In 2000, President Bill Clinton dedicated March as National Colorectal Cancer Awareness Month. The purpose of this designation is to increase public awareness of the facts about colon cancer – a cancer that is preventable, treatable and has a high survival rate. Regular screening tests, expert medical care and a healthy lifestyle, which includes a proper diet and exercise, are essential for prevention. Several studies have demonstrated that exercise can also help prevent colon cancer.
The American Cancer Society estimates that there will be approximately 107,000 new cases of colorectal cancer in 2023. Of these, 52,550 men and women will succumb to the disease. It is the second-leading cause of U.S. cancer deaths for both men and women combined. The good news is incidence and mortality rates are dropping both nationally as well as in northeast Pennsylvania. The bad news is northeast Pennsylvania still has increased incidence and mortality rates when compared to the national average.
Studies show that prevention of this disease is multifaceted and includes: engaging in daily exercise, eating a low-fat diet with little red meat, avoiding smoking, drinking in moderation and having regular colonoscopy screenings.
Early detection is the key to survival. Death from colorectal cancer can be eliminated if caught at the earliest signs of disease. Colorectal cancer progresses very slowly, usually over years. It often begins as non-cancerous polyps in the lining of the colon. In some cases, these polyps can grow and become cancerous, often without any symptoms. Some symptoms that may develop are: blood in stool, changes in bowel movement, feeling bloated, unexplained weight loss, feeling tired easily, abdominal pain or cramps, and vomiting. Contact your physician if you have any of these symptoms.
The risk of colon cancer increases with age, as 90 percent of those diagnosed are older than age 50. A family history of colon cancer increases risk. Also, those with benign polyps, inflammatory bowel disease, ulcerative colitis or Crohn’s disease are at greater risk and should be screened more frequently.
The intestine works like a sewage plant, recycling the food and liquid needed by your body. However, it also stores waste prior to disposal. The longer the wastes remain idle in your colon or rectum, the more time toxins have to be absorbed from you waste into the surrounding tissues. One method in which exercise may help prevent colon cancer is to get your body moving, including your intestines. Exercise stimulates muscular contraction called peristalsis to promote movement of waste through your colon.
Exercise to prevent colon cancer does not have to be extreme. A simple increase in daily activity for 15 minutes, two times per day or 30 minutes, once per day is adequate to improve the movement of waste through your colon. This can be simply accomplished by walking, swimming, biking or playing golf, tennis or basketball. For those interested in a more traditional exercise regimen, perform aerobic exercise for 30-45 minutes four to five days per week, with additional sports and activities for the remainder of the time. For those in poor physical condition, begin slowly. Start walking for five to 10 minutes, two to three times per day. Then, add one to two minutes each week until you attain a 30-45 minute goal.
Medical Contributor: Christopher A. Peters, M.D
Dr. Christopher Peters is a partner of Radiation Medicine Associates of Scranton (RAMAS) and serves as medical director of Northeast Radiation Oncology Centers (NROC). He is an associate professor of clinical medicine at GCSOM. Sources: American Cancer Society/Northeast Regional Cancer Institute, and CA Cancer J Clin.

EVERY MONDAY - Read Dr. Paul J. Mackarey "Health & Exercise Forum!"
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's Articles, visit our Healthcare Forum!
PEOPLE WILL OFTEN ASK ME, “IS THERE SUCH A THING AS AN EXERCISE RUT?” THEY WANT TO KNOW WHY THEY DO NOT SEEM TO BE IMPROVING WITH THEIR EXERCISE PROGRAM…they exercise 3-4 times a week for 30 to 45 minutes and they feel frustrated and STUCK in a rut.
The purpose of this column will be to offer suggestions on how to improve or get more out of a “stale” exercise program. Last week’s column offered tips to improve a stale cardiovascular and strength program. This week we will discuss flexibility and functional training tips and include the components necessary for a healthy mind, body and spirit connection.
