Like many of you, I have always enjoyed the outdoors...walking, running, biking, hiking etc. However, recently, I have been more concerned about being safe, (getting older and more cautious, distracted drivers) when doing these activities on the side of the road.
Almost 15 percent of all motor vehicle injuries to people happened to those not in cars but while walking, running or hiking, so one needs to be safe. In fact, over 4,000 walkers or runners were fatally hit by a motor vehicle according to the Centers for Disease Control (CDC). These statistics continue to increase as the number of distractions to drivers increases (phone calls, texts, etc). Consequently, walkers, runners and cyclists must be more aware than ever to prevent injury from motor vehicles and stay safe.
Source: http://www.runnersworld.com
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Have you ever noticed high level athletes warming up before a game or competition walking or running backwards? You may also see fitness enthusiasts in gyms emulating these athletes to improve their fitness or performance. I found the concept of backward walking, (also called retro walking) interesting and decided to research the topic for more information and validation. Walking backward does have many therapeutic benefits, however, before you attempt this activity on a treadmill or elliptical, please consult your physician and physical therapist and have a spotter nearby.
At a recent meeting of The American College of Sports Medicine, several studies were presented on the topic of backward waking. Most of the research was conducted while moving backward on a treadmill and an elliptical machine. When comparing two groups recovering from knee injuries, the backward motion group showed significant improvement in strength in the quadriceps (front thigh) and hamstring (back thigh) muscles when compared to the traditional forward walking group. Furthermore, the muscles of the front (tibialis anterior) and back (gastro/achilles) of the shin/ankle also demonstrated an increase in strength and endurance with backward walking. One explanation is that forward motion is routine in daily living that it has become very efficient and does not tax or stress the muscles the body. While this efficiency prevents fatigue in daily activities, it may not stress the muscles enough to gain strength as quickly as an unfamiliar exercise.
Due in great part to the increased strain of performing an unfamiliar exercise, backward walking on a treadmill or backward pedaling on an elliptical, offered a greater cardiovascular benefit and caloric expenditure than forward motion at all levels. Specifically, walking backward on a treadmill at 2.5 mph at grades of 5% - 10% has been found to significantly increase cardiovascular endurance than walking forward under the same conditions. This knowledge is useful for healthy individuals in need of greater cardio exercise. However, it may also serve as a precaution for those with cardio problems and should consult their physician prior to engaging in this activity.
A recent study in the International Journal of Obesity, found that those who performed new activities or increased the intensity of an activity, even if for a short duration (interval training) expended more energy and burned more calories than those who worked out at the same pace consistently for a longer duration. Moreover, when engaging in a new activity such as backward walking, even more calories were burned. This phenomenon may be due to the fact that routine activities such as forward walking are performed more efficiently and easily.
We challenge our body when we inefficiently perform a new motor skill such as backward walking and burn more calories. In other words, if you want to burn more calories without exercising for longer periods of time, than try a new activity and engage in higher intensity, intermittently, for part of the time. For example, walk backward on the treadmill for 30 minutes at 2.5 mph, but do so at a 5 – 10% incline for 1-2 minutes every 5 minutes.
Some studies show that using other muscle groups by performing different exercises not only prevents boredom, but also protects your muscles and tendons from overuse and joints from wear and tear. Specifically, the knee joint and the patella joint (the joint where the knee cap glides on the knee), benefits from backward walking due to less stress and compression forces on the joint. The thigh and ankle/foot muscles benefit from using a different form of contraction while lengthening the muscle. Some authors propose that this may also prevent strains and pulls and may be valuable to strengthen those with a history of shin splints and flat feet (pronation).
Mixing up your program prevents boredom. As a rule, those willing to change their exercise routine are more compliant and continue to exercise longer than those stuck in the same routine. A new challenge to improve distance, speed, and resistance while exercising in a different direction will be refreshing to your program.
