Allergies affect 30 % of adults and 40% of children in the United States. Avoiding the outdoors is often not an option…especially if you enjoy outdoor activities and sports. Not long ago, it was unthinkable that an athlete with serious allergies could compete at a high level, such as the Olympics. Now, in great part due to advanced research, medications and proper management, an Olympic gold medal for those suffering from allergies is a reality. Recently, the National Institute of Allergy and Infectious Disease at the National Institutes of Health have published research on this topic to provide a better understanding and make recommendations.
The most common allergic reactions which athletes suffer from are sneezing, itchy and watery eyes, runny nose and coughing. Moreover, 67% of those with these symptoms also suffer from asthma. The athlete in NEPA is particularly vulnerable when the pollen count is high during spring and fall for several reasons. One, after being indoors all winter, one might develop a heightened sensitivity to allergens. Also, increased rapid and deep breathing during exercise makes athletes more susceptible to significant symptoms when exposed to allergens such as tree, grass and weed pollens.
As mentioned last week, allergy skin testing can be performed to determine the allergens to which you are susceptible. Once determined, allergy shots are effective in building up tolerance to these allergens. If appropriate, you may be able to use allergy drops, administered under the tongue and conveniently used at home.
Asthma suffers should use their inhaler BEFORE symptoms occur. A recent study found that pretreatment using a short-acting bronchodilator inhaler within 15 minutes before exercise is very effective in preventing asthma symptoms for more than four hours. It is important to keep a bronchodilator available. If you fail to benefit from this, see your physician for other methods to control your exercise-induced symptoms.
Whether you have allergic respiratory problems from rhinitis or asthma, you many benefit from conditioning your airways with a 10 to 15 minute warm-up before and cool-down after the activity. This may serve to gradually prepare your lungs for an increased demand.
In addition to preventing dehydration on hot and humid days, constant hydration is very important for the athlete with allergies to prevent dry airways in athletes.
Know the signs and symptoms of asthma (coughing, wheezing, tightness in chest, shortness of breath).
Some schools have a file on each student athlete with a allergic or asthmatic problem which requires medication. The file includes information such as medical doctor release and instruction, emergency contacts and medications. Students must have their medications on hand before they can enter the field. The National Athletic Trainers Association recommends using a peak flow meter to monitor at risk players and can determine when a player can return to the field.
If possible, find an alternate practice facility with climate control for athletes at risk. Plan practices for these athletes when the pollen count is low. Check the newspaper or internet for pollen counts in your area. Training by the water, (ocean) where there is a breeze and less pollen is helpful.
Shower and change clothing immediately after being outdoors
During a flare up, do less aerobic exercise to limit stress on respiratory system. Try strength training indoors instead.
When pollen count is high, keep windows shut at home and in your car….use air-conditioning.
Keep pets out of your bedroom…especially when sleeping
Dry clothing in dryer…do not hang on clothesline outdoors
Sources: American College of Allergy, Asthma, and Immunology. National Athletic Trainers Association.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

I am sure that many of you feel as I do…it is hard to believe that I am living in the year 2025! Moreover, I hope you share my sentiments that each year, despite the trials and challenges of each month, week, day, and minute, is a gift, not to be taken for granted and 2025 is no different. And that is why we resolve at this time each year to make a concerted effort to improve ourselves; mentally, physically and spiritually, so that we may live a longer and healthier life, to spend more time with the friends and family we love.
Not surprisingly, getting physically fit and losing weight are the top resolutions to begin each New Year, even 2025. According to the University of Pittsburgh Medical Center, 10 million Americans choose to join one of the 45,000 health clubs and hope to get fit and healthy for life. Unfortunately, if starting an exercise program is the hard part, than sticking to it is the hardest part.
Once the initial excitement and enthusiasm wears off after the 2025 new year, so does the discipline and determination necessary to overcome the many distractions in our lives to make exercise a priority for life. Diane Klein, PhD polled long-term exercisers (those exercising at least 3 times per week for more than 13 years) what motivated them to “stick with the program.” The answers are in order of importance. Please note that “appearance” was NOT at the top of the list.