Flexibility training involves the careful stretching of the muscles, tendons and joints to improve the range of motion in order to safely perform daily activities and sports without injuring or tearing soft tissues. It is probably the most neglected part of the fitness program. However, while the amount of inherent flexibility varies for each person, a minimal range is necessary as it relates to daily activities and sports. For example, as you age it is important to have enough flexibility in your back, hips and knees to wash your feet, put shoes and socks on. Flexibility exercises should always be performed after a warm –up activity and done slowly and gently.
There are two types of flexibility exercises; dynamic and static. Dynamic stretching is performed with movement such as pushing the ankle up and down like a gas pedal. Passive stretching is performed using an outside force such as using a towel to pull the ankle up in order to stretch the calf. Dynamic should be performed before an activity (before running or playing tennis) and static performed after the activity is over in order to increase range of motion for future activities.
In conclusion, it is easy for fitness enthusiasts to get so focused on maintaining a routine that they allow their program to become stale and ineffective. It is essential to reassess and update your program to prevent stagnation.
Make sure the routine has all three fundamental components of a well-balanced exercise program; cardiovascular, strength and flexibility training. Moreover, to be truly healthy, one must work toward a “Healthy Mind, Body, and Spirit. Therefore, in addition to traditional exercise one must incorporate the following: nutrition; meditation, relaxation techniques, yoga, core fitness; functional/sports specific training; leisure sports and activities
In order to prevent an exercise program from getting stale, one must incorporate all aspects of wellness…a healthy mind, body and spirit!
While each component offers its own specific benefit, the combination of all three cooperatively provides unique value. Too often, fitness enthusiasts concentrate on the exercises they LIKE or are good at more than the ones they NEED.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine
For all of Dr. Mackarey's articles our Health Care Forum
People will often ask me, "Is there such a thing as an exercise rut?" They want to know why they do not seem, to be improving with their exercise program?... they exercise 3-4 times a week for 30 to 45 minutes and they feel frustrated and STUCK in a rut. While initially responding favorably to exercise, after 6 -9 months or more, they do not notice progress in weight loss, strength, tone, endurance or daily function.
Here are a few suggestions on how to improve or get more out of a “stale” exercise program.
Step one is to build an exercise program that is grounded in the basics. Next, Step two, which begins after the basics have been mastered, includes the components necessary for a healthy mind, body and spirit connection and translates into functional activities of daily living including work and leisure sports.
Make sure your routine has all three fundamental components of a well-balanced exercise program:
While each component offers its own specific benefit, the combination of all three cooperatively provides unique value. Too often, fitness enthusiasts concentrate on the exercises they LIKE or are good at more than the ones they NEED. A well-balanced program includes what you like and need!
In fact, recent studies show that those performing all three components surpassed those performing one or any combination of two of the training types when tested for efficient:
Cardiovascular exercise is any activity that raises your heart rate and respiratory rate. This type of exercise strengthens the heart muscle and the muscles that assist in breathing. When these muscles are stronger, they in turn work more efficiently to deliver oxygen to your muscles and other parts of the body. Ultimately, these oxygenated muscles can work harder and longer to burn fat during exercise and at rest.
*Most experts recommend at least 30 minutes of sustained cardio, 3-4 days per week. However, recent studies support the notion of performing 10-15 minutes, twice daily, 4 days per week. For those “stuck” in a fitness rut, to advance your program, cardio should be performed 5-6 days per week for 45-60 minutes.
Strength training is an activity that provides any type of resistance to muscle contraction to build strength in the muscle. The resistance can be without movement against an immovable object such as pushing against a wall (isometric) or with movement such as lifting up or lowering a weight down against gravity (isotonic/dynamic). There are two types of isotonic muscle contraction; concentric, which involves raising the weight against gravity as the muscle shortens and eccentric which involves lowering a weight against gravity as the muscle lengthens.
A standing biceps curl is an example that incorporates both concentric and eccentric contractions. A progressive strength training program includes all three types of muscle contraction. By using the classic bicep muscle curl these photos will demonstrate all three types of muscle contraction:


Sources: National Institutes of Health; American Council on Exercise
Model: Heather Holzman

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” Next Week: Read Stuck in an Exercise Rut…Part II of II!
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine
For all of Dr. Mackarey's articles visit: Mackarey's Health and Exercise Forum!
