Pain is different than discomfort! Muscle soreness and “feeling the burn” can occur during a normal healthy exercise routine. However, you should never experience a sharp, deep, intense, or lingering pain during or after exercise. In fact, if the soreness lasts more than 24-48 hours, than you did more damage than benefit to your muscles and other tissues and it is time to scale back and take time off. If necessary, use RICE (rest, ice compression and elevation). It is important to get in tune with your body and learn the difference between muscle strain and fatigue discomfort and pain from soft tissue damage from overuse and overload. Find the proper amount of weight and repetitions and gradually increase over time.
There is no solid evidence that stretching alone before a sport or activity prevents injury. In fact, over stretching may be counterproductive before a sport as it may weaken the muscle. The current wisdom on the matter is; never stretch a cold muscle. Instead, warm up for 5-10 minutes by actively moving the extremities and light jogging or biking and THEN lightly stretch the arms, legs, back etc. More vigorous stretching should be performed to improve the flexibility of tight muscles (ie calf and hamstring muscles) and best done after your workout but not before a sporting activity (tennis, basketball, etc.).
It depends on your body type and hormones! It is very unlikely that women and prepubescent males will bulk up from lifting weights…especially light weights (blame or thank hormones). It will, however, increase metabolism and fat burning efficiency which can lead to weight loss and good muscle tone. Stick with low resistance and high repetitions for best results.
It is not possible to target an area of the body to burn more fat! It is very common for women to ask for a specific exercise to reduce the fat in their buttocks, thighs, and abdomen. Regretfully, it is not possible to target weight loss in these areas or other body parts. In fact, when you lose weight through diet and exercise, the caloric expenditure will be evenly distributed throughout the body. However, once the adipose tissue in a specific part of the body such as the abdomen is reduced from general weight loss, targeting the area with exercises specific to that muscle group will improve the tone and definition for a leaner look in that region.
Sure, it would be great to dedicate 60 minutes 5 -6 days a week for exercise. But for most of us who work and raise a family it is not practical. The good news is that the research supports 30 minutes of exercise 3-5 days a week. Moreover, evidence shows that 10 minutes, three times a day, 5 days per week will help you attain the 150 minutes a week supported in most exercise studies.
Most people with the most common form of arthritis, osteoarthritis, feel better when they are moving. That is not to say that they don’t have increased symptoms when they OVERDO it. An exercise program specifically designed for a person’s problem and limitations will improve their symptoms and function. For example, if an individual has arthritis in their knees, they should use an exercise bike (partial weight bearing) or swim (buoyancy effect of water) instead of walk or run (full weight bearing) for aerobic exercise.
Furthermore, they would do far better with light cuff weights in a sitting or lying position to strengthen their legs than performing squats or lunges. It is important to remember, the weight gain and joint weakness and stiffness associated with a sedentary lifestyle will do more harm to an arthritic joint than a proper exercise program.
Not unless you are planning a killer workout! The number one reason most of us exercise is to lose or control body weight. High calorie sports drinks are counterproductive and unnecessary. If you do not plan on exercising for more than 60 minutes, good old fashion H2O is more than adequate. However, if you plan to do a “killer” workout for more than 60 minutes and may incorporate a high intensity interval training (HIIT) program, than a sports drink with electrolytes and other nutrients, may be of value.
For most of us, effective resistance training is not about the equipment. It is safe to say, caveman was pretty fit and strong despite the fact that he never went to a gym and lifted weights. He did however, lift, push, pull, and carry heavy stones, timber, and animals for day-to-day survival. So too, it is for modern man, the body does not distinguish between the resistance provided by a elastic band, dumbbell, or cable with pulleys and weight stacks. As long as the basic principles of strength training are applied, (isolating a muscle or muscle group, loading the muscle with enough force to bring it to fatigue without causing tissue damage, and allowing for adequate rest and recover) than the muscle will gain strength regardless of the type of resistance.
First, let me confess that I love to run and up until recently, ran almost daily. However, now that I am over 60, I had to find new forms of aerobic exercise which would be kinder and gentler to my joints. So, I mix it up between biking (indoors and outdoors, recumbent and upright), brisk walking or hiking, elliptical and stepper and swimming laps. Again, like the caveman weightlifting example, the body (heart and lungs) does not know what is causing an increase in heart rate for 30, 45 or 60 minutes, it only knows that it must respond to allow the body to function under this stress. And, in the process it becomes conditioned to the point that it will work much more efficiently when not under stress with a lower heart and respiratory rate and blood pressure at rest.