Prevention of falls by improvement in balance and coordination has received a great deal of attention in the past few years. This is not only valuable to the athlete but may be even more important to those over 50. With age, balance centers are slow to react to changes in inclination, elevation, rotation and lateral movements. This slow reaction time leads to falls that may cause fractures, head injuries and more. Working on this problem by challenging the vestibular and balance centers before it is seriously compromised is important and backward walking is one way for this to be effectively accomplished.

Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

As summer fads and cool fall nights are upon us, many of us will prepare to put away some of our warm weather toys…closing the pool, storing kayaks and boats and packing up the “slip and slide.” However, one activity that can last well into the fresh breeze of fall is cycling. In fact, many feel that fall is the best time of year to jump on a bike and enjoy the ride! If you are looking for a kick start to riding your bike this fall, consider the 20th and final Tour de Scranton on Sunday, April 15, 2024. It is a fun-filled, noncompetitive bike ride through Scranton and neighboring communities. Tom and Betty Moreken, with the help of dedicated friends and countless supporters have raised over $400,000.00 to benefit addiction treatment and prevention in honor of their daughter Erin, a victim of drug addiction. I have had the privilege to know Tom and Betty and have always admired their resilience and selflessness to turn a negative into a positive and do something good for others. They and their friends truly represent everything that is good about the people of NEPA!
So dust off your bikes and join the fun at Tour de Scranton. Hopefully, it will entice you to ride the many beautiful and well-maintained trails that are available at the Countryside Conservancy and other locations in the Abingtons and the Lackawanna Heritage Valley Authority.
Tour de Scranton is the official “kick off” to biking season in NEPA. This year, on Sunday, September 15th, the 20th annual and final Tour de Scranton will offer a selection of several routes and distances for the novice and experienced rider at its non-competitive bike ride for riders of every age and skill level. This event supports “The Erin Jessica Moreken Drug & Alcohol Treatment Fund” which provides charitable gifts to qualified local organizations or individuals struggling with the disease of addiction. For more information visit: www.tourdescranton.com.
There are many obvious reasons to bike…cardiovascular fitness, burn calories, improve leg strength and others. But, the real question is, “what are the advantages of biking over other forms of exercise?” Glad you asked…
Prevention is the best management of musculoskeletal problems associated with biking. First, many of the problems associated with biking such as knee pain, buttock soreness, and tendonitis can be prevented through proper fitting. Furthermore, it is important that your equipment be in good working order such as tires, chain, brakes and pedals. Next, be sure to maintain a fairly good fitness level in order to bike safely. If you are a beginner, start slowly. Warm up and slowly bike for 10 to 15 minutes and build up over time. Practice the coordination of stopping, starting, shifting and braking. Work on good strength and flexibility of the hamstrings, quadriceps, calves and gluteal muscles. All of these muscles are necessary to generate pedal force. Balance is also important to safety and can be practiced on and off the bike. Be aware that adaptive equipment can modify your bike for added comfort and safety such as soft handlebar tape, seat post and front fork shock absorbers, padded biking shorts, c-out and gel pad saddle seats, and wider tires.
Be careful not to progress too quickly because inactivity to over activity in a short period of time can create problems. Overuse injuries such as tendonitis, can be avoided by cross training. Bike every other day and walk, run or swim on off days. Make sure to take time off to recover after a long ride. Use ice and massage to sore muscles and joints after riding.
Remember, cycling should be fun! Pain from improperly fitted and poorly maintained equipment is preventable. Excessive workouts and training rides should be kept to a minimum and consider cross-training in between.
EQUIPMENT: Helmets are a must! Also, keep your bike in good condition. Road bikes should have mirrors and reflectors. Use hand signals and obey traffic rules. Dress for weather and visibility. Have a first aid and tire patch kit, tire pump and tools. Seat comfort can be improved with gel cushion or split seat.
BE ALERT: for traffic, parked cars, pedestrians loose gravel and cracks in the road.
SOURCES: American Physical Therapy Association
Visit your doctor regularly and listen to your body.