Tomorrow is Valentine’s Day! And, while you may wonder what that has to do with health and wellness, you might be surprised to learn that love can be good for your health! Studies show that it is in our DNA to seek out good relationships and that these solid relationships can lead to a happier, safer and healthier life. Conversely, infatuation and less committed, volatile relationships that are “on and off,” are very stressful and unhealthy. But those fortunate to participate in a stable and satisfying long-term relationship are the beneficiaries of many health benefits! Whether you have spouse, partner, or close friend, (love is love is love), feeling connected, respected, valued, and loved is critically important to your health and wellness!
The US Department of Human Services found that couples in a committed long-term relationship are less likely to require sick visits to their physician. And, when hospitalized, these “love birds,” have shorter hospital stays. One theory for this health benefit is that couples in good relationships watch after each other to ensure regular healthy visits for routine care and testing. Consequently, they are less likely to have unexpected serious illnesses.
Experts feel that social isolation is associated with unhealthy behavior and depression. Happy, loving and committed couples are far less likely to suffer from depression. Furthermore, these couples are less likely to engage in risky and unhealthy behaviors such as excessive drinking and drug abuse.
Researchers have found a strong relationship between marital status and blood pressure. Happily married couples have the lowest, while unhappily married couples have the highest. Happy singles scored somewhere in between. It is also interesting to note that non married committed couples and well-adjusted singles with strong support groups had lower blood pressure.
Studies show that long-term committed couples have far less anxiety than new romance. MRI brain scans found both groups showed high activation in areas of the brain related to romance, but only new couples had activation of the area of the brain associated with anxiety.
A CDC report on pain included a study of more than 127,000 adults and found that married people were less likely to complain of headaches and lower back pain. In fact, one study showed, when a happily married couple held hands, pain thresholds improved and, the happier the marriage, the greater the effect
Similar to the findings on pain, there is a strong link between happy and committed couples and stress management. The support and love from a strong and healthy relationship provides good coping methods to help overcome adversity…job loss, illness etc.
Solid loving relationships can boost your immune system. In fact, researchers at Carnegie Mellon University found that people who exhibit positive emotions are less likely to get sick after exposure to cold or flu viruses.
It may be that a wound from “Cupid’s Arrow” will heal faster when you are in a loving relationship. Researchers at Ohio State University Medical Center gave married couples superficial wounds and followed their healing time. The wounds healed nearly twice as fast in spouses who interacted warmly compared with those who behaved with hostility.
Strong research indicates that married people live longer. Researchers found that people who had never been married were 58% more likely to die than married people. Some reasons purported were mutual financial, emotional and physical support and assistance from children. One common denominator for a short life span is loneliness and those in a healthy relationship may live longer because they feel loved and connected.
A study in the Journal of Family Psychology showed that happiness depends more on the quality of family relationships than on the level of income. So, according to the research, when it comes to a long, happy and healthy life…love is more important than money!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM
For all of Dr. Mackarey's articles visit our "Health and Exercise Forum"
We are more than one month into the New Year and many people are still talking about their health and fitness goals. As you probably know, losing weight and getting fit are the most popular resolutions, however, for many who have not maintained an active lifestyle in years, it is challenging to know where to begin. Moreover, beginning without a good plan can lead to injury and leave you discouraged. For example, those overweight and de-conditioned should not start a walking program to aggressively. Walking at a fast pace and long distance without gradually weaning into it will most likely lead to problems.
There is probably nothing more natural to human beings than walking. Ever since Australopithecus, an early hominin (human ancestor) who evolved in Southern and Eastern Africa between 4 and 2 million years ago, that our ancestors took their first steps as committed bipeds. With free hands, humans advanced in hunting, gathering, making tools etc. while modern man uses walking as, not only a form of locomotion, but also as a form of exercise and fitness. It is natural, easy and free...no equipment or fitness club membership required!
“There’s no question that increasing exercise, even moderately, reduces the risks of many diseases, including coronary heart disease, breast and colon cancer, and Type 2 diabetes,” said Dr. Jennifer Joyce, MD, professor of family medicine at GCSOM. “Research has even shown that you could gain two hours of life for each hour that you exercise regularly.”
