, jump, and bend. They bear 80% of your body weight when you stand still and 150% or more when you walk across the room. In a 160-pound person, that’s 240 pounds of force!”
According to the National Institutes of Health, body weight or body mass index (BMI) has a direct impact on hip and knee degeneration, pain and dysfunction. In fact, one study found that people with or at risk of significant hip/knee osteoarthritis had a 2-3% reduction in risk of hip or knee replacement for every 1% reduction in weight, regardless of the baseline BMI.
It is commonly known that the primary cause of osteoarthritis is normal wear and tear, especially for those over 50. However, extra body weight can accelerate this process. As the joint degenerates, the cartilage at the end and in between your joints gets compressed and dehydrated which leads to deterioration. Eventually, the bones rub directly on each other as the cushion wears away, leading to pain, swelling, and stiffness, loss of motion, strength and function.
While it may seem obvious that extra weight will put more strain and stress on the hip and knee joints; another mechanism involved in this degenerative process. Excess body fat can increase chemicals in your blood stream that can cause inflammation in your joints.
If you need a goal and a motive, how about this: losing even 10 pounds will equate to 40 pounds less force compressing and stressing your hips and knees. Moreover, reducing body fat will limit the hormones that cause inflammation in your joints. Talk to your primary care physician or visit www.cdc .gov to find a BMI calculator. Just plug in your height and weight and it calculates it for you. For example, a 155-pound male at 5 feet 8 inches tall has a BMI of 23.6. (A BMI of 18.5 to 24.9 is considered a healthy weight for this person).
The Mediterranean Diet is a solid start to eating healthy. It is less of a diet and more of a lifestyle. The foundation of this diet is plant foods built around vegetables, fruits, herbs, nuts, beans and whole grains. Moderate amounts of fish, dairy, poultry and eggs with limited consumption of red meat are paramount. The Mediterranean lifestyle also includes shared meals with family and friends, small portions, regular exercise, and wine in moderation with food and friends.
Exercise has many more benefits than just losing weight. Physical activity is one of the most important factors in improving a lifestyle in a positive way. A minimum of 30 minutes of physical activity, 5 days per week can greatly contribute to weight loss and longevity.
Researchers have found that the benefits of regular physical activity are numerous. Some of the more important benefits are:
Visit your doctor regularly and listen to your body.
Keep moving, eat healthy foods, exercise regularly, and live long and well
SOURCES: WebMD, National Institutes of Health; CDC, American Council on Exercise

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
In addition to lowering blood pressure, this gentle form of exercise can help maintain strength, balance, flexibility and mental health and is an ideal activity for all ages!
This research was brought to my attention by my friend and mentor from Dalton, Peter Frieder, Chairman,Gentex Corporation and current Board Chair at WVIA. Peter is celebrating his birthday today with a number of years that clearly does not represent his physiological age, in great part due to his dedication to health and wellness. Happy Birthday and thank you!
According to a new study by the China Academy of Chinese Medical Sciences (CACMS), the ancient martial art practice of Tai Chi is effective in lowering blood pressure as much, if not more, than traditional aerobic exercise. For those with prehypertension or hypertension and are unable to tolerate the repetitive and prolonged weight bearing stresses of running, walking or cycling, these results have tremendous implications. The slow, gentle and controlled movements and positions of Tai Chi coupled with controlled breathing and meditation may be a valuable alternative, especially for those with aging muscles and joints. Improved strength, flexibility balance, posture and mental health are additional bonuses.
Tai Chi is multifaceted in that it combines martial arts, slow gentle and controlled movements, sustained postures, a focused and meditative mind, and controlled breathing. It is considered by many to be “meditation or medication in motion.”
Tai Chi involves slow-motion movements transitioning with control from one position to another. The positions have historically been named for the actions of animals, for example:

Deep and purposeful breathing, mental focus, body awareness and meditation are integral components of the exercise. The beauty of Tai Chi is not only in the physical form, but also in its safety for all levels of fitness. It is helpful for individuals from high level athletes to those with physical disabilities. The movements are natural and gentle without forcing the muscles and joints to extreme or uncomfortable positions. It is often used as an adjunct therapy in the wellness as well as rehabilitation of a variety of athletic (ACL surgery, joint replacements) and neurological conditions (Parkinson’s, MS, head trauma), to name a few. Based on the aforementioned Chinese study, Tia Chi can be applied as a technique to control or lower blood pressure, especially for those who cannot utilize traditional aerobic exercise.
Tai Chi has been found to offer many physical and mental benefits. Some of these include:
Muscle Strength – upper and lower body, trunk and core strength
Flexibility – participants report improved range of motion and flexibility of the spine and extremities
Balance and Proprioception – some studies report a reduction of falls due to a variety of sustained positionsand improved awareness of one’s body in space
Aerobic Conditioning - recent studies have found that participants have lower heart rate and blood pressure
Mental Health – through improved balance, strength, and flexibility, studies show participants have gained confidence and control as well as lower blood pressure and stress reduction.
All Tai Chi classes begin with four basic principles: warm-up, instruction, practice and breathing.
Warm-up- gentle easy motions to warm-up and loosen the joints and muscles to prevent injury.
Tai Chi Forms – “Short Forms” are beginner movements which are gentle, slow, and short in duration while “Long Forms” are more advanced.
Breath Work – gentle breathing combined with movement to relax the mind and focus energy
Don’t be intimidated by the language or history – Yang, Wu, Cheng are only brands of movements with a history of martial arts but this in no way impacts participation.
Get medical clearance – check with your physician to see if Tai Chi is safe for you. Some orthopedic or vestibular problems might require special attention.
Observe or take a beginner class – often available at local fitness clubs or senior centers. Research options in your area and find a friend to join you. Consider an introductory instructional video to get a feel for Tai Chi. (See local Tia Chi classes below)
Meet with an instructor – if it makes you more comfortable, make time to talk to an instructor before enrolling in a class.
Dress for success – wear loose-fitting clothes that allow for range of motion and comfortable shoes for balance and support.
Track your progress – use an app or keep a journal of your progress. Heart rate, blood pressure and endurance (the time you can hold a pose or tolerate a class) are easy to monitor.
Model: Lily Smith, University of Scranton Physical Therapy Student and PT aide at Mackarey Physical Therapy.
Sources: HarvardHealthPublishing; New Atlas; China Academy of Chinese Medical Sciences (CACMS); National Institutes of Health
Local Tai Chi Classes: Steamtown Yoga, Scranton, PA; Mission Yoga, Scranton, PA;Dragon’s Heart Tai Chi & Kung Fu, Clarks Summit, PA; Rothrocks Kung Fu & Tai Chi, Duryea, PA
For more information: HarvardHealth; www.taichihealth.com; www.treeoflifetaichi.com

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Seasonal allergies affect 30 % of adults and 40% of children in the United States. Avoiding the outdoors is often not an option…especially if you enjoy outdoor activities and sports. Not long ago, it was unthinkable that an athlete with serious seasonal allergies could compete at a high level, such as the Olympics. Now, in great part due to advanced research, medications and proper management, an Olympic gold medal for those suffering from seasonal allergies is a reality. Recently, the National Institute of Allergy and Infectious Disease at the National Institutes of Health have published research on this topic to provide a better understanding and make recommendations.
The most common allergic reactions which athletes suffer from are sneezing, itchy and watery eyes, runny nose and coughing. Moreover, 67% of those with these symptoms also suffer from asthma. The athlete in NEPA is particularly vulnerable when the pollen count is high during spring and fall for several reasons. One, after being indoors all winter, one might develop a heightened sensitivity to allergens. Also, increased rapid and deep breathing during exercise makes athletes more susceptible to significant symptoms when exposed to allergens such as tree, grass and weed pollens.
Allergy skin testing can be performed to determine the allergens to which you are susceptible. Once determined, allergy shots are effective in building up tolerance to these allergens. If appropriate, you may be able to use allergy drops, administered under the tongue and conveniently used at home.
Asthma suffers should use their inhaler BEFORE symptoms occur. A recent study found that pretreatment using a short-acting bronchodilator inhaler within 15 minutes before exercise is very effective in preventing asthma symptoms for more than four hours. It is important to keep a bronchodilator available. If you fail to benefit from this, see your physician for other methods to control your exercise-induced symptoms.
Whether you have allergic respiratory problems from rhinitis or asthma, you many benefit from conditioning your airways with a 10 to 15 minute warm-up before and cool-down after the activity. This may serve to gradually prepare your lungs for an increased demand.
In addition to preventing dehydration on hot and humid days, constant hydration is very important for the athlete with allergies to prevent dry airways in athletes.
Know the signs and symptoms of asthma (coughing, wheezing, tightness in chest, shortness of breath).
Some schools have a file on each student athlete with a allergic or asthmatic problem which requires medication. The file includes information such as medical doctor release and instruction, emergency contacts and medications. Students must have their medications on hand before they can enter the field. The National Athletic Trainers Association recommends using a peak flow meter to monitor at risk players and can determine when a player can return to the field.
If possible, find an alternate practice facility with climate control for athletes at risk. Plan practices for these athletes when the pollen count is low. Check the newspaper or internet for pollen counts in your area. Training by the water, (ocean) where there is a breeze and less pollen is helpful.
Shower and change clothing immediately after being outdoors
During a flare up, do less aerobic exercise to limit stress on respiratory system. Try strength training indoors instead.
When pollen count is high, keep windows shut at home and in your car….use air-conditioning.
Keep pets out of your bedroom…especially when sleeping
Dry clothing in dryer…do not hang on clothesline outdoors
Sources: American College of Allergy, Asthma, and Immunology. National Athletic Trainers Association.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
A myth is a traditional story, idea, or belief, especially one concerning early history of a people or explaining a natural or social phenomenon. It is a widely held but false belief or idea. In medicine, health myths are also widely held beliefs about health issues such as medicines, herbs, treatments, cures, antidotes, etc. which are partially or totally false and unsubstantiated in the scientific literature. This is a partial list of the most common health myths:
SOURCES: WebMd; National Institutes of Health, Mayo Clinic

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article does not intend as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!