Keep moving, eat healthy foods, and exercise regularly

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Patients often tell me that they would like to exercise but hesitate due to their knee or hip pain. They want to know what type of exercise is best for those suffering from osteoarthritis (OA). Osteoarthritis is also known as degenerative arthritis. It is the most common form of arthritis in the knee. It is usually a gradual, slow and progressive process of “wear and tear” to the cartilage in the joint which eventually wears down to the bony joint surface. It is most often found in middle-aged and older people and in weight bearing joints such as the hip, knee and ankle. It causes gradual onset of pain, swelling and stiffness in the involved joint, especially after increased activity and weakness with loss of function due to disuse.
However, OA is not an excuse to avoid exercise but it is important to be smart about it. Regular exercise is essential to maintain a normal lifestyle for those with OA. However, if you do the wrong exercise, use poor technique, or are too aggressive, you could flare-up your joints and do more harm than good.
When performed correctly, exercise for those with OA has many benefits:
Pain Control
Exercise controls OA pain by releasing natural pain control chemicals in the body called endorphins. It also controls pain by assisting in weight loss and improving range of motion.
Weight Control
We all know how well exercise burns calories and that increased body weight creates increase stress on the joints.
Prevention of Joint Stiffness
Exercise will help maintain joint range of motion. A stiff joint is a painful joint.
Prevention of Muscle Weakness
Exercise will help maintain muscle strength. Weak muscles will allow or increase in joint wear and tear.
Maintain Lifestyle
If a joint is stiff and weak, then they become painful which negatively impacts your lifestyle. Exercise can prevent this problem.
Start Slowly
Wean into exercise because if you advance too quickly, you will flare up the joint and have increased pain. For example, walk for 5-10 minutes the first session. If you do not have pain, add 1-2 minutes each session.
Lose Weight
Every pound lost equates to less stress on your joints. For example, a loss of 5 pounds of body weight translates to 20-30 pounds of stress through the knee, according to David Borenstein, MD, President of the American College of Rheumatology. Also, body weight has a direct impact on daily activities. For example, walking upstairs creates stress through the knee equal to 4 times body weight and seven times body weight going downstairs. Therefore, less body weight equals less stress.
Low Impact Workouts
Low impact exercise creates less stress on the joints while strengthening leg muscles and those who those who maintain leg muscle strength have less stress on their joints. It is even important not to load your arms with heavy objects when walking or using stairs to limit joint stress.
Some examples of low-impact exercises are: walking, swimming, elliptical trainer, and biking. Strength training is also low-impact and should be performed with low weight and high repetitions. Water therapy is great for those with OA, especially in a heated pool. It is a great low-impact exercise with less gravity and stress on the joints. Walk, swim and do mild resistance exercises in the water. Use a snorkel and mask for swimming to limit excessive neck turning and back extension.
Walking is a great form of exercise; however, walking softly is important for those with OA. Wear good running shoes and orthotics if necessary. Discuss this with your physical therapist or podiatrist. When possible, use soft surfaces like cinder, mulch or rubber. Avoid grass and soft stand due to instability and torsion that may irritate your joints.
Warm-Up
Warming up your body is critical to prevent injury to the muscles and tendons. This can be done by marching in place or using aerobic equipment such as a bike for 5 to 10 minutes before exercise. Always perform the warm-up activity at ½ your normal pace.
Balance & Relaxation Techniques
Tai Chi and ballroom dancing are two good examples of activities which promote balance and relaxation. Studies showed that those with OA who participated in Tia Chi two times a week for eight weeks reported less pain, increased range of motion and improved daily activities and function. They also noted less low back pain and better sleeping.
Proper Clothing
Stay warm in winter and consider wearing compression shorts. Be cool in the summer months with DrytechR type material.
Pre/Post Exercise First Aid
If you are sore for longer than 12 to 24 hours after exercise, then you overdid it and must make adjustments next time. Otherwise, use hot packs, bath or shower before you exercise to loosen up and apply ice to your joints after exercise, especially if they are sore.
Post Exercise Stretch
Gentle, active range of motion stretches after exercise is important to maintain mobility. Do not bounce or cause pain. For example: Low Back – knees to chest; Arms – row –the – boat, arms behind head, arms behind back; Legs – wall lean calf stretch, bend and extend knees, open and close hips.