According to the American Heart Association, walking as little as 30 minutes a day can provide the following benefits:
Anything is better than nothing! However, for most healthy adults, the Department of Health and Human Services recommends at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous aerobic activity, or an equivalent combination of moderate and vigorous aerobic activity. The guidelines suggest that you spread out this exercise during the course of a week. Also aim to do strength training exercises of all major muscle groups at least two times a week.
As a general goal, aim for at least 30 minutes of physical activity a day. If you can't set aside that much time, try several short sessions of activity throughout the day (3 ten or 2 fifteen minute sessions). Even small amounts of physical activity are helpful, and accumulated activity throughout the day adds up to provide health benefit.
Remember it's OK to start slowly — especially if you haven't been exercising regularly. You might start with five minutes a day the first week, and then increase your time by five minutes each week until you reach at least 30 minutes.
For even more health benefits, aim for at least 60 minutes of physical activity most days of the week. Once you are ready for a challenge, add hills, increase speed and distance.
Keeping a record of how many steps you take, the distance you walk and how long it takes can help you see where you started from and serve as a source of inspiration. Record these numbers in a walking journal or log them in a spreadsheet or a physical activity app. Another option is to use an electronic device such as a smart watch, pedometer or fitness tracker to calculate steps and distance.
Make walking part of your daily routine. Pick a time that works best for you. Some prefer early morning, others lunchtime or after work. Enter it in your smart phone with a reminder and get to it!
Studies show that compliance with an exercise program is significantly improved when an exercise buddy is part of the equation. It is hard to let someone down or break plans when you commit to someone. Keep in mind that your exercise buddy can also include your dog!
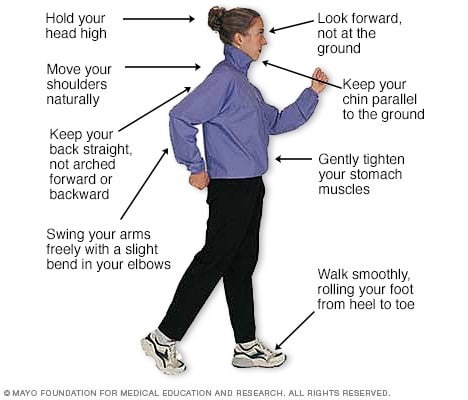
Like everything, there is a right way of doing something, even walking. For efficiency and safety, walking with proper stride is important. A fitness stride requires good posture and purposeful movements. Ideally, here's how you'll look when you're walking:
Sources : Sapiens.org; WebMD; Mayo Clinic
* Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine.
For all of Dr. Mackarey's articles: Visit our Healthcare Forum!
There is a very good chance that the cold temps and snow will return soon! Winter in NEPA can be the perfect opportunity to try something new. For example, for those who enjoy running or walking you can continue to do so in the winter, with a few adjustments. Equipment, such as treaded sneakers, allows you to run or walk in the snow. Snow shoes are a great way to hike and walk in the snow while cross country skiing simulates running in the snow. But, in the last few years, another outdoor activity has become a winter sport; mountain biking in the snow has become popular.
Many mountain biking enthusiasts in NEPA enjoy 7-8 months of trail riding at our beautiful state parks. Now, with a few modifications, mountain bikers can continue year round. In fact, the adventure in the snow may be an exciting new experience. If winter biking is not your thing, maybe winter walking, running, snow shoeing or cross-country skiing will suit you better.
The physical and psychological benefits of outdoor activities are many: each season brings its own unique beauty, and winter is no different. Most will not have to abandon outdoor activities, but some adjustments in equipment, clothing, and food are necessary for each season and the temperature changes that it brings.
While recommended, it is not necessary to purchase a bike specifically for mountain biking in the snow. With a few simple modifications and adjustments, you can prepare a regular mountain bike for winter use.
In addition to rocks and stumps, winter biking offers the challenges of snow banks and ice chunks. The air pressure in your shock system will be affected by temperature. Additional air pressure will be required to improve shock absorption and in extreme cases, using less viscous oil will be required.