Source: WebMD, Mayo Clinic
Visit your doctor regularly and listen to your body.
Keep moving, eat healthy foods, exercise regularly, and live long and well!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Osteochondritis dissecans, also called OCD, is the most common cause of a loose body or fragment in the knee and is usually found in young males between the ages of ten and twenty. While this word sounds like a mouth full, breaking down its Latin derivation to its simplest terms makes it understandable: “osteo” means bone, “chondro” means cartilage, “itis” means inflammation, and “dissecans” means dissect or separate. In OCD, a flap of cartilage with a thin layer of bone separates from the end of the bone. As the flap floats loosely in the joint, it becomes inflamed, painful and disrupts the normal function of the joint.
Typically, OCD is found in the knee joint of active young men who participate in sports which involve jumping or full contact. Although less common, it is also found in other joints such as the elbow.
Often, the exact cause of OCD is unknown. For a variety of reasons, blood flow to the small segment at the end of the bone lessens and the weak tissue breaks away and becomes a source of pain in the joint. Long term, OCD can increase the risk of osteoarthritis in the involved joint.
To properly diagnose OCD a physician will consider onset, related activities, symptoms, medical history, and examine the joint involved for pain, tenderness, loss of strength and limited range of motion. Often, a referral to a specialist such as an orthopedic surgeon for further examination is necessary. Special tests specifically detect a defect in the bone or cartilage of the joint such as:
Radiograph (X-ray) may be performed to assess the bones.
Magnetic Resonance Imaging (MRI) may be performed to assess bones and other soft tissues such as cartilage, ligaments, muscles and tendons.
The primary goal of treatment for OCD is to relieve pain, control swelling, and restore the complete function (strength and range of motion) of the joint. The age of the patient and severity of the injury determine the treatment methods. For example, medications assist with pain and inflammation reduction.
Young patients who are still growing have a good chance of healing with conservative treatment. Rest and physical therapy are the conservative treatments of choice. Rest entails avoiding any activity that compresses the joint such as jumping, running, twisting, squatting, etc. In some cases, using a splint, brace and crutches to protect the joint and eliminate full weight bearing, may be necessary for a few weeks. Physical therapy, either as a conservative or post operative treatment, involves restoring the range of motion with stretching exercises and improving the strength and stability of the joint through strengthening exercises. Modalities for pain and swelling such as heat, cold, electrical stimulation, ultrasound, compression devices assist with treatment depending on the age of the patient and severity of the problem.
Conservative treatment can often require 3 to 6 months to be effective. However, if it fails, arthroscopic surgery stimulates healing or reattaches the loose fragment of cartilage and bone. In some cases if the defect is small, surgery involves filling in the defect with small bundles of cartilage. In other cases, the fragment is reattached directly to the defect using a small screw or bioabsorbable device. More recently, surgeons are using the bone marrow of the patient to repair the deficit by stimulating the growth of new tissue (bone marrow stimulation).
In other cases, a plug of healthy tissue from the non-weight bearing surface of a patient's knee relocated to the defect to stimulate healing (osteochondral autograft transplantation OATS). While there are many surgical options for OCD, an orthopedic surgeon will help the patient decide the most appropriate procedure based on age, size of defect, and other factors.
While prevention is not always possible, some measures can be taken to limit risk. For example, if a child playing sports has a father and older brother who had OCD, then it would be wise to consider the following: Avoid or make modifications for sports requiring constant jumping. Cross-train for a sport to avoid daily trauma (run one day and bike the next). Also, do not play the sport all year round (basketball in the fall/winter and baseball in the spring/summer). Seek the advice from an orthopedic or sports physical therapist to learn proper strength and conditioning techniques. Learn proper biomechanics of lifting, throwing, squatting, running, jumping and landing.
Sources: Mayo Clinic

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Congratulations to more than 1,000 courageous runners who finished the 27th Annual Steamtown Marathon today. Most, if not all of you are waking up this morning with a little less jump in your step than you had yesterday.