SOURCES: Rothman Institute, Philadelphia, PA and American Academy of Orthopaedic Surgeons; www.lifescript.com
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
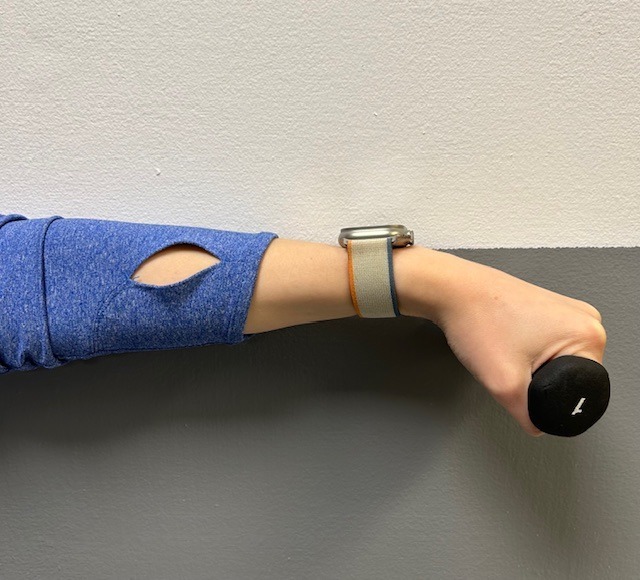
Tennis elbow, also called lateral epicondylitis, is an inflammation of the lateral (outside) bony protuberance at the elbow. It is at this protuberance that the tendon of the long muscles of the hand, wrist and forearm attach to the bone. As the muscles repeatedly and forcefully contract, they pull on the bone, causing inflammation. The trauma is irritating when working the muscles in an awkward position with poor leverage like hitting a backhand in tennis.
It is not unusual for a patient to come to my office with severe pain on the outside of their elbow. Especially, after intensifying their tennis workouts or changing the racquet string tension. Others come to me with pain on the inside of the elbow (“golfer’s elbow”) from wrist action that advanced golfer’s use at impact. However, this problem is not only for tennis players and golfers. Laborers working with wrenches or screwdrivers with an awkward or extended arm can also develop tennis elbow. Others who are vulnerable are: those working for hours at a computer using a mouse as well as those working hard maintaining their lawns and gardens.
In a more chronic problem, lateral elbow pain may arise by a degenerative condition of the tendon fibers on the bony prominence at the lateral elbow. Sporadic scar tissue forms from a poor attempt by the body to overcompensate and heal without eliminating the cause.
While symptoms may vary, pain on the outside of the elbow is almost universal. Patients also report severe burning pain that begins slowly and worsens over time when lifting, gripping or using fingers repetitively. In more severe cases, pain can radiate down the forearm.
Conservative treatment is almost always the first option and is successful in 85-90 percent of patients with tennis elbow. Your physician may prescribe anti-inflammatory medication (over the counter or prescribed). Physical/Occupational therapy, rest, ice, and a tennis elbow brace to protect and rest may be advised. Ergonomic changes in equipment, tools, technique and work-station may be necessary. Improvement should occur in 4-6 weeks. If not, a corticosteroid injection may be needed to apply the medication directly to the inflamed area. Physical therapy, range of motion, and stretching exercises may be necessary prior to a gradual return to activity. Deep friction massage can assist healing.

Exercises performed in a particular manner to isometrically hold and eccentrically lengthen the muscle with contraction.
New Conservative Treatment: Platelet-Rich-Plasma (PRP) is a new treatment for the conservative management of degenerated soft tissues that has recently received great media attention. In great part, due to its success in several high profile athletes. According to the Journal of the American Academy of Orthopaedic Surgeons,(JAAOS), platelet-rich plasma (PRP) is autologous (self-donated) blood with an above normal concentration of platelets. Normal blood contains both red and white blood cells, platelets and plasma. Platelets promote the production and revitalization of connective tissue by way of various growth factors on both a chemical and cellular level.
