Patients often tell me that they would like to exercise but hesitate due to their knee or hip pain. They want to know what type of exercise is best for those suffering from osteoarthritis (OA). Osteoarthritis is also known as degenerative arthritis. It is the most common form of arthritis in the knee. It is usually a gradual, slow and progressive process of “wear and tear” to the cartilage in the joint which eventually wears down to the bony joint surface. It is most often found in middle-aged and older people and in weight bearing joints such as the hip, knee and ankle. It causes gradual onset of pain, swelling and stiffness in the involved joint, especially after increased activity and weakness with loss of function due to disuse.
However, OA is not an excuse to avoid exercise but it is important to be smart about it. Regular exercise is essential to maintain a normal lifestyle for those with OA. However, if you do the wrong exercise, use poor technique, or are too aggressive, you could flare-up your joints and do more harm than good.
When performed correctly, exercise for those with OA has many benefits:
Pain Control
Exercise controls OA pain by releasing natural pain control chemicals in the body called endorphins. It also controls pain by assisting in weight loss and improving range of motion.
Weight Control
We all know how well exercise burns calories and that increased body weight creates increase stress on the joints.
Prevention of Joint Stiffness
Exercise will help maintain joint range of motion. A stiff joint is a painful joint.
Prevention of Muscle Weakness
Exercise will help maintain muscle strength. Weak muscles will allow or increase in joint wear and tear.
Maintain Lifestyle
If a joint is stiff and weak, then they become painful which negatively impacts your lifestyle. Exercise can prevent this problem.
Start Slowly
Wean into exercise because if you advance too quickly, you will flare up the joint and have increased pain. For example, walk for 5-10 minutes the first session. If you do not have pain, add 1-2 minutes each session.
Lose Weight
Every pound lost equates to less stress on your joints. For example, a loss of 5 pounds of body weight translates to 20-30 pounds of stress through the knee, according to David Borenstein, MD, President of the American College of Rheumatology. Also, body weight has a direct impact on daily activities. For example, walking upstairs creates stress through the knee equal to 4 times body weight and seven times body weight going downstairs. Therefore, less body weight equals less stress.
Low Impact Workouts
Low impact exercise creates less stress on the joints while strengthening leg muscles and those who those who maintain leg muscle strength have less stress on their joints. It is even important not to load your arms with heavy objects when walking or using stairs to limit joint stress.
Some examples of low-impact exercises are: walking, swimming, elliptical trainer, and biking. Strength training is also low-impact and should be performed with low weight and high repetitions. Water therapy is great for those with OA, especially in a heated pool. It is a great low-impact exercise with less gravity and stress on the joints. Walk, swim and do mild resistance exercises in the water. Use a snorkel and mask for swimming to limit excessive neck turning and back extension.
Walking is a great form of exercise; however, walking softly is important for those with OA. Wear good running shoes and orthotics if necessary. Discuss this with your physical therapist or podiatrist. When possible, use soft surfaces like cinder, mulch or rubber. Avoid grass and soft stand due to instability and torsion that may irritate your joints.
Warm-Up
Warming up your body is critical to prevent injury to the muscles and tendons. This can be done by marching in place or using aerobic equipment such as a bike for 5 to 10 minutes before exercise. Always perform the warm-up activity at ½ your normal pace.
Balance & Relaxation Techniques
Tai Chi and ballroom dancing are two good examples of activities which promote balance and relaxation. Studies showed that those with OA who participated in Tia Chi two times a week for eight weeks reported less pain, increased range of motion and improved daily activities and function. They also noted less low back pain and better sleeping.
Proper Clothing
Stay warm in winter and consider wearing compression shorts. Be cool in the summer months with DrytechR type material.
Pre/Post Exercise First Aid
If you are sore for longer than 12 to 24 hours after exercise, then you overdid it and must make adjustments next time. Otherwise, use hot packs, bath or shower before you exercise to loosen up and apply ice to your joints after exercise, especially if they are sore.
Post Exercise Stretch
Gentle, active range of motion stretches after exercise is important to maintain mobility. Do not bounce or cause pain. For example: Low Back – knees to chest; Arms – row –the – boat, arms behind head, arms behind back; Legs – wall lean calf stretch, bend and extend knees, open and close hips.