Pressure - lower the air pressure in the tires 5-10 psi lower than normally used in the summer to improve traction.
Treads – Just as with winter car tires, a larger tire with more volume and large, widely space knobs will improve traction. Some special winter tires offer studs for improved performance on the ice.
Disc Brakes – that are self-cleaning and mounted away from the snow are best for winter biking. However, brakes should be examined and cleaned intermittently for snow and ice accumulation.
Platform Pedals – allow the rider to quickly plant the foot for balance when sliding.
It is important to layer clothing. Use DryTech or UnderArmor type materials (headgear, gloves, shirts and pants) to allow sweat to breath away from the skin to the next layer of clothing. Use a facemask to cover your mouth and nose to prevent frost bite and warm air before it enters the lungs. Chemical hand and toe warmers are great. Try winter running or walking shoes as described below.
There are running shoes specifically designed for use in wet, cold and sloppy winter conditions. These “winterized” running shoes, which can also be used for walking, offer waterproofing, sealed seams, gaiter collars to keep out snow and slop, slip resistant fabric, anti-roll stability features, anti-microbal material and aggressive tread patterns for traction on slippery surfaces. Some shoe recommendations for both winter walkers and runners include:
. Some shoe recommendations for winter runners and walkers from The Runner’s World Magazine include:
For winter walkers, walking or trekking poles will improve balance and safety when briskly walking in winter conditions. I am a strong proponent of using these tools. They are lightweight, adjustable, and collapsible. Some examples are: Black DiamondR Trail Explorer 3 Trekking Poles - $59.99 andMountainsmithR FX Lite Trekking Poles - $35.09. For an inexpensive alternative, an old pair of ski poles will work just fine.
These activities should also be considered as a viable option for the winter walker and runner. These are great cross-training alternatives with tremendous aerobic benefits.
Snowshoes work by distributing your weight over a larger surface area so your foot does not sink completely into the snow. Commonly used by fur traders, trappers and forest rangers, snow shoeing has become very popular among many outdoor exercise enthusiasts. It is relatively safe and inexpensive. Some snowshoes include the Tubbs Flex TRK - $169. (REI) and Redfeather Hike - $149.00 (Cabelas).Boots and poles are also required, but ski or trekking poles along with hiking boots or winter running shoes can be used.
Cross country skiing has also gained tremendous popularity among winter outdoor exercise enthusiasts. It is a cross between running and skiing in which the participant propels through a snow-covered trail by pushing and gliding with a running or fast-walking motion. Some examples of equipment packages that include boots, pole, bindings and skis are Alpina Sports Tour – no wax for $229.00 and Rossignol XT from LL Bean at $224.00.
Many of the area’s state parks, such as Lackawanna and Promised Land, offer wonderful trails for winter walking, hiking, running, snow shoeing, cross-country skiing and biking.
For the more casual walker in need of protection from the snow and ice, it may be treacherous just to walk the dog or go to the bank, post-office or grocery store. Consider traction devices that easily slip on and off your shoes or boots such as StabilicersR (cleats-type device) or YaktraxR (chain-type device).
Visit your doctor regularly and listen to your body.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum” every Monday.
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles: visit our healthcare forum
New Year’s Resolutions are very predictable. While most are health oriented, I purport that a healthy mind, body and spirit requires a healthy lifestyle. Interestingly, the ten most popular resolutions listed below, all have an impact on a healthy life.
Polls repeatedly show that one of the most consistent resolutions for the New Year is to make more time to spend with family and friends. Moreover, research shows that the comfort and camaraderie of these people whom we love is important to our health and well-being.
The benefits of regular exercise is no longer anecdotal, it is factual. Daily exercise, even in small doses, has been associated with more health benefits than anything else known to man. Studies clearly demonstrate that it reduces cholesterol and coronary artery disease and the risk of some cancers. Also, it increases longevity, helps achieve and maintain weight loss, enhances mood, lowers blood pressure, and even improves arthritis. In short, exercise keeps you healthy and makes you look and feel better. If done properly, there is no down side. So, make this year the year to do it!