Those over 50 would be well-advised to engage in low-impact aerobics on a regular basis. For example, if you want to run two to three days per week, do not run two days in a row and consider performing low impact exercise in between. Some examples of low impact aerobics are walking, treadmill walking, swimming, elliptical trainer, and an exercise or road bike.
Change is necessary with age! For many years, I have repeatedly preached about the value of engaging in an active lifestyle throughout life. It is especially important to be active as one gets older to maintain mobility and independence. However, many take this advice to an extreme and refuse to accept the inevitable changes that occur in the body with age. They run, jump, lift and throw like a teenager and often fail to modify their activity or exercise regimen appropriately for their age. Consequently, they suffer from multiple injuries, including muscle tears, tendonitis, bursitis, impingement, and advanced osteoarthritis.
Keep in mind, everyone ages differently. One person at 60 years of age may be the equivalent of another at 50. However, change with age is inevitable, so be kind to your body…it’s the only one you have! It is always prudent to consult your physician and physical therapist for a program designed specifically for your needs.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
Access all of Dr. Mackarey's articles in our Health Care Forum!
PEOPLE WILL OFTEN ASK ME, “IS THERE SUCH A THING AS AN EXERCISE RUT?” THEY WANT TO KNOW WHY THEY DO NOT SEEM TO BE IMPROVING WITH THEIR EXERCISE PROGRAM…they exercise 3-4 times a week for 30 to 45 minutes and they feel frustrated and STUCK in a rut.
The purpose of this column will be to offer suggestions on how to improve or get more out of a “stale” exercise program. Last week’s column offered tips to improve a stale cardiovascular and strength program. This week we will discuss flexibility and functional training tips and include the components necessary for a healthy mind, body and spirit connection.
Flexibility training involves the careful stretching of the muscles, tendons and joints to improve the range of motion in order to safely perform daily activities and sports without injuring or tearing soft tissues. It is probably the most neglected part of the fitness program. However, while the amount of inherent flexibility varies for each person, a minimal range is necessary as it relates to daily activities and sports. For example, as you age it is important to have enough flexibility in your back, hips and knees to wash your feet, put shoes and socks on. Flexibility exercises should always be performed after a warm –up activity and done slowly and gently.
There are two types of flexibility exercises; dynamic and static. Dynamic stretching is performed with movement such as pushing the ankle up and down like a gas pedal. Passive stretching is performed using an outside force such as using a towel to pull the ankle up in order to stretch the calf. Dynamic should be performed before an activity (before running or playing tennis) and static performed after the activity is over in order to increase range of motion for future activities.
In conclusion, it is easy for fitness enthusiasts to get so focused on maintaining a routine that they allow their program to become stale and ineffective. It is essential to reassess and update your program to prevent stagnation.
Make sure the routine has all three fundamental components of a well-balanced exercise program; cardiovascular, strength and flexibility training. Moreover, to be truly healthy, one must work toward a “Healthy Mind, Body, and Spirit. Therefore, in addition to traditional exercise one must incorporate the following: nutrition; meditation, relaxation techniques, yoga, core fitness; functional/sports specific training; leisure sports and activities
In order to prevent an exercise program from getting stale, one must incorporate all aspects of wellness…a healthy mind, body and spirit!
While each component offers its own specific benefit, the combination of all three cooperatively provides unique value. Too often, fitness enthusiasts concentrate on the exercises they LIKE or are good at more than the ones they NEED.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine
For all of Dr. Mackarey's articles our Health Care Forum
People will often ask me, "Is there such a thing as an exercise rut?" They want to know why they do not seem, to be improving with their exercise program?... they exercise 3-4 times a week for 30 to 45 minutes and they feel frustrated and STUCK in a rut. While initially responding favorably to exercise, after 6 -9 months or more, they do not notice progress in weight loss, strength, tone, endurance or daily function.
Here are a few suggestions on how to improve or get more out of a “stale” exercise program.