The actual PRP injection requires the patient to donate a small amount of their own blood. The blood is placed into a centrifuge (a machine that spins the blood at a high velocity to separate the different components of blood such as plasma, white and red blood cells), for approximately 15 minutes. Once separated, the physician draws the platelet-rich plasma to be injected directly into the damaged tissue. In theory, the high concentration of platelets, with its inherent ability to stimulate growth and regeneration of connective tissue, will promote and expedite healing.
Surgery for tennis elbow is only considered in patients with severe pain for longer than 6 months without improvement from conservative treatment. One surgical technique involves removing the degenerated portion of the tendon and reattaching the healthy tendon to bone. Recently, arthroscopic surgery developed to perform this technique. However, research does not support the value of one over the other at this point. Physical/occupational therapy is used after surgery. Return to work or athletics may require 4-6 months. More recently, a surgical technique using ultrasound to guide a needle to debride (clean) the area of scar tissue has been developed. If eligible for this procedure, the time required for healing, rehabilitation and return to activity is much shorter.
If you feel you suffer from tennis elbow, ask your family physician which of these treatment options are best for you.
Visit your doctor regularly and listen to your body.
EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy

This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
There is still plenty of summer remaining and its not too late to think of your pleasure puddle in different light…a health spa! It may very well be the exercise of choice for many people. Many have discovered the benefits of moving their limbs in the warm water of a home pool following knee or shoulder surgery. Also, long distance runners who often look for cross training methods without joint compression and arthritis sufferers who are often limited in exercise choices by joint pain from compressive forces when bearing weight, can enjoy the buoyancy effects of water. These are good examples of the benefits or water exercise…aerobic and resistive exercise without joint compression.
Most doctors recommend some form of exercise with arthritis. Pain and fatigue are the most limiting factors for the person with arthritis. Pool exercise may be the answer. With proper technique, adequate rest periods, appropriate resistance and repetitions, water exercise can be very effective.
The following are some of the benefits of water exercise:
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
JUNE IS GREAT OUTDOORS MONTH! AS WE KICK OFF SUMMER AND CELEBRATE THE FOUR OF JULY, MAKE TIME TO GET THE HECK OUTSIDE! Research shows that spending time outdoors has many positive effects on your health. While there are many year-round activity options, in Northeastern Pennsylvania our short-lived summer is the inspiration to “suck the marrow out of a sunny day!” Summer in NEPA is enjoyed in many ways such as walking, running, hiking, biking, horseback riding, boating, kayaking, and swimming. Studies show that even less vigorous activities such as fishing, picnicking camping, barbequing, or reading a good book on the porch are healthier than being indoors.
It is reported that Americans spend 90% of their lives indoors and that number increases with age. Worse yet, for some, venturing outdoors is considered risky behavior with fear of the sun, ticks, wind, mosquitoes, and other creatures of God. Well, the truth of the matter is the risk of being one with nature is far less than the ill effects of a life stuck indoors. Please consider the following benefits of spending time outdoors.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
June is migraine and headache awareness month! According to the World Health Organization about half of the world’s adult population has had a headache at least once in the past year. Prolonged use of electronic devices has greatly contributed to this problem. For many people, these headaches are infrequent and do not often affect daily life. But what about when your headache occurs frequently or is so severe it prevents you from going about your day to day activities? Some types of headaches are more easily treated and managed than others.
There are two types of headaches: primary and secondary. Primary headaches occur without an underlying disease and include migraines and tension-type headaches. Secondary headaches can be associated with serious disease, requiring emergency care, or can be referred from other structures of the body such as the cervical spine (neck).
Headaches symptoms that may constitute a medical emergency are: vomiting, seizures, fever, muscle pain, night sweat, weight loss, and neurologic symptoms such as blurred vision. If you are experiencing any of these symptoms, if your headache worsens, or your symptoms change it is recommended that you seek medical attention. Any headache that is unusual for you and does not resolve itself in a reasonable time should be brought to your primary care physician’s attention.