SOURCES: Rothman Institute, Philadelphia, PA and American Academy of Orthopaedic Surgeons; www.lifescript.com
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
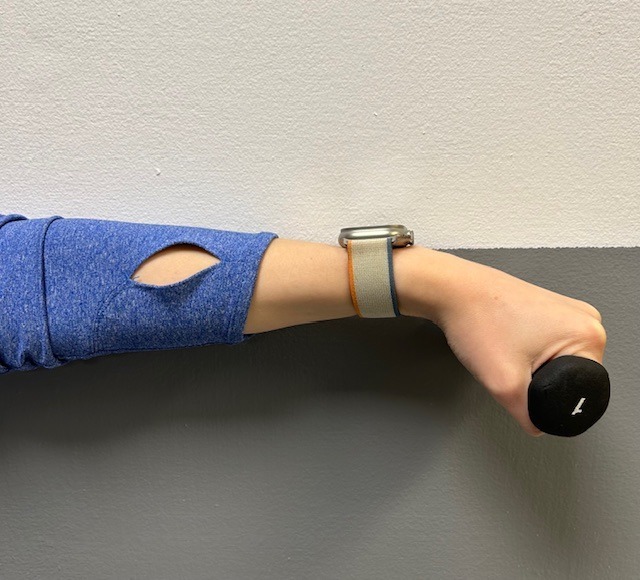
Tennis elbow, also called lateral epicondylitis, is an inflammation of the lateral (outside) bony protuberance at the elbow. It is at this protuberance that the tendon of the long muscles of the hand, wrist and forearm attach to the bone. As the muscles repeatedly and forcefully contract, they pull on the bone, causing inflammation. The trauma is irritating when working the muscles in an awkward position with poor leverage like hitting a backhand in tennis.
It is not unusual for a patient to come to my office with severe pain on the outside of their elbow. Especially, after intensifying their tennis workouts or changing the racquet string tension. Others come to me with pain on the inside of the elbow (“golfer’s elbow”) from wrist action that advanced golfer’s use at impact. However, this problem is not only for tennis players and golfers. Laborers working with wrenches or screwdrivers with an awkward or extended arm can also develop tennis elbow. Others who are vulnerable are: those working for hours at a computer using a mouse as well as those working hard maintaining their lawns and gardens.
In a more chronic problem, lateral elbow pain may arise by a degenerative condition of the tendon fibers on the bony prominence at the lateral elbow. Sporadic scar tissue forms from a poor attempt by the body to overcompensate and heal without eliminating the cause.
While symptoms may vary, pain on the outside of the elbow is almost universal. Patients also report severe burning pain that begins slowly and worsens over time when lifting, gripping or using fingers repetitively. In more severe cases, pain can radiate down the forearm.
Conservative treatment is almost always the first option and is successful in 85-90 percent of patients with tennis elbow. Your physician may prescribe anti-inflammatory medication (over the counter or prescribed). Physical/Occupational therapy, rest, ice, and a tennis elbow brace to protect and rest may be advised. Ergonomic changes in equipment, tools, technique and work-station may be necessary. Improvement should occur in 4-6 weeks. If not, a corticosteroid injection may be needed to apply the medication directly to the inflamed area. Physical therapy, range of motion, and stretching exercises may be necessary prior to a gradual return to activity. Deep friction massage can assist healing.

Exercises performed in a particular manner to isometrically hold and eccentrically lengthen the muscle with contraction.
New Conservative Treatment: Platelet-Rich-Plasma (PRP) is a new treatment for the conservative management of degenerated soft tissues that has recently received great media attention. In great part, due to its success in several high profile athletes. According to the Journal of the American Academy of Orthopaedic Surgeons,(JAAOS), platelet-rich plasma (PRP) is autologous (self-donated) blood with an above normal concentration of platelets. Normal blood contains both red and white blood cells, platelets and plasma. Platelets promote the production and revitalization of connective tissue by way of various growth factors on both a chemical and cellular level.