Step one is to build an exercise program that is grounded in the basics. Next, Step two, which begins after the basics have been mastered, includes the components necessary for a healthy mind, body and spirit connection and translates into functional activities of daily living including work and leisure sports.
Make sure your routine has all three fundamental components of a well-balanced exercise program:
While each component offers its own specific benefit, the combination of all three cooperatively provides unique value. Too often, fitness enthusiasts concentrate on the exercises they LIKE or are good at more than the ones they NEED. A well-balanced program includes what you like and need!
In fact, recent studies show that those performing all three components surpassed those performing one or any combination of two of the training types when tested for efficient:
Cardiovascular exercise is any activity that raises your heart rate and respiratory rate. This type of exercise strengthens the heart muscle and the muscles that assist in breathing. When these muscles are stronger, they in turn work more efficiently to deliver oxygen to your muscles and other parts of the body. Ultimately, these oxygenated muscles can work harder and longer to burn fat during exercise and at rest.
*Most experts recommend at least 30 minutes of sustained cardio, 3-4 days per week. However, recent studies support the notion of performing 10-15 minutes, twice daily, 4 days per week. For those “stuck” in a fitness rut, to advance your program, cardio should be performed 5-6 days per week for 45-60 minutes.
Strength training is an activity that provides any type of resistance to muscle contraction to build strength in the muscle. The resistance can be without movement against an immovable object such as pushing against a wall (isometric) or with movement such as lifting up or lowering a weight down against gravity (isotonic/dynamic). There are two types of isotonic muscle contraction; concentric, which involves raising the weight against gravity as the muscle shortens and eccentric which involves lowering a weight against gravity as the muscle lengthens.
A standing biceps curl is an example that incorporates both concentric and eccentric contractions. A progressive strength training program includes all three types of muscle contraction. By using the classic bicep muscle curl these photos will demonstrate all three types of muscle contraction:


Sources: National Institutes of Health; American Council on Exercise
Model: Heather Holzman

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” Next Week: Read Stuck in an Exercise Rut…Part II of II!
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine
For all of Dr. Mackarey's articles visit: Mackarey's Health and Exercise Forum!
We are more than one month into the New Year and many people are still talking about their health and fitness goals. As you probably know, losing weight and getting fit are the most popular resolutions, however, for many who have not maintained an active lifestyle in years, it is challenging to know where to begin. Moreover, beginning without a good plan can lead to injury and leave you discouraged. For example, those overweight and de-conditioned should not start a walking program to aggressively. Walking at a fast pace and long distance without gradually weaning into it will most likely lead to problems.
There is probably nothing more natural to human beings than walking. Ever since Australopithecus, an early hominin (human ancestor) who evolved in Southern and Eastern Africa between 4 and 2 million years ago, that our ancestors took their first steps as committed bipeds. With free hands, humans advanced in hunting, gathering, making tools etc. while modern man uses walking as, not only a form of locomotion, but also as a form of exercise and fitness. It is natural, easy and free...no equipment or fitness club membership required!
“There’s no question that increasing exercise, even moderately, reduces the risks of many diseases, including coronary heart disease, breast and colon cancer, and Type 2 diabetes,” said Dr. Jennifer Joyce, MD, professor of family medicine at GCSOM. “Research has even shown that you could gain two hours of life for each hour that you exercise regularly.”
According to the American Heart Association, walking as little as 30 minutes a day can provide the following benefits:
Anything is better than nothing! However, for most healthy adults, the Department of Health and Human Services recommends at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous aerobic activity, or an equivalent combination of moderate and vigorous aerobic activity. The guidelines suggest that you spread out this exercise during the course of a week. Also aim to do strength training exercises of all major muscle groups at least two times a week.
As a general goal, aim for at least 30 minutes of physical activity a day. If you can't set aside that much time, try several short sessions of activity throughout the day (3 ten or 2 fifteen minute sessions). Even small amounts of physical activity are helpful, and accumulated activity throughout the day adds up to provide health benefit.
Remember it's OK to start slowly — especially if you haven't been exercising regularly. You might start with five minutes a day the first week, and then increase your time by five minutes each week until you reach at least 30 minutes.
For even more health benefits, aim for at least 60 minutes of physical activity most days of the week. Once you are ready for a challenge, add hills, increase speed and distance.