Migraines: Migraines are a primary form of headache that typically lasts from four to seventy two hours, can range from moderate to severe pain, and typically are located on only one side of the head. Often they can be accompanied by an aura, nausea or vomiting, sensitivity to sound, or light sensitivity. Migraines can be aggravated by routine physical activity such as going up stairs. This type of headache is thought to occur in the central nervous system.
Tension-type: Tension-type headaches are the most common primary headache disorder and can last anywhere from thirty minutes to seven days. These can often have a pressing or tightening quality that occurs on both sides of the head. Typically, there is no nausea, vomiting, or aggravation with physical activity, however, light or sound sensitivity can occur. This type of headache is thought to occur in the central nervous system but can have a hereditary component and is usually associated with muscle tender points. Tension – type headaches can be treated with relaxation techniques such as Progressive Muscle Relaxation (PMR), medications, and physical therapy.
The most common secondary headache that is not related to a serious medical condition is a cervicogenic headache (originating from the neck).
Cervicogenic Headache: The length of time a cervicogenic headache can last varies. Here the pain is on one side and usually starts in the neck. This type of headache is aggravated or preceded by head postures or movements of the neck. Due to the nerves of the neck and face sharing common connections, pain signals sent from one region can lead to discomfort in the other. Physical therapy can be an effective treatment to help relieve symptoms. For example: posture, exercise, ergonomics, massage, manual techniques, traction, trigger point, and acupressure.
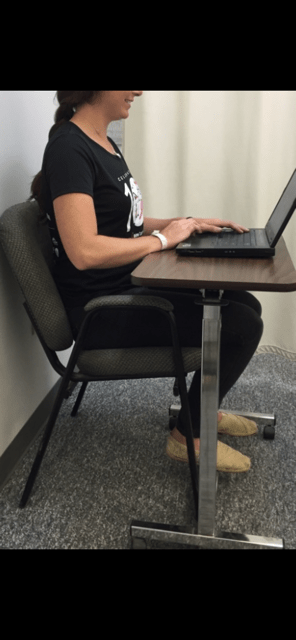
A cervicogenic headache can be caused by an accident or trauma or can stem from neck movement or sustained postures. Sustained postures could mean sitting in front of a computer at work or looking down at your phone. Changing these postures throughout the day could help reduce symptoms. Changing postures could mean bringing your phone closer to you using pillows or another supportive surface when reading or checking social media. If you are someone who works at a desk, it could involve taking breaks or getting a standing desk. However your life requires you to move, there are some simple and effective exercises you can perform throughout the day to help cervicogenic headache symptoms.
Progressive Muscle Relaxation: PMR is an effective method for reducing tension throughout the body. With this method you first tense a muscle group, such as at the neck or shoulder, and then relax the muscles noting the difference between the two. This helps reduce both stress and tension. For more information or to learn how to do PMR, refer to podcast at: https://www.psychologies.co.uk/try-progressive-muscle-relaxation
Manage your stress level: While stressors vary from person to person, one method for managing stress is with exercise. Any form of exercise can help reduce stress, but a cost free method is aerobic exercise such as walking or running. A less time consuming method could be to perform deep breathing exercises throughout the day.
Heat or cold: When feeling sore or stiff, applying a hot or cold pack or taking a hot shower can help ease a tension headache.
Posture: Some tips for posture are to make sure your head is over your shoulders rather than sitting forward and making sure you are sitting or standing up straight with your shoulders back.
Over the counter medications: Talk to your doctor or pharmacist for additional information.
Posture: See tips listed under tension headaches.
Ergonomics: If your job or hobbies require you to sit for extended periods it may be beneficial to change positions throughout the day or consider getting a standing desk. Also, limit time on electronic devices. When sitting make sure the monitor is at eye level, your legs are able to fit under your desk, and you are close to the keyboard and monitor. If you are working with a laptop or phone, avoid putting it on your lap. Instead, bring your laptop closer to you by putting pillows on your lap or using an ergonomic desktop. See photo below.
Exercise: Some exercises to help relieve symptoms are chin tucks, shoulder blade pinches, and back extension. These exercises can be performed multiple times throughout the day in sitting or standing.