The actual PRP injection requires the patient to donate a small amount of their own blood. The blood is placed into a centrifuge (a machine that spins the blood at a high velocity to separate the different components of blood such as plasma, white and red blood cells), for approximately 15 minutes. Once separated, the physician draws the platelet-rich plasma to be injected directly into the damaged tissue. In theory, the high concentration of platelets, with its inherent ability to stimulate growth and regeneration of connective tissue, will promote and expedite healing.
Surgery for tennis elbow is only considered in patients with severe pain for longer than 6 months without improvement from conservative treatment. One surgical technique involves removing the degenerated portion of the tendon and reattaching the healthy tendon to bone. Recently, arthroscopic surgery developed to perform this technique. However, research does not support the value of one over the other at this point. Physical/occupational therapy is used after surgery. Return to work or athletics may require 4-6 months. More recently, a surgical technique using ultrasound to guide a needle to debride (clean) the area of scar tissue has been developed. If eligible for this procedure, the time required for healing, rehabilitation and return to activity is much shorter.
If you feel you suffer from tennis elbow, ask your family physician which of these treatment options are best for you.
Visit your doctor regularly and listen to your body.
EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy

This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
This column is repeated every year at this time with the intent of raising the level of awareness to prevent death or serious illness from heat stroke in athletes and other active people in hot, humid weather.
It is the end of July and we have managed to survive two “heat waves” in NEPA. While it is important to have fun in the sun, please be mindful of how your body reacts to high humidity and heat and take appropriate precautions. Athletes are particularly vulnerable this time of year due to daytime practice sessions. (August 5 & 6, 2024, first day of acclimatization and August 12, 2024, first day of practice for fall sports according to PIAA). Visit www.piaa.org for more information. Keep in mind, you don’t have to be running a marathon or playing football in full uniform to suffer from heat stroke.
Heat stroke, one of the most serious heat-related illnesses, is the result of long term exposure to the sun to the point which a person cannot sweat enough to lower the body temperature. The elderly and infants are most susceptible and it can be fatal if not managed properly and immediately. Believe it or not, the exact cause of heatstroke is unclear. Prevention is the best treatment because it can strike suddenly and without warning. It can also occur in non athletes at outdoor concerts, outdoor carnivals, or backyard activities.
Some “old school” folks think that wearing extra clothing and “breaking a good sweat” is an optimal goal for exercise. However, it may be potentially very dangerous in hot and humid conditions. When exercising in hot weather, the body is under additional stress. As the activity and the hot air increases your core temperature your body will to deliver more blood to your skin to cool it down. In doing so, your heart rate is increased and less blood is available for your muscles, which leads to cramping and other more serious problems. In humid conditions, problems are magnified as sweat cannot be evaporated from the skin to assist in cooling the body.
The American Academy of Pediatrics and The American College of Sports Medicine has the following recommendations which are appropriate for both the competitive athlete and weekend warrior:

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
The 27th Steamtown Marathon is three months away and, despite the warm weather, many local runners are deep into training. With serious heat waves of summer, any prolonged endurance activity in minimal to moderate heat can be dangerous if not prepared. Adequate hydration is critically important, not only to those training for a marathon but also for other outdoor endurance activities such as cycling, hiking, long distance power walking, etc
Next to oxygen, water is the nutrient most needed for life. A person can live without food for a month, but most can survive only three to four days without water. Even though proper hydration is essential for health, water gets overlooked as one of the six basic nutrients. Dehydration occurs when the amount of water taken into the body is less than the amount that is being lost. Dehydration can happen very rapidly (i.e. in less than eight hours); the consequences can be life threatening and the symptoms can be alarmingly swift.
In the body, water is needed to regulate body temperature, carry nutrients, remove toxins and waste materials, and provide the medium in which all cellular chemical reactions take place. Fluid balance is vital for body functions. A significant decrease in the total amount of body fluids leads to dehydration. Fluids can be lost through the urine, skin, or lungs. Along with fluids, essential electrolytes, such as sodium and potassium, are also perilously depleted in a dehydrated individual.
The risk of dehydration is not limited to endurance athletes and outdoor enthusiasts. Dehydration is the most common fluid and electrolyte disorder of frail elders, both in long term care facilities and in the community! Elders aged 85 to 99 years are six times more likely to be hospitalized for dehydration than those aged 65 to 69 years.