As active people by nature, many of you will resist the logic of rest, despite the pain and stiffness in your muscles and joints. Therefore, I would like to offer some words of wisdom, based on science, to encourage you to adequately rest and allow your body to recover.
With adequate rest and recovery, an elite runner can quickly regain full form in 3-4 weeks, while an average runner may require 4-6 weeks. Meb Keflezighi, an elite American runner and winner of the 2014 Boston Marathon, is an excellent example of the merits of rest and recovery. However, he discovered it by accident…following the 2012 New York City Marathon, Meb developed a foot infection which required three weeks rest. With the Olympic Trials just 70 days away, Meb quickly regained his pre-injury fitness level to win the 2012 US Olympic Marathon Trials and join the US Olympic Team in London. It may be that his injury was fortuitous and allowed him adequate recovery time, (that he might not have otherwise allowed), preparing him for intensive training leading up to the trials.
The Effects of Running 26.2 Miles on the Body:
(RunNow.com - Jim Peskett)
One of the most obvious effects of running a marathon is significant muscle and joint pain and stiffness. It will set in after you sit for a while and attempt to get up and move around. For most, it will be more pronounced the day after the marathon, as you get out of bed and limp to the bathroom. Studies show that the leg muscles, (especially the calf muscles) display significant inflammation and necrosis (dead tissue) in the fibers of the muscle. In other words, the trauma to the muscles is so severe that tissue damage causes muscle cells to die. Consequently, studies found that muscle strength, power and endurance is compromised and required significant time to recover… sometimes as long as 4-6 weeks!
Additionally, many runners report severe bone and joint pain following the race. Some studies report findings of microfractures or bone bruising from the repeated and prolonged pounding of the marathon. It is purported that the stress on the joints may be related to: weight and body type, running shoes, running style and mechanics. While not dangerous, again, it is important to respect the stress placed on the body and allow adequate healing…LISTEN TO YOUR BODY!
Creatine kinase is an enzyme found in the brain, skeletal muscles and heart. It is found in elevated levels in the presence of cellular damage to these tissues, for example, following a heart attack. Similarly, significantly elevated creatine kinase levels are found in the blood of runners up to 4 days post marathon, demonstrating extensive tissue damage at the cellular level. It is important to note, that these enzyme markers are present, even if a runner does not experience muscle soreness. So, adequate rest for healing and recovery is required, regardless of soreness.
It is not a coincidence that the runners are more likely to contract colds and flu after intensive training or running 26.2 miles. The immune system is severely compromised after a marathon and without adequate recovery; a runner can become ill and ultimately lose more training time or will underperform.
FALSE: As stated above, enzyme levels that indicate cellular damage to the tissues are present in the post-marathon runner, even in those without significant pain.
FALSE: In addition to rest, drink, drink, drink - 24 ounces of water for every 2 pounds you lose after the marathon. This is based on pre and post exercise weight. You just burned 2,600 calories so avoid diet soft drinks. You need the glucose (sugar) boost. Also, don’t drink alcohol and use minimal amounts of caffeine (the equivalent of 1-2 cups of coffee). First, drink plenty of water and sports drinks (Gatorade) to prevent a diuretic like caffeine from messing up your fluid balance.
FALSE: Studies clearly show that the VO2 Max, (the best measurement of a runner’s endurance and fitness), is unchanged after one week of inactivity. And, after two weeks, the loss is less than 6% and can be regained quickly. Moreover, it is important to remember, without adequate rest and recovery, performance is comprised, not by the loss of VO2 Max, but by muscle-skeletal tissue damage, which renders the leg muscles of the runner weaker. Remember Meb Keflezighi!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Like many of you, I have always enjoyed the outdoors...walking, running, biking, hiking etc. However, recently, I have been more concerned about being safe, (getting older and more cautious, distracted drivers) when doing these activities on the side of the road.
Almost 15 percent of all motor vehicle injuries to people happened to those not in cars but while walking, running or hiking, so one needs to be safe. In fact, over 4,000 walkers or runners were fatally hit by a motor vehicle according to the Centers for Disease Control (CDC). These statistics continue to increase as the number of distractions to drivers increases (phone calls, texts, etc). Consequently, walkers, runners and cyclists must be more aware than ever to prevent injury from motor vehicles and stay safe.