Physical Therapy: Physical therapy may include massage, manual techniques, stretching, traction/ decompression and exercise. A physical therapist can assess your posture and provide strategies specific to you.
Over the counter medications: While medication may not cure cervicogenic headaches, they may help relieve pain. Talk to your doctor or pharmacist for additional information.
Visit your doctor regularly and listen to your body.

Dr. Chua is a neurologist and headache specialist at Geisinger Health System in Northeast Pennsylvania. In addition to caring for people with headache and facial pain disorders, Dr. Chua also serves as: Director of Headache Medicine at Geisinger, Clinical Director of Neurology at Geisinger Wyoming Valley, faculty at Thomas Jefferson University’s Advanced Headache Diagnosis and Management Post-Graduate Certificate Program, and Treasurer and Executive Board Member of the Association of Migraine Disorders. In her spare time, she enjoys going on adventures with her husband and toddler, learning new skills (she is now certified in battlefield acupuncture), and buying great books she will never have time to read!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
We’ve all heard it before – encouragement to exercise to trim our waistline or to speed up our metabolism. However, there may be more benefit to lacing up those sneakers than you’d think. Recent studies have established a link between exercise and cognition, making physical activity even more important.
Exercise has been shown to improve sleep and mood, decrease stress, and even increase libido. It also can bolster our self-esteem and ability to problem-solve and to remember details. In fact, strength training has even been shown to reverse cognitive decline to a degree in aging adults with mild impairment. Though the medical community is still trying to elucidate exactly how exercise boosts our brains physiologically, increased circulation to the brain and modulation of the hypothalamus-pituitary-adrenal axis that regulates the body’s response to stress have been implicated as the bearers of benefit. While exercise can be advantageous for everyone, it perhaps is even more valuable to those struggling with mood disorders. Exercise can help combat anxiety and depression and quell the symptoms of Attention Deficit Hyperactivity Disorder and Post Traumatic Stress Disorder as it helps the brain to pump out neurotransmitters and pain-fighting endorphins. Exercise makes addiction management easier, as well, and has recently been shown to help alcoholics lessen consumption.
So, how much exercise exactly is enough to illicit tangible cognitive benefit, you ask? Any amount of weight lifting, running, walking, or yoga helps, but habitual activity helps the most. Studies cite that a few consecutive weeks of participation in a fitness regimen yielded notable, positive results in subjects. Try to make exercise part of your daily routine to encourage good fitness habits. If you find the idea of adopting a strenuous new fitness program intimidating or off-putting, have no fear. Moderate exercise is enough to do the trick. The Mayo Clinic cites both brisk walking and mowing the lawn as examples of moderate activity, so an average fitness level is adequate for yielding positive mental results.
If you’re thinking about beginning an exercise program for the first time, start gradually. Begin with walking for 10 to 15 minutes twice daily, and add 1 or 2 minutes to your session every time you walk until you can walk continuously for 45 to 60 minutes. The same principle can be used when beginning other fitness routines involving biking, swimming, running, etc. Begin a weight training program to strengthen bones and tendons using 3 to 5 pound dumbbells, and increase the weight you use by a pound once you can easily perform 30 consecutive repetitions. Be careful to pay close attention to posture and form. Contact your physical therapist or a personal trainer for assistance with designing an appropriate exercise program. Don’t hesitate to contact your physician, either, if you have questions about whether a particular exercise program is safe and suitable for your age group or current fitness level. Consider these tips to make the most of your workout:
Guest Contributor: Leanne Woiewodski, MD, graduate, GCSOM
Sources:
US National Library of Medicine, National Institutes of Health, Helpguide.org, IDEA Health & Fitness Association, Mayo Clinic, Public Library of Science

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Spring is here! So, too, is allergy season and spring sports! It seems this every year at this time a young little league baseball player wheezes as they cross home plate and desperately tries to catch their breath. Players, coaches, umpires, parents watch in dismay, deciding whether they need to call an ambulance. Minutes later the player recovers from this scary situation…until the next time. Could this be an example of exercised-induced asthma (EIA)?