Is water adequate to prevent dehydration? Will a sports drink improve my performance? While some answers to these questions apply generally to all, others vary according to the temperature, humidity, length of time and intensity of the activity and condition of the athlete.
Proper hydration is essential for the comfort and safety of the recreational and serious athlete. Hydration is critical to maintain cardiovascular function, body temperature and muscle performance. As temperature, humidity, intensity, and duration of exercise increase, so too does the importance of proper hydration. Excessive sweating can lead to a loss of blood volume which requires the heart to work much harder to circulate you blood through your body.
Dehydration is a major cause of fatigue, loss of coordination, and muscle cramping leading to poor performance. Prehydration, (drinking before exercise) is the first step in preventing dehydration. Marathon runners, other long-distance runners, and cyclists often prehydrate1-2 days before a big event. Rehydration, (drinking during or after exercise) is the second step in preventing dehydration. While athletes may be more vulnerable to dehydration, all persons engaging in exercise would benefit from increased performance, delayed muscle fatigue and pain by maintaining adequate hydration. Proper prehydration would include drinking 12-16 ounces of water 1-2 hours before exercise. Athletes with other health issues should consult their family physician before engaging in long distance endurance sports.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Ageism is prejudice or discrimination on the grounds of a person’s age…
While I hesitate to discuss politics, as an aging physical therapist, I feel that it is incumbent upon me to speak out against ageism, especially with so much attention being paid to the age of the candidates in the upcoming US presidential election. Interestingly enough, age seems to be of more concern for President Biden (age 81), than his opponent, former President Trump (age 78), even though there is only 4 years between them. By the way, “Corporate Sages,” Warren Buffett, CEO of Berkshire Hathaway is 93 years old and Rupert Murdock, CEO of News Corp is 86 years old and their stock holders seem very satisfied! Two local examples of aging with an “A Game” are my 92 year old mentor, Dr. Gino Mori, founder of Delta Medix, who took college classes for enrichment until the age of 90 and Fr. Bernard Mcllhenny, SJ, retired dean of admissions at the University of Scranton, who plays golf (competitively) at least once a week at the age of 98.
It is low hanging fruit to list all the problems associated with age; muscle and bone loss, balance deficits, delayed mental processing, and memory loss to name a few. However, the purpose of this column is to present the positive qualities of the “golden years!”
There are no shortcuts for the assimilation and accumulation of knowledge and wisdom that one acquires over a lifetime and it cannot be taught…only experienced! Not only do older adults know what they know, more importantly, they know what they DON’T know! Moreover, they know how to use this knowledge efficiently and effectively. This is referred to as “crystallized intelligence” and it keeps improving with age…even at 65-75 and more.
While the term “Grumpy Old Men/Women” makes for good TV, the reality is that most of us get more agreeable, likable and consistent with age. Older people are less volatile, control their emotions and tend to focus more on the important things in life.
With age, people tend to be less egocentric and more in tune with the feelings and emotions of others. Using this acquired insight, one can foster a more cooperative and productive solution to problems with friends, family and coworkers.
Quality over quantity with age! Studies show that women over 40 and much older have improved sexual satisfaction when compared to their youth. Moreover, women over 80 were more satisfied with sex than those between 55 and 75! Go figure!
Whether you like it or not, there is a good chance that you will become a “morning person” with age. As sleeping patterns change, including sleep interruptions, we tend to go to bed earlier and rise and shine with the sun. The good news is that you can start your day early to “suck the marrow” out of the day.
Most migraine sufferers report little to no headaches after age 70. And, for older adults who experience headaches, they tend to be less painful and debilitating.
Studies show that early retirement may not be good for your health. The Longevity Project that people who continue to be productive, have purpose, and enjoy their work, live the longest. So maybe, Biden and Trump want the POTUS job in order to stay healthy!
While older adults may fear falling and breaking a bone, they don’t have the same fears and concerns that distract many younger people. With age, self-esteem and confidence improves and with wealth, education, good health and a sense of purpose, these qualities increase exponentially. According to the American Psychological Association, while more young people report high stress levels, older Americans report less. And, even when encountering a stressful situation, older people have learned coping methods to manage it better than younger people.