Source: http://www.runnersworld.com
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

“When is it safe for my child to start weight training?” This is a very common question asked by parents of young athletes who are looking for advice regarding their children’s participation in weight training. This month, for example, I received three such inquiries. While some who are eager to get a “competitive edge” may not be satisfied with the answer, these recommendations are grounded in the scientific literature and medical specialist with the hope to prevent injury and dispel fear and fallacy.
Weight training, weight lifting or resistive training all describes the use of a resistive force on a muscle to improve strength. While much attention has been given to the benefits of weight training in adults, much less has been written about its application in children.
According to the Journal of Pediatric Orthopedics, children less than 12 years old are considered prepubescent or before puberty. Teenagers who are between 12 and 19 are considered to be adolescents. Studies consistently demonstrate that strength gains are much more significant in adolescents than in preadolescents. It is important to note that these strength gains are not only from the enlargement of muscle fibers (hypertrophy), but also from the improvement in the coordination and efficiency in muscle contraction and the recruitment of motor units and fibers within the muscle.
Preadolescents lack the hormones necessary to develop masculine characteristics. Adolescents begin to produce the hormones of testosterone and androsterone to develop secondary sexual characteristics such as pubic hair and enlarged genitalia. In view of this, age 13-14 is the optimal age to safely begin and benefit from a well-designed weight training program.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

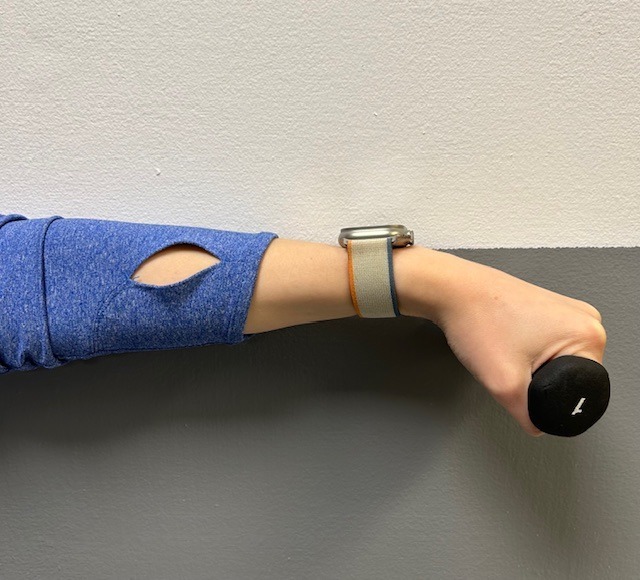
Tennis elbow, also called lateral epicondylitis, is an inflammation of the lateral (outside) bony protuberance at the elbow. It is at this protuberance that the tendon of the long muscles of the hand, wrist and forearm attach to the bone. As the muscles repeatedly and forcefully contract, they pull on the bone, causing inflammation. The trauma is irritating when working the muscles in an awkward position with poor leverage like hitting a backhand in tennis.
It is not unusual for a patient to come to my office with severe pain on the outside of their elbow. Especially, after intensifying their tennis workouts or changing the racquet string tension. Others come to me with pain on the inside of the elbow (“golfer’s elbow”) from wrist action that advanced golfer’s use at impact. However, this problem is not only for tennis players and golfers. Laborers working with wrenches or screwdrivers with an awkward or extended arm can also develop tennis elbow. Others who are vulnerable are: those working for hours at a computer using a mouse as well as those working hard maintaining their lawns and gardens.
In a more chronic problem, lateral elbow pain may arise by a degenerative condition of the tendon fibers on the bony prominence at the lateral elbow. Sporadic scar tissue forms from a poor attempt by the body to overcompensate and heal without eliminating the cause.
While symptoms may vary, pain on the outside of the elbow is almost universal. Patients also report severe burning pain that begins slowly and worsens over time when lifting, gripping or using fingers repetitively. In more severe cases, pain can radiate down the forearm.