Dr. Gregory Cali, a local pulmonologist, (lung doctor) was gracious enough to participate in an interview about this problem…exercise-induced asthma (EIA). The topic was chosen in response to an email question from a concerned mother of an athlete with asthma. Dr. Cali informed me that the first thing to know about exercise induced asthma (EIA) is that EIA is not a distinct disease in itself-but is one manifestation or presentation of asthma. Putting it simply, EIA occurs in patients who have develop narrowing of the bronchial tubes ( bronchoconstriction) when they exercise. Some experts would rather we use the phrase exercise induced bronchoconstriction which is what happens when someone has an asthma attack. This bronchoconstriction occurs because of spasm of the tiny muscles of the airways, plugging of the airways with thick mucous, and swelling or edema of the cells lining the airways.
In fact, it is inflammation of the airways, mostly due to allergies, that is at the root of most cases of asthma. This inflammation causes the bronchial tubes to become over-reactive-and predisposed to narrowing- when exposed to certain triggers. Exercise is one of those triggers in susceptible people. The patient with EIA complains of chest tightness, wheezing, and shortness of breath when exercising. Some patients only experience coughing with exercise. Symptoms are usually worse in cold, dry air. This is believed to be due to the drying and cooling of the airways, which occurs with exercise, especially if the patient opens his or her mouth while exercising. Nasal breathing is much better at warming and humidifying air and may help to reduce EIA.
Dr. Cali feels that the most important point about EIA is to make sure a specific diagnosis is made. It is difficult at times to differentiate asthma from the normal breathlessness, which occurs with exercise. The feature of EIA that distinguishes it from normal breathing, or being "out of shape" is the fact that EIA is ALWAYS associated with a decrease in airflow. This can be measured with either a peak flow meter or a spirometer. It is also important that a specific diagnosis be made so that a person will not be labeled as asthmatic when they may be "normal" or have other conditions such as heart problems or anemia.
Dr. Cali also recommends before a person is labeled asthmatic, they have spirometric testing. An improvement in airflow after inhaling. A bronchodilator is an important indicator of asthma. Sometimes a bronchial challenge test is needed to diagnose asthma. In this test, the subject breathes in a known bronchoconstrictor in small quantities and the response is noted. Patients with asthma almost always respond to the inhaled agent by a reduction in airflow.
Inform Coaches – If coaches are made aware, than they can be prepared for the onset of EIA. Provide emergency contacts and medications with instructions, such as inhalers, should be available.
Warm and Moisten Air - Whatever the patient can do to warm and moisten the inhaled air can help prevent EIA. Nose breathing during exercise or wearing a loose covering over the mouth in cold weather may help. Sometimes, in severe cases, switching to an indoor sport like swimming may be necessary.
Start Out Slowly - It is important to start out slowly and warm up first before exercising at full tilt. Slowly jog around the track or field before practice or a game to prepare your lungs for full-speed.
Medications – are often necessary. Quick- acting bronchodilators like Albuterol, used 15-20 minutes before planned exercise, is recommended. This can be repeated once more during the exercise, but if tightness or wheezing occurs, the exercise should be stopped. Many patients with asthma require preventative treatment with anti-inflammatory medications. Inhaled steroids and/or leukotriene inhibitors may have to be added if the asthma is not controlled with Albuterol alone. In fact, some patients with asthma who are overly reliant on quick acting bronchodilator medications can get into serious trouble if they do not use inhaled steroids. Be sure to communicate your needs with your coaches.
Play Smart - In conclusion, people with asthma should not shy away from exercise. With proper precautions, people with asthma should be able to participate in all kinds of sports activities: baseball, football, soccer, swimming, tennis and running (even a marathon)! The key point is that the asthma needs to be under control and monitored by the patient, parents, coaches and doctor as a team.
Visit your doctor regularly and listen to your body.
Medical Contributor: Gregory Cali, DO, pulmonary specialist, Dunmore, PA

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!