We can waste our time debating the potential problems with an aging POTUS, however, we must decide between two candidates that will be octogenarians while in office. With that in mind, we must focus on the potential for solid, honest, dedicated, effective and productive leadership to guide us through the next four years. Research has shown that the workforce is aging worldwide and older workers are a critical component to overall productivity in an age of worker shortages. A thorough assessment of the literature related to the productivity of an aging workforce shows that older workers are at least as productive and in some cases (that does not require heavy labor), are more productive than their younger coworkers. In great part, this is attributed to the aforementioned positive aspects of aging such as “crystallized intelligence”. In view of this, ageism has no place in the workplace because older workers can and do keep up.
SOURCES: National Institutes of Health; Mayo Clinic, WebMD

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
JUNE IS GREAT OUTDOORS MONTH! AS WE KICK OFF SUMMER AND CELEBRATE THE FOUR OF JULY, MAKE TIME TO GET THE HECK OUTSIDE! Research shows that spending time outdoors has many positive effects on your health. While there are many year-round activity options, in Northeastern Pennsylvania our short-lived summer is the inspiration to “suck the marrow out of a sunny day!” Summer in NEPA is enjoyed in many ways such as walking, running, hiking, biking, horseback riding, boating, kayaking, and swimming. Studies show that even less vigorous activities such as fishing, picnicking camping, barbequing, or reading a good book on the porch are healthier than being indoors.
It is reported that Americans spend 90% of their lives indoors and that number increases with age. Worse yet, for some, venturing outdoors is considered risky behavior with fear of the sun, ticks, wind, mosquitoes, and other creatures of God. Well, the truth of the matter is the risk of being one with nature is far less than the ill effects of a life stuck indoors. Please consider the following benefits of spending time outdoors.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
I have been advising my patients to exercise, keep active, and walk as long as they can in order to stay mobile and healthy. However, seniors often tell me activities that require prolonged walking is limited by ankle pain from arthritis. They often ask, “What is arthritis of the ankle?” How does it happen? What can I do about it?
Your family physician will examine your ankle to determine if you have arthritis. In more advanced cases you may be referred to a specialist such as a podiatrist, orthopaedic surgeon or rheumatologist for further examination and treatment. X-rays will show if the joint space between the bones in the ankle is getting narrow from wear and tear arthritis. If rheumatoid arthritis is suspected, blood tests and an MRI may be ordered. The diagnosis will determine if you problem if minor, moderate or severe.
In the early stages your treatment will be a conservative, nonsurgical approach, which may include; anti-inflammatory medication, orthopedic physical therapy, exercise, activity modifications, supplements, bracing, etc. You and your family physician, podiatrist, orthopedic surgeon or rheumatologist will decide which choices are best.
When conservative measures no longer succeed in controlling pain and deformity, improving strength and function then more aggressive treatment may be necessary.
SOURCES: Rothman Institute, Philadelphia, PA and American Academy of Orthopaedic Surgeons
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Human beings were designed to move…walk, run, climb, lift, hunt, and gather. Contemporary man has suffered greatly from a technologically driven inactive and sedentary lifestyle. Inactivity is associated with many health problems; obesity, adult-onset diabetes, high blood pressure to name a few. The problems associated with lack of movement are many:
The more you move your body, the more you colon moves! A regular and consistent exercise and activity regime, results in a more consistent bowel schedule, especially with age. Healthy muscle tone in your abdominal muscles and diaphragm is also the key to moving waste through your digestive tract.
Osteoarthritis, rheumatoid arthritis and many inflammatory or auto-immune diseases can cause achy and stiff joints. However, even healthy joints can also stiffen when you don’t use them enough. Put them to work so they don't get tight and cause pain.
All muscles get weak from lack of use, including the muscles that help your lungs expand and contract as you breathe if you don’t work them out regularly. The less exercise or activity you do, the more you experience shortness of breath, even during easy daily tasks.
Physical problems are not the only complication of inactivity. A lack of movement can also increase feelings of anxiety and depression. Aerobic exercises like walking, biking, swimming, or running, have been proven to stimulate endorphins to boost and steady your mood, and even improve your self-esteem.