Conservative treatment is almost always the first option and is successful in 85-90 percent of patients with tennis elbow. Your physician may prescribe anti-inflammatory medication (over the counter or prescribed). Physical/Occupational therapy, rest, ice, and a tennis elbow brace to protect and rest may be advised. Ergonomic changes in equipment, tools, technique and work-station may be necessary. Improvement should occur in 4-6 weeks. If not, a corticosteroid injection may be needed to apply the medication directly to the inflamed area. Physical therapy, range of motion, and stretching exercises may be necessary prior to a gradual return to activity. Deep friction massage can assist healing.

Exercises performed in a particular manner to isometrically hold and eccentrically lengthen the muscle with contraction.
New Conservative Treatment: Platelet-Rich-Plasma (PRP) is a new treatment for the conservative management of degenerated soft tissues that has recently received great media attention. In great part, due to its success in several high profile athletes. According to the Journal of the American Academy of Orthopaedic Surgeons,(JAAOS), platelet-rich plasma (PRP) is autologous (self-donated) blood with an above normal concentration of platelets. Normal blood contains both red and white blood cells, platelets and plasma. Platelets promote the production and revitalization of connective tissue by way of various growth factors on both a chemical and cellular level.
The actual PRP injection requires the patient to donate a small amount of their own blood. The blood is placed into a centrifuge (a machine that spins the blood at a high velocity to separate the different components of blood such as plasma, white and red blood cells), for approximately 15 minutes. Once separated, the physician draws the platelet-rich plasma to be injected directly into the damaged tissue. In theory, the high concentration of platelets, with its inherent ability to stimulate growth and regeneration of connective tissue, will promote and expedite healing.
Surgery for tennis elbow is only considered in patients with severe pain for longer than 6 months without improvement from conservative treatment. One surgical technique involves removing the degenerated portion of the tendon and reattaching the healthy tendon to bone. Recently, arthroscopic surgery developed to perform this technique. However, research does not support the value of one over the other at this point. Physical/occupational therapy is used after surgery. Return to work or athletics may require 4-6 months. More recently, a surgical technique using ultrasound to guide a needle to debride (clean) the area of scar tissue has been developed. If eligible for this procedure, the time required for healing, rehabilitation and return to activity is much shorter.
If you feel you suffer from tennis elbow, ask your family physician which of these treatment options are best for you.
Visit your doctor regularly and listen to your body.
EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy

This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Seasonal allergies affect 30 % of adults and 40% of children in the United States. Avoiding the outdoors is often not an option…especially if you enjoy outdoor activities and sports. Not long ago, it was unthinkable that an athlete with serious seasonal allergies could compete at a high level, such as the Olympics. Now, in great part due to advanced research, medications and proper management, an Olympic gold medal for those suffering from seasonal allergies is a reality. Recently, the National Institute of Allergy and Infectious Disease at the National Institutes of Health have published research on this topic to provide a better understanding and make recommendations.
The most common allergic reactions which athletes suffer from are sneezing, itchy and watery eyes, runny nose and coughing. Moreover, 67% of those with these symptoms also suffer from asthma. The athlete in NEPA is particularly vulnerable when the pollen count is high during spring and fall for several reasons. One, after being indoors all winter, one might develop a heightened sensitivity to allergens. Also, increased rapid and deep breathing during exercise makes athletes more susceptible to significant symptoms when exposed to allergens such as tree, grass and weed pollens.
Allergy skin testing can be performed to determine the allergens to which you are susceptible. Once determined, allergy shots are effective in building up tolerance to these allergens. If appropriate, you may be able to use allergy drops, administered under the tongue and conveniently used at home.
Asthma suffers should use their inhaler BEFORE symptoms occur. A recent study found that pretreatment using a short-acting bronchodilator inhaler within 15 minutes before exercise is very effective in preventing asthma symptoms for more than four hours. It is important to keep a bronchodilator available. If you fail to benefit from this, see your physician for other methods to control your exercise-induced symptoms.
Whether you have allergic respiratory problems from rhinitis or asthma, you many benefit from conditioning your airways with a 10 to 15 minute warm-up before and cool-down after the activity. This may serve to gradually prepare your lungs for an increased demand.