Keeping a record of how many steps you take, the distance you walk and how long it takes can help you see where you started from and serve as a source of inspiration. Record these numbers in a walking journal or log them in a spreadsheet or a physical activity app. Another option is to use an electronic device such as a smart watch, pedometer or fitness tracker to calculate steps and distance.
Make walking part of your daily routine. Pick a time that works best for you. Some prefer early morning, others lunchtime or after work. Enter it in your smart phone with a reminder and get to it!
Studies show that compliance with an exercise program is significantly improved when an exercise buddy is part of the equation. It is hard to let someone down or break plans when you commit to someone. Keep in mind that your exercise buddy can also include your dog!
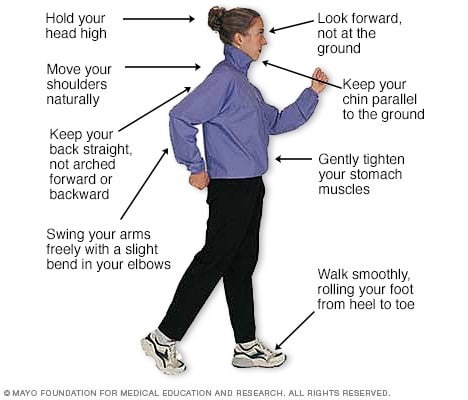
Like everything, there is a right way of doing something, even walking. For efficiency and safety, walking with proper stride is important. A fitness stride requires good posture and purposeful movements. Ideally, here's how you'll look when you're walking:
Sources : Sapiens.org; WebMD; Mayo Clinic
* Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine.
For all of Dr. Mackarey's articles: Visit our Healthcare Forum!
We all know someone who has been affected by a stroke. It can be a devastating and life-changing event. According to the National Stroke Association, (NSA) it is the 5th leading cause of death and number one cause of disability in the United States. Nearly 800,000 people in the USA have a stroke every year. Every 40 seconds someone has a stroke and every 4 minutes someone dies of a stroke in the USA. 897% of all strokes are ischemic from a clot or mass blocking a blood vessel in the brain.
According to a study in the Journal of the American Medical Association, there is almost a 50% reduction in strokes and 40% reduction in stroke deaths more than two decades from 1987 to 2011. THE GOOD NEWS: According to a study in the Journal of the American Medical Association, there is almost a 50% reduction in strokes and 40% reduction in stroke deaths more than two decades from 1987 to 2011. Improved smoking cessation, management of high blood pressure and cholesterol are believed to be significant contributing factors. THE BAD NEWS: Progress has slowed in recent years! THE MESSAGE: Continued vigilance and lifestyle changes are essential!
While the signs and symptoms vary, most people experiencing a stroke have several if not all of these symptoms in various parts of the body.
F – Face Drooping – ask for a smile to see if one side droops
A – Arm weakness or numbness
S – Speech – can the person repeat a simple sentence? Do they slur?
T – Time = Brain Damage! Time to Call 911
If the above signs or symptoms have been identified than there is a medical emergency - Immediately Call 911
Strokes can happen at any age, even to babies in the womb. Still, the odds of a stroke climb quickly after middle age.
Visit your doctor regularly and listen to your body.
Keep moving, eat healthy foods, and exercise regularly

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice in downtown Scranton, PA and is an associate professor of clinical medicine at GCSOM.
When a patient comes to our physical therapy clinic with lower back pain it is standard protocol to take a thorough history and complete a neurological exam. This is especially important if the patient has leg pain, tingling or numbness in one or both legs referred from their lower back. During the history, the patient will often report an increase in symptoms in their legs at night in bed. They report pain, tingling, a need to constantly move their legs. While some of these symptoms are associated with lower back pain and “sciatica” others, such as the urge to constantly move the legs, is not. This may be a symptom associated with another problem such as restless legs syndrome or RLS.
Recently, more information has become available on restless legs syndrome (RLS). According to the RLS Foundation, RLS is a neurological condition suffered by approximately 10% of the population in the United States. It is considered a central nervous system disorder. There are many manifestations of this disease. Some people suffer only mild symptoms creating urges to move their legs in bed at night. Others suffer severe symptoms of uncontrollable urges to move their legs sitting or lying. The problem may lead to insomnia, disrupted sleep, distress and fatigue.