Many studies have found that regular movement improves energy. Exercise helps deliver oxygen and nutrients to your tissues. When you sit or are inactive, tissues are not getting the same amount of fuel they need to keep you going.
Movement stimulates your metabolism. Hyperactive people burn more calories…just by fidgeting! Even if you are not hyperactive, the more active you are, the more calories you burn each time you move.
One of the first recommendations sleep doctors make to their patients suffering from insomnia is exercise. When you keep a regular exercise routine, you fall asleep faster, and you sleep deeper once you drift off.
Regular exercise tells your body to make more chemicals called growth factors. They boost blood vessel production in your brain. The more blood that gets to your brain, the better you can think, remember, and make decisions.
Spending most of your time sitting raises your risk of heart disease, in great part due to the fact that partly you’re more likely to have high blood pressure. This is a big risk factor for heart issues like coronary artery disease and heart attack.
When physical activity is a regular part of your life, your body has an easier time keeping your blood glucose under control. Exercise can stabilize blood sugar levels and keep you out of the type 2 diabetes danger zone.
When your core muscles are weak from lack of use, they can’t support your back the way they should. This makes it much easier to tweak your back muscles during everyday movements like standing or reaching. Pilates, yoga, and other exercises that use stretching are good for building a stronger back. Schedule an appointment with a good orthopedic and sports PT.
Logically, one might think that you’d be hungry more often if you exercised more, but the opposite is usually true. Aerobic exercise like biking, swimming, walking, and running can actually decrease your appetite because it changes the levels of certain “hunger hormones” in your body.
Studies show the more moderate activity you get, the lower your chance of catching a cold or other germs. When you make exercise a habit, your immune system gets stronger.
If your skin looks duller than usual, a lack of movement may be to blame. Some studies show that moderate exercise boosts your circulation and your immune system, which helps your skin keep that youthful glow.
SOURCE: WebMD

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Most of us are all too familiar with someone in our family or workplace that can be described as a hyperactive or high energy person. I am sure members of my family or coworkers in my office are thinking that this statement is a self-description. Consequently, based on doctor’s advice, it is best to limit me to one cup of coffee or pay the price when I become a hyperactive taskmaster. Now, after further research on this topic, I have concluded that it may be that I may be hyperactive by nature, regardless of my caffeine intake. While many of you may find the following facts hard to believe, and the effects of it may vary for everyone, the facts are still the facts.
Approximately 80% of the world's population consumes caffeine on a daily basis. While research is constantly being done on health benefits and side-effects of it, great controversy and misconception persists. The purpose of this column will be to discuss the “current wisdom” and present the truth about it.
Caffeine is completely absorbed within 30 to 45 minutes of ingestion and its effects linger for about three hours. Eventually it is excreted and there is no accumulation in the body. It has been shown to affect mood, stamina, the blood vessels in the brain, as well as stomach and intestinal activity. However, for most people, when used in moderation (200 to 300mg or 2-3 cups), caffeine use is perfectly safe and may offer some health benefits.
Caffeine is a natural substance found in certain leaves, seeds, and fruits of over 60 plants worldwide. In our culture, the most common sources in our diet are coffee, tea leaves, cocoa beans, cola, and energy drinks. It can also be produced synthetically and added to food, beverages, supplements, and medications. Consumption of 130 to 300 mg of it per day is considered minimal to moderate. Amounts exceeding 500 mg are moderate to heavy and more than 1000 mg/day is excessive. The average daily consumption among Americans is about 280 mg/day and 20% to 30% consume more than 600 mg/day. It's contents in some of the more popular forms are:
Caffeine can be habit-forming, but it is not addictive. The American Journal of Drug and Alcohol Abuse states that it is a mild stimulant but does not have the qualities of addictive stimulants like cocaine and amphetamines. However, sudden abstinence from caffeine can produce mild withdrawal symptoms such as headache, restlessness, and irritability. Therefore, it is recommended to slowly wean off it over a week or two to lessen these symptoms.