In addition to preventing dehydration on hot and humid days, constant hydration is very important for the athlete with allergies to prevent dry airways in athletes.
Know the signs and symptoms of asthma (coughing, wheezing, tightness in chest, shortness of breath).
Some schools have a file on each student athlete with a allergic or asthmatic problem which requires medication. The file includes information such as medical doctor release and instruction, emergency contacts and medications. Students must have their medications on hand before they can enter the field. The National Athletic Trainers Association recommends using a peak flow meter to monitor at risk players and can determine when a player can return to the field.
If possible, find an alternate practice facility with climate control for athletes at risk. Plan practices for these athletes when the pollen count is low. Check the newspaper or internet for pollen counts in your area. Training by the water, (ocean) where there is a breeze and less pollen is helpful.
Shower and change clothing immediately after being outdoors
During a flare up, do less aerobic exercise to limit stress on respiratory system. Try strength training indoors instead.
When pollen count is high, keep windows shut at home and in your car….use air-conditioning.
Keep pets out of your bedroom…especially when sleeping
Dry clothing in dryer…do not hang on clothesline outdoors
Sources: American College of Allergy, Asthma, and Immunology. National Athletic Trainers Association.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Ice baths have become a new trend or fad in health and fitness, especially among elite athletes and some celebrities. However, it is far from a new treatment modality. In fact, the Ancient Greeks employed cold-water immersion for fever, pain relief, relaxation and socialization. In addition, Hippocrates documented the use of cold for medicinal purposes for its analgesic benefits.
Ice baths, a type of cryotherapy, is also referred to as cold water immersion (CWI) or cold water therapy. This involves immersing your body in ice water for approximately 5-15 minutes from the neck down at 50-59 degrees. The ice baths are commonly used for pain, delayed-onset muscle soreness (DOMS), and inflammation and mood elevation.
In theory, the cold water lowers the temperature of your skin and body by vasoconstriction (narrow) of the blood vessels. When you get out of the cold, water the vasodilatation (widen) of the blood vessels. Immediately, this brings fresh oxygen and nutrient-rich blood back to the tissues to warm the body and in the process, reduce pain, inflammation and promote healing.
If you have the following health conditions, ice baths may not be the best therapeutic modality for you. Before you consider trying an ice bath, consult with your physician to avoid potentially serious problems:
While some studies have shown that subjects report less muscle soreness following CWI when compared to rest, most studies suggest that the reported effects are placebo. Also, reports of improved circulation, reduced inflammation and improved recovery or performance has not been scientifically validated. In view of this, it is recommended that those considering the use of CWI for pain and inflammation management, reduced muscle soreness, and mood elevation, should consult their physician to determine if the potential risks are worth the purported benefits.
SOURCES: nih; health.com; health.clevelandclinic.org; prevention.com

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
During a recent “lunch-and-learn” meeting at our office, several younger staff members were discussing the use of supplements to compliment their fitness routines. One such staff member, Lily Smith, a physical therapy student aid at our clinic from the University of Scranton, is also a serious weight training and fitness enthusiast and shared her experience with creatine supplements with the hope of educating others, especially those preparing to “get fit” in 2024!
A National Health Interview survey found the creatine use among adolescents and young adults to be 34%. It is also very popular in the military with 27% average usage. While athletes and exercise enthusiasts use protein shakes and creatine supplements with hopes to improve size, strength and performance, it appears that most users do not have a full understanding of the risks and benefits. In view of this, today address the use of creatine in strength training and make recommendations based on the literature.
As long as I can remember, young athletes would take or do anything that they believed would improve their speed, strength, agility and athletic edge in order to succeed in sports. Running with weights wrapped around the ankles, drinking raw eggs and whole milk, and consuming copious amounts of beef, pork, and chicken were not unusual. Today, it may not be much different. However, the products do not come from our kitchen cabinet and tremendous misinformation is associated with it. Creatine is one example that was purported to enhance performance as early as the 1970’s but only gained popularity in the 1990’s. 40% of all college athletes and 50% of professional athletes admit to using creatine at some point, despite a lack of scientific evidence to support its effectiveness or safety.