Recent studies report that more than 66 percent of adult Americans are considered overweight or obese. As a result, weight loss is one of the most popular New Year's resolutions. However, adhering to a weight loss program is not easy. It requires many things, including, setting reasonable goals and staying focused. Often, professional help is required. While this may be one of the most difficult goals to attain, the ultimate reward and value is well worth the effort.
Second only to losing weight, this resolution, while extremely difficult, is another life-saving goal that must be attempted. Studies report that smokers try and fail four times on average before they are successful. SO, KEEP TRYING! Get help. Talk to your physician about using over-the-counter or prescription nicotine replacement therapy and proven quit-smoking aids. Consider smoking cessation classes, support groups and hotlines in addition to the meds. This is one goal that is worth the effort.
Due in great part to our hectic and stressful work and family demands, the United States is home to millions of people requiring the use of mood elevators and antidepressants. As a result, it is important to learn what really makes you happy in order to FIND YOUR SMILE. It requires the balance of a healthy mind, body and spirit. It might be a walk in the snow, taking dance classes or a trip to the spa. One hint, it is often something simple and inexpensive.
This is one tip for a healthier New Year that I expect to receive plenty of flack about! But, I would be remise if I did not mention this potentially harmful habit. While many people use the New Year as an incentive to finally stop drinking, most are unable to adhere to such a rigid goal. Studies show that moderate drinking can offer many health benefits such as lowering cholesterol and coronary artery disease but that is defined as one or two 8 ounce drinks per day and red wine is preferred. However, many heavy drinkers would do well to taper off to a moderate level. For those with a problem and have decided that you want to stop drinking, there is a world of help and support available such as Alcoholics Anonymous. There are also a number of treatment-based programs, as well as support groups for families of alcoholics.
This is one tip that few consider being health related. However, serious stress from financial problems affects millions of Americans every day. This cumulative stress can be very harmful to your health and can be lessened by initiating a plan. Get professional help and learn how to downsize and reevaluate your real needs…less toys with less stress for a longer life!
There may be no one thing more important to gaining a new perspective on life that to have learned something new. It could be as drastic as returning to school to prepare for a career change or as simple as learning to play bridge. Have you vowed to make this year the year to learn something new? Take a course at local college or read a new book. Visit the Everhart Museum or take the free tour of the Scranton Cultural Center. It will enrich your life and make you a more interesting person. Most local colleges and universities offer distance and adult education programs.
Service to others is service to you! There may not be anything more gratifying than providing a service to others in need. Volunteerism makes you a better and healthier person. It fits into any schedule. Donate clothes, time or resources. Locally, we have many charitable causes in need of help: Be a “Friend of the Poor,” or serve lunch at St. Frances Soup Kitchen.
The goal of organization, like the goal of financial order, has similar health implications because it eliminates tremendous stress. There are many books and websites that offer suggestions on how to organize just about anything in your life. For this reason, I love my iPhone – there’s an App for that!

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit:
The American Academy of Pediatrics (AAP) cited studies suggesting that heavy use of electronic media may interfere with children’s speech and language development replace important playtime with parents and lead to obesity. Studies also have found that more than 90 percent of U.S. kids have used mobile devices and most started using them before age 1. The pediatricians’ group recommends no screen time for children up to age 2. Moreover, they recommend total screen time, including TV and computer; use should be less than one hour daily for ages 2 and older. Pediatricians don’t want parents to overreact. They understand that a little screen time on occasion is not likely to harm a child, especially if they are typically active and creative most of the day.
Dramatic increases in virtual education makes this information more alarming. This may be the year to consider safe and appropriate gifts that promote physical activity. The academy’s website offers suggestions on ideal toys for young children, including balls, puzzles, coloring books and card games. Visit: AAP.org or HealthyChildren.org, the official parenting website of the AAP.