The need to eliminate caffeine from your diet is not supported in the literature. In fact, studies show that moderate use can enhance your mood and improve focus and alertness. The American Dietetic Association suggests limiting intake to 200mg to 300mg (2- 3 cups of coffee) per day.
While caffeine is a diuretic, its effects are very mild. However, like all diuretics, it will cause you to urinate more often and therefore, lose fluids. The more fluids you lose, the greater the chance for dehydration, especially if you are at risk due to health issues. Also, long distance runners and athletes performing in conditions of extreme heat must use caution. Minimal to moderate intake with generous use of water and sports drinks should suffice.
A study conducted at the University of Madrid of more than 126,000 people found that women who drank 2-3 cups of caffeinated coffee per day had a 25% lower risk of heart disease. Also, a 33-yearlong study of more than 1,000 participants at Johns Hopkins University found that coffee had no significant effect on the risk of hypertension. Moderation seemed to be the key component in these studies. Interestingly, caffeinated colas did increase the risk of hypertension; however, it was believed to be due to the high amounts of sugars and other ingredients in the drink.
However, for many reasons, physicians tell their cardiac patients, especially those with high blood pressure or abnormal heart rhythms, to avoid it. This matter should be discussed in more detail with your physician before using caffeine. Tea, especially black and green, contains a much smaller amount of caffeine than coffee, is often recommended for the health benefits of antioxidants.
While studies show that moderate amounts (40 – 200mg) in children does not make them hyperactive, others demonstrate that a 12 oz can of cola with only 35 mg of caffeine makes them bounce off the walls. It has been concluded that it is the sugar and other ingredients in the soda that makes them hyperactive. In fact, some studies show that small amounts of it can work like Ritalin and improves focus in children with attention disorders.
Caffeine has been shown to increase calcium excretion when taken in large amounts. Unless a child drinks caffeinated coffee in place of milk, there is no scientific evidence that bone loss will occur. When it is used in moderation, no evidence of bone loss exists.
There is no scientific evidence to support the claim that caffeine causes fibrocystic breast disease or breast cancer. Confusion may lie with the fact that it is associated with increased breast pain during monthly hormonal changes. If so, women are well advised to reduce the intake of caffeine during this time.
Source: www.LifeScript.com

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
June is migraine and headache awareness month! According to the World Health Organization about half of the world’s adult population has had a headache at least once in the past year. Prolonged use of electronic devices has greatly contributed to this problem. For many people, these headaches are infrequent and do not often affect daily life. But what about when your headache occurs frequently or is so severe it prevents you from going about your day to day activities? Some types of headaches are more easily treated and managed than others.
There are two types of headaches: primary and secondary. Primary headaches occur without an underlying disease and include migraines and tension-type headaches. Secondary headaches can be associated with serious disease, requiring emergency care, or can be referred from other structures of the body such as the cervical spine (neck).
Headaches symptoms that may constitute a medical emergency are: vomiting, seizures, fever, muscle pain, night sweat, weight loss, and neurologic symptoms such as blurred vision. If you are experiencing any of these symptoms, if your headache worsens, or your symptoms change it is recommended that you seek medical attention. Any headache that is unusual for you and does not resolve itself in a reasonable time should be brought to your primary care physician’s attention.
Migraines: Migraines are a primary form of headache that typically lasts from four to seventy two hours, can range from moderate to severe pain, and typically are located on only one side of the head. Often they can be accompanied by an aura, nausea or vomiting, sensitivity to sound, or light sensitivity. Migraines can be aggravated by routine physical activity such as going up stairs. This type of headache is thought to occur in the central nervous system.
Tension-type: Tension-type headaches are the most common primary headache disorder and can last anywhere from thirty minutes to seven days. These can often have a pressing or tightening quality that occurs on both sides of the head. Typically, there is no nausea, vomiting, or aggravation with physical activity, however, light or sound sensitivity can occur. This type of headache is thought to occur in the central nervous system but can have a hereditary component and is usually associated with muscle tender points. Tension – type headaches can be treated with relaxation techniques such as Progressive Muscle Relaxation (PMR), medications, and physical therapy.
The most common secondary headache that is not related to a serious medical condition is a cervicogenic headache (originating from the neck).