This supplement is a natural substance that turns into creatine phosphate in the body. Creatine phosphate helps produce adenosine triphosphate (ATP), which provides energy for muscles to contract. While the body produces some creatine, it can also be found in foods rich in protein such as meat and fish. Manufacturers claim that creatine use will improve strength, increase lean muscle mass and aide in the recovery from exercise induced fatigue.
While creatine is popular among young people due in part to its availability, very little research has been done in people under 18 years of age. Even in the few studies conducted on adults, the results regarding efficacy are mixed. Some studies show that creatine may improve strength performance due to the recovery cycle of ATP. In theory, the use of creatine is purported to allow one to recover more quickly from exercise. For example, shortly after lifting heavy weights to failure, a quick recovery might allow the weight lifter to lift an additional set of repetitions to increase the duration of intensive training. Therefore, based on this theory, one must work out to complete failure during training to benefit from creatine. However, it is important to remember, there is no evidence that this purported benefit is realized in performance improvement in weight training or endurance sports.
Furthermore, no studies support the notion that it improves performance in endurance sports. Also, research does show that not all users are affected by creatine the same way. Most users fail to find any benefit at all. More concerning to this author is the fact that there are no guidelines for safety or disclosure of side-effects from long term use. Make no mistake, based on the research and current wisdom, CREATINE IS AN UNPROVEN TREATMENT SUPPLEMENT!
If one decides that creatine is a product they would like to use, despite the lack of evidence for its effectiveness, there are recommendations that one should follow for proper use. But there is no consistently established dose. Some studies have found 25 grams daily for 14 days as a “kickstart” dose or “loading” phase followed by 4-5 grams (or 0.1 g/kg of bodyweight) daily for 18 months with few side effects such as: muscle cramps, dehydration, upset stomach, water retention/bloating with weight gain. It is important to remember when establishing a dosage that many weight training supplements already contain creatine and in high doses excess creatine is excreted by the kidneys. It is also recommended that creatine users “wean off” the product when they decide to discontinue use.
Remember, an average adult in the United States receives 1 to 2 grams of creatine each day from a normal, well-balanced diet. Creatine is naturally found in meat, poultry and fish and theoretically, one could increase their creatine intake through dietary changes. Some manufacturers recommend 10 to 30 grams per day with a maintenance dose of 2 to 5 grams per day for athletic performance. Creatine is available in many forms; tablets, capsules and powder. It should be kept in a cool, dry place out of direct sunlight.
Creatine use is not recommended if you are pregnant, breast feeding, have kidney disease or bipolar disorder. There are many reported side effects associated with creatine use such as; water retention, nausea, diarrhea, cramping, muscle pain and high blood pressure. It is recommended that users consume large quantities of water when taking creatine to prevent dehydration. It may be very dangerous to use creatine when dehydration or weight loss is associated with an activity such as wrestling or summer sessions during football.
Furthermore, some studies show that large amounts of carbohydrates may increase the effects of creatine and caffeine may decrease the effects. Users are warned that using creatine with stimulants such as caffeine and guarana (a Brazilian plant extract similar to caffeine found in energy drinks) can lead to serious cardiac problems. The effects of creatine supplements on the many organ systems of the body are unknown. High doses may cause kidney damage. Although no cases have been reported in the literature, it is not known how it may interact with other supplements, over-the-counter medications and prescription drugs.
In conclusion, despite the lack of scientific evidence that creatine is more effective than proper nutrition and effective weight training, it remains a popular, easily available supplement purported to improve strength, endurance and performance in athletes. While relatively safe if taken as directed, it is always wise to consult your physician, especially if you have a history or risk of kidney problems. And, by the way, Lily did not feel that creatine supplements made any significant difference, positively or negatively. She no longer uses it due to the expense, inconvenience and lack of scientific evidence to support its efficacy.
Sources: University of New England; Medicine & Science in Sports & Exercise; NIH and Lily Smith, PT student, University of Scranton, Student PT aide, Mackarey Physicla Therapy
.Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!