Genetic among first-degree relatives: This type develops earlier in life and the symptoms are more severe. There is also an iron deficiency associated with genetic RLS.
Non-inherited or idiopathic. This type is more associated with aging. There are several criteria to diagnose RLS. Also, there are medications and other treatment options available for RLS. Exercise, including stretching, walking and weight-training can be very effective.

Read Dr. Mackarey’s Health & Exercise Forum – every Monday
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit MackareyPhysicalTherapy.com
The “first Thanksgiving” was in 1621 between the Pilgrims of Plymouth Colony and the Wampanoag tribe in present day Massachusetts to celebrate the harvest and other blessings of the previous year. In 1789, President George Washington, at the request of Congress, proclaimed Thursday, November 26, as a day of national thanksgiving. In 1863, Abraham Lincoln proclaimed the national holiday of Thanksgiving to be the last Thursday of November.
Americans and Canadians continue to celebrate this holiday as a time for family and friends to gather, feast, and reflect upon their many blessings. Like most, I am very grateful for the simple things; family, good friends, food, shelter, and health. This year, I am also thankful for the dedicated scientists who developed the COVID 19 vaccination so we can safely enjoy Thanksgiving with our families. It turns out that being grateful is, not only reflective and cleansing; it is also good for your health!
Grateful people are more likely to behave in a prosocial manner, even when it is not reciprocated. A study by the University of Kentucky found those ranking higher on gratitude scales were less likely to retaliate against others, even when others were less kind. Emmons and McCullough conducted one of the most detailed studies on thankfulness. They monitored the happiness of a group of people after they performed the following exercise:
There are many things in our lives, both large and small, that we might be grateful about. Think back over the past week and write down on the lines below up to five things in your life that you are grateful or thankful for.” The study showed that people who are encouraged to think of things they’re grateful for are approximately 10% happier than those who are not.
Conclusion: Amy Morin, psychotherapist, mental health trainer and bestselling author offers this advice: “Developing an “attitude of gratitude” is one of the simplest ways to improve your satisfaction with life. We all have the ability and opportunity to cultivate gratitude. Simply take a few moments to focus on all that you have, rather than complain about all the things you think you deserve.” So…be grateful and have a happy Thanksgiving!
Source: NIH, Forbes, Amy Morin “13 Things Mentally Strong People Don’t Do.”

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's
November is National Chronic Obstructive Pulmonary Disease (COPD) month. COPD is the fourth leading cause of death in the United States, according to the Centers for Disease Control and Prevention. This problem refers to a group of lung diseases that causes damage to the airways and air sacs in the lungs. People with COPD suffer from diminished airflow and difficulty breathing. Emphysema and chronic bronchitis are two of the most common types of COPD. The damage can't be reversed, so treatment includes medications and lifestyle changes designed to control symptoms and minimize further damage, according to the Mayo Clinic.
Exercise is an important part of life for those with COPD because it improves the overall strength and endurance of respiratory muscles. When you exercise, muscles adapt and use oxygen more efficiently so your lungs don't have to work so hard. Also, in addition to improvement in breathing, exercise boosts mental health, helps maintain a healthy weight and blood pressure, and improves circulation. Most importantly, exercise will improve your quality of life with COPD. Before you begin an exercise program, see your family physician or pulmonologist for approval. Then, see a physical therapist to design a program specific to you needs. Always begin slowly and rest if you get short of breath, have chest pain, feel dizzy or sick to your stomach.
While not all of these endurance exercises may be appropriate for you, one or two of these may offer a good starting point.
Walk Around the House – Start walking around the house for 1-2 minutes nonstop. Every 1-2 hours. Then, add 1-2 minutes every week.
Static Marching – hold onto the countertop or back of chair and march in place for 30 seconds. Rest 1-2 minutes and repeat. Do 5 cycles. Add 5-10 seconds every week.
Climb the Steps – If you can do so safely, use the steps for exercise 1-2 times per day. Then, add 1-2 times per day.
Walk the Mall/Treadmill – If you are able to get out of the house and can tolerate more extensive endurance exercises, get out and walk the malls or use a treadmill.