Cervicogenic Headache: The length of time a cervicogenic headache can last varies. Here the pain is on one side and usually starts in the neck. This type of headache is aggravated or preceded by head postures or movements of the neck. Due to the nerves of the neck and face sharing common connections, pain signals sent from one region can lead to discomfort in the other. Physical therapy can be an effective treatment to help relieve symptoms. For example: posture, exercise, ergonomics, massage, manual techniques, traction, trigger point, and acupressure.
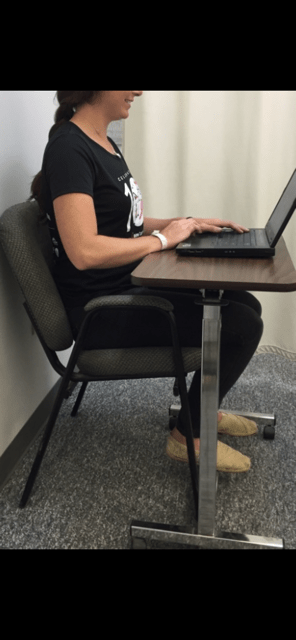
A cervicogenic headache can be caused by an accident or trauma or can stem from neck movement or sustained postures. Sustained postures could mean sitting in front of a computer at work or looking down at your phone. Changing these postures throughout the day could help reduce symptoms. Changing postures could mean bringing your phone closer to you using pillows or another supportive surface when reading or checking social media. If you are someone who works at a desk, it could involve taking breaks or getting a standing desk. However your life requires you to move, there are some simple and effective exercises you can perform throughout the day to help cervicogenic headache symptoms.
Progressive Muscle Relaxation: PMR is an effective method for reducing tension throughout the body. With this method you first tense a muscle group, such as at the neck or shoulder, and then relax the muscles noting the difference between the two. This helps reduce both stress and tension. For more information or to learn how to do PMR, refer to podcast at: https://www.psychologies.co.uk/try-progressive-muscle-relaxation
Manage your stress level: While stressors vary from person to person, one method for managing stress is with exercise. Any form of exercise can help reduce stress, but a cost free method is aerobic exercise such as walking or running. A less time consuming method could be to perform deep breathing exercises throughout the day.
Heat or cold: When feeling sore or stiff, applying a hot or cold pack or taking a hot shower can help ease a tension headache.
Posture: Some tips for posture are to make sure your head is over your shoulders rather than sitting forward and making sure you are sitting or standing up straight with your shoulders back.
Over the counter medications: Talk to your doctor or pharmacist for additional information.
Posture: See tips listed under tension headaches.
Ergonomics: If your job or hobbies require you to sit for extended periods it may be beneficial to change positions throughout the day or consider getting a standing desk. Also, limit time on electronic devices. When sitting make sure the monitor is at eye level, your legs are able to fit under your desk, and you are close to the keyboard and monitor. If you are working with a laptop or phone, avoid putting it on your lap. Instead, bring your laptop closer to you by putting pillows on your lap or using an ergonomic desktop. See photo below.
Exercise: Some exercises to help relieve symptoms are chin tucks, shoulder blade pinches, and back extension. These exercises can be performed multiple times throughout the day in sitting or standing.
Physical Therapy: Physical therapy may include massage, manual techniques, stretching, traction/ decompression and exercise. A physical therapist can assess your posture and provide strategies specific to you.
Over the counter medications: While medication may not cure cervicogenic headaches, they may help relieve pain. Talk to your doctor or pharmacist for additional information.
Visit your doctor regularly and listen to your body.

Dr. Chua is a neurologist and headache specialist at Geisinger Health System in Northeast Pennsylvania. In addition to caring for people with headache and facial pain disorders, Dr. Chua also serves as: Director of Headache Medicine at Geisinger, Clinical Director of Neurology at Geisinger Wyoming Valley, faculty at Thomas Jefferson University’s Advanced Headache Diagnosis and Management Post-Graduate Certificate Program, and Treasurer and Executive Board Member of the Association of Migraine Disorders. In her spare time, she enjoys going on adventures with her husband and toddler, learning new skills (she is now certified in battlefield acupuncture), and buying great books she will never have time to read!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!