Giving gifts to children is a favorite part of the holidays, whether they're wrapped under a tree or exchanged with the lighting of a candle. When choosing a toy for a child, the American Academy of Pediatrics recommends the toy be appropriate for the child's age and stage of development. This makes it more likely the toy will engage the child – and reduces the risk it could cause injury. Below are some additional tips from the AAP on toy selection and safety:

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit: www.mackareyphysicaltherapy.com/forum
We all know someone who has been affected by a stroke. It can be a devastating and life-changing event. According to the National Stroke Association, (NSA) it is the 5th leading cause of death and number one cause of disability in the United States. Nearly 800,000 people in the USA have a stroke every year. Every 40 seconds someone has a stroke and every 4 minutes someone dies of a stroke in the USA. 897% of all strokes are ischemic from a clot or mass blocking a blood vessel in the brain.
According to a study in the Journal of the American Medical Association, there is almost a 50% reduction in strokes and 40% reduction in stroke deaths more than two decades from 1987 to 2011. THE GOOD NEWS: According to a study in the Journal of the American Medical Association, there is almost a 50% reduction in strokes and 40% reduction in stroke deaths more than two decades from 1987 to 2011. Improved smoking cessation, management of high blood pressure and cholesterol are believed to be significant contributing factors. THE BAD NEWS: Progress has slowed in recent years! THE MESSAGE: Continued vigilance and lifestyle changes are essential!
While the signs and symptoms vary, most people experiencing a stroke have several if not all of these symptoms in various parts of the body.
F – Face Drooping – ask for a smile to see if one side droops
A – Arm weakness or numbness
S – Speech – can the person repeat a simple sentence? Do they slur?
T – Time = Brain Damage! Time to Call 911
If the above signs or symptoms have been identified than there is a medical emergency - Immediately Call 911
Strokes can happen at any age, even to babies in the womb. Still, the odds of a stroke climb quickly after middle age.
Visit your doctor regularly and listen to your body.
Keep moving, eat healthy foods, and exercise regularly

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice in downtown Scranton, PA and is an associate professor of clinical medicine at GCSOM.
We all know someone who has been affected by a stroke. It can be a devastating and life-changing event. According to the National Stroke Association, (NSA) it is the 5th leading cause of death and number one cause of disability in the United States. Nearly 800,000 people in the USA have a stroke every year. Every 40 seconds someone has a stroke and every 4 minutes someone dies of a stroke in the USA. 897% of all strokes are ischemic from a clot or mass blocking a blood vessel in the brain.
According to a study in the Journal of the American Medical Association, there is almost a 50% reduction in strokes and 40% reduction in stroke deaths more than two decades from 1987 to 2011. THE GOOD NEWS: According to a study in the Journal of the American Medical Association, there is almost a 50% reduction in strokes and 40% reduction in stroke deaths more than two decades from 1987 to 2011. Improved smoking cessation, management of high blood pressure and cholesterol are believed to be significant contributing factors. THE BAD NEWS: Progress has slowed in recent years! THE MESSAGE: Continued vigilance and lifestyle changes are essential!
A stroke occurs when the arteries of the brain are unable to bring necessary blood flow to a specific region of the brain. When blood flow carrying essential oxygen and nutrients is unable to reach brain tissue, the brain cells in that tissue die. The longer the blood flow is cut off, the greater and more permanent the residual damage. Two primary causes of loss of blood flow to the brain are ischemic stroke and hemorrhagic stroke. In an ischemic stroke a clot obstructs or blocks the flow of blood to the brain. In a hemorrhagic stroke, a blood vessel tears or ruptures which interrupts the flow of blood to the brain. Another term used when describing a stroke is a “mini stroke” which is a transient ischemic attack (TIA) which caused by a temporary clot.
The effects of a stroke depend on several factors such as the location and duration of the tissue damage. The brain is unique in that one side of the brain is responsible for the opposite side of the body. So, a stroke that damages the right side of the brain will result in damage to the left side of the body.
The brain stem is the central trunk of the brain which traverses downward to form the spinal cord. Symptoms include:
Keep moving, eat healthy foods, and exercise regularly

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice in downtown Scranton, PA and is an associate professor of clinical medicine at GCSOM.
SOURCES: National Stroke Association, National Institutes of Health; www.strokeassociation.org; www.stroke.org