Recumbent Bike – If balance is a problem, but you can tolerate more extensive. Endurance exercise, use a recumbent bike (a bike with a backrest)
Walking is free exercise and can be done in some form by almost everyone…even with an assistive device such as a cane or walker. For those with COPD who are active and fit – walk 4-5 days per week for 30 to 45 minutes. Less fit individuals can walk for 15 to 20 minutes. For those with COPD who are in poor condition and have significant SOB – walk for 2-3 minutes (to the bathroom or around the house) every 30 to 45 minutes. Try not to sit for 60 minutes without getting up and walking around.
Posture exercises are designed to keep your body more upright and prevent rounded shoulders and forward head/neck. More erect posture promotes better breathing. Perform 5 repetitions each 3 -5 times per day
Row-The-Boat - Pinch shoulder blades together as if you are rowing a boat.
I-Don’t-Know – Shrug shoulders up toward the ears as you do when you say “I don’t know.”
Chin Tucks – Bring your head back over your shoulders and tuck your chin in
Bicep Curls – sit in chair and bend your elbows up and down with a can of peas in your hands
Wrist Curls – as above but bend your wrists up and down
Chair Push-ups – Push up with your arms to get out of a chair
Saw Wood – pull a light resistance band (yellow) back from a door knob as if you were sawing wood.
Hip Hikes – Sit in chair and march by hiking your hip and lifting up your heel 4-6 inches off the floor
Leg Kicks – Sit in chair and kick your knee out straight – then bend it down to the floor
Hips Out and In – Sit in chair and bring your knees in and out against a resistance band
Toe Raise/Heel Raise – Sit in chair and raise your toes up – then raise your heels up
Diaphragmatic Breathing - The diaphragm muscle is essential for breathing. While sitting or lying down, put one hand on your abdomen and the other on your chest. Slowly inhale through your nose and try to separate the hand your stomach from the hand on your chest. Then, slowly exhale through pursed lips.
Pursed Lipped Breathing - breathe in through your nose slowly for 3- 5 seconds. Then, purse your lips as though you're going to whistle. Lastly, exhale slowing through the pursed lips over 5 to 10 seconds.
“Better Breathers Club,” in conjunction with the American Lung Association, offers a free local support group to help patients and their families suffering from COPD and chronic lung disease. For more information contact the American Lung Association at www.lung.org

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice in downtown Scranton, PA and is an associate professor of clinical medicine at GCSOM.
According to the World Health Organization about half of the world’s adult population has had a headache at least once in the past year. Prolonged use of electronic devices has greatly contributed to this problem. For many people, these headaches are infrequent and do not often affect daily life. But what about when your headache occurs frequently or is so severe it prevents you from going about your day to day activities? Some types of headaches are more easily treated and managed than others.
There are two types of headaches: primary and secondary. Primary headaches occur without an underlying disease and include migraines and tension-type headaches. Secondary headaches can be associated with serious disease, requiring emergency care, or can be referred from other structures of the body such as the cervical spine (neck).
Headaches symptoms that may constitute a medical emergency are: vomiting, seizures, fever, muscle pain, night sweat, weight loss, and neurologic symptoms such as blurred vision. If you are experiencing any of these symptoms, if your headache worsens, or your symptoms change it is recommended that you seek medical attention. Any headache that is unusual for you and does not resolve itself in a reasonable time should be brought to your primary care physician’s attention.
Migraines: Migraines are a primary form of headache that typically lasts from four to seventy two hours, can range from moderate to severe pain, and typically are located on only one side of the head. Often they can be accompanied by an aura, nausea or vomiting, sensitivity to sound, or light sensitivity. Migraines can be aggravated by routine physical activity such as going up stairs. This type of headache is thought to occur in the central nervous system and is related to blood vessels.
Tension-type: Tension-type headaches are the most common primary headache disorder and can last anywhere from thirty minutes to seven days. These can often have a pressing or tightening quality that occurs on both sides of the head. Here there is no nausea, vomiting, light sensitivity, or aggravation with physical activity. This type of headache is thought to occur in the central nervous system but can have a hereditary component and is usually associated with muscle tender points. Tension – type headaches can be treated with relaxation techniques such as Progressive Muscle Relaxation (PMR), medications, and physical therapy.
The most common secondary headache that is not related to a serious medical condition is a cervicogenic headache (originating from the neck).
Cervicogenic Headache: The length of time a cervicogenic headache can last varies. Here the pain is on one side and usually starts in the neck. This type of headache is aggravated or preceded by head postures or movements of the neck. Due to the nerves of the neck and face sharing common connections, pain signals sent from one region can lead to discomfort in the other. Physical therapy can be an effective treatment to help relieve symptoms. For example: posture, exercise, ergonomics, massage, manual techniques, traction, trigger point, and acupressure.
A cervicogenic headache can be caused by an accident or trauma or can stem from neck movement or sustained postures. Sustained postures could mean sitting in front of a computer at work or looking down at your phone. Changing these postures throughout the day could help reduce symptoms. Changing postures could mean bringing your phone closer to you using pillows or another supportive surface when reading or checking social media. If you are someone who works at a desk, it could involve taking breaks or getting a standing desk. However your life requires you to move, there are some simple and effective exercises you can perform throughout the day to help cervicogenic headache symptoms.
5 TIPS FOR TENSION HEADACHES
Progressive Muscle Relaxation: PMR is an effective method for reducing tension throughout the body. With this method you first tense a muscle group, such as at the neck or shoulder, and then relax the muscles noting the difference between the two. This helps reduce both stress and tension. For more information or to learn how to do PMR, refer to podcast at: https://www.psychologies.co.uk/try-progressive-muscle-relaxation
Manage your stress level: While stressors vary from person to person, one method for managing stress is with exercise. Any form of exercise can help reduce stress, but a cost free method is aerobic exercise such as walking or running. A less time consuming method could be to perform deep breathing exercises throughout the day.
Heat or cold: When feeling sore or stiff, applying a hot or cold pack or taking a hot shower can help ease a tension headache.
Posture: Some tips for posture are to make sure your head is over your shoulders rather than sitting forward and making sure you are sitting or standing up straight with your shoulders back.
Over the counter medications: Talk to your doctor or pharmacist for additional information.
5 TIPS FOR CERVICAL HEADACHES
Posture: See tips listed under tension headaches.
Ergonomics: If your job or hobbies require you to sit for extended periods it may be beneficial to change positions throughout the day or consider getting a standing desk. Also, limit time on electronic devices. When sitting make sure the monitor is at eye level, your legs are able to fit under your desk, and you are close to the keyboard and monitor. If you are working with a laptop or phone, avoid putting it on your lap. Instead, bring your laptop closer to you by putting pillows on your lap.
Exercise: Some exercises to help relieve symptoms are chin tucks, shoulder blade pinches, and back extension. These exercises can be performed multiple times throughout the day in sitting or standing.
Physical Therapy: Physical therapy may include massage, manual techniques, stretching, traction/ decompression and exercise. A physical therapist can assess your posture and provide strategies specific to you.
Over the counter medications: While medication may not cure cervicogenic headaches, they may help relieve pain. Talk to your doctor or pharmacist for additional information.
Contibutor: Alexa Rzucidlo, PT, DPT

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine (formerly The Commonwealth Medical College).
As more of us become more comfortable living with COVID 19, travel plans have exploded. For 2 ½ years many have put air travel for family vacations on hold and we are eager to get back to air travel. As you may have gathered from my previous columns, travel is one of my passions. My family and I have been fortunate to have visited many spiritual places of natural wonder and beauty that we call our National Parks. Many of the parks are on the west coast and require some preparation to endure the many hours of travel by airplane through different time zones. Moreover, travel to other countries and continents, often requiring 8, 10, 16 or more non-stop hours on a plane can really take a toll on your mind and body and gave new meaning to the term “jet lag.”
According to the Mayo Clinic, jet lag, also known as jet lag disorder, is a sleep disorder that can occur in people who travel through different time zones in a short period of time, such as a flight from New York City to Los Angeles. Obviously, the further the distance traveled and the more time zones entered, the more significant and drastic the symptoms, as found, for example, in those traveling from the United States to Asia.
Sunlight has a direct impact on our internal clock by regulating melatonin, a hormone that regulates sleep and wake cycles in the body. Travel through different time zones can affect the amount and duration of sunlight and therefore, impact the regulation of these cycles. The inability to regulate the cycles results in many symptoms.
Posture exercises are designed to keep your body more upright and prevent rounded shoulders and forward head/neck.

Read Dr. Mackarey’s Health & Exercise Forum – every Monday
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.