Congratulations to more than 1,000 courageous runners who finished the 27th Annual Steamtown Marathon today. Most, if not all of you are waking up this morning with a little less jump in your step than you had yesterday.
As active people by nature, many of you will resist the logic of rest, despite the pain and stiffness in your muscles and joints. Therefore, I would like to offer some words of wisdom, based on science, to encourage you to adequately rest and allow your body to recover.
With adequate rest and recovery, an elite runner can quickly regain full form in 3-4 weeks, while an average runner may require 4-6 weeks. Meb Keflezighi, an elite American runner and winner of the 2014 Boston Marathon, is an excellent example of the merits of rest and recovery. However, he discovered it by accident…following the 2012 New York City Marathon, Meb developed a foot infection which required three weeks rest. With the Olympic Trials just 70 days away, Meb quickly regained his pre-injury fitness level to win the 2012 US Olympic Marathon Trials and join the US Olympic Team in London. It may be that his injury was fortuitous and allowed him adequate recovery time, (that he might not have otherwise allowed), preparing him for intensive training leading up to the trials.
The Effects of Running 26.2 Miles on the Body:
(RunNow.com - Jim Peskett)
One of the most obvious effects of running a marathon is significant muscle and joint pain and stiffness. It will set in after you sit for a while and attempt to get up and move around. For most, it will be more pronounced the day after the marathon, as you get out of bed and limp to the bathroom. Studies show that the leg muscles, (especially the calf muscles) display significant inflammation and necrosis (dead tissue) in the fibers of the muscle. In other words, the trauma to the muscles is so severe that tissue damage causes muscle cells to die. Consequently, studies found that muscle strength, power and endurance is compromised and required significant time to recover… sometimes as long as 4-6 weeks!
Additionally, many runners report severe bone and joint pain following the race. Some studies report findings of microfractures or bone bruising from the repeated and prolonged pounding of the marathon. It is purported that the stress on the joints may be related to: weight and body type, running shoes, running style and mechanics. While not dangerous, again, it is important to respect the stress placed on the body and allow adequate healing…LISTEN TO YOUR BODY!
Creatine kinase is an enzyme found in the brain, skeletal muscles and heart. It is found in elevated levels in the presence of cellular damage to these tissues, for example, following a heart attack. Similarly, significantly elevated creatine kinase levels are found in the blood of runners up to 4 days post marathon, demonstrating extensive tissue damage at the cellular level. It is important to note, that these enzyme markers are present, even if a runner does not experience muscle soreness. So, adequate rest for healing and recovery is required, regardless of soreness.
It is not a coincidence that the runners are more likely to contract colds and flu after intensive training or running 26.2 miles. The immune system is severely compromised after a marathon and without adequate recovery; a runner can become ill and ultimately lose more training time or will underperform.
FALSE: As stated above, enzyme levels that indicate cellular damage to the tissues are present in the post-marathon runner, even in those without significant pain.
FALSE: In addition to rest, drink, drink, drink - 24 ounces of water for every 2 pounds you lose after the marathon. This is based on pre and post exercise weight. You just burned 2,600 calories so avoid diet soft drinks. You need the glucose (sugar) boost. Also, don’t drink alcohol and use minimal amounts of caffeine (the equivalent of 1-2 cups of coffee). First, drink plenty of water and sports drinks (Gatorade) to prevent a diuretic like caffeine from messing up your fluid balance.
FALSE: Studies clearly show that the VO2 Max, (the best measurement of a runner’s endurance and fitness), is unchanged after one week of inactivity. And, after two weeks, the loss is less than 6% and can be regained quickly. Moreover, it is important to remember, without adequate rest and recovery, performance is comprised, not by the loss of VO2 Max, but by muscle-skeletal tissue damage, which renders the leg muscles of the runner weaker. Remember Meb Keflezighi!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

It is one week away from the 27th Steamtown Marathon. This column is dedicated to all the runners preparing for the big day. One small piece of advice; start slowly, avoid the first mile adrenaline sprint downhill, and enjoy the journey! Remember, only one Olympic marathon winner (Juan Zabala, Argentina, 1932) was in the lead at the 5 mile mark. Lesson: The last miles matter more than the first!
Today, I hope to address some common questions for the novice marathon runner or for those coming from other locations to run in the race. What should you pack? How should I dress? What supplies will I need?
Elite runners are so experienced that they know exactly what to pack in preparation for the big marathon day. However, those, running in marathon for the first or second time usually have lots of questions. First, what you need and what you can bring will depend on your support team. If you are running alone and will not have family or friends meeting you along the way, then you are limited to a fanny pack and a few supplies. If you have a support team, then they can carry a bag with supplies, meet you along the course and you can have a sense of security.
Remember; do not do anything different on race day. Try out special clothing, water with supplements and snacks on a practice run. Also, experiment with your best pre-race meal. You will be getting up at 5-6:00am to catch the bus from Scranton to Forest City. You may want to pack breakfast to eat in the high school gym such as; bagel, peanut butter, jelly, banana and coffee or Gatorade. Moving your bowels before the race is a must.
Dress: Columbus Day Weekend in NEPA could bring 30 to 40 degree temperatures when you catch the bus in Scranton and at the 8:00 am race starting time in Forest City.
Clothing:
Accessories:
If you don’t mind the little pack on your butt, a fanny pack can be valuable. In it, you will want supplies such as: small bandages, small roll of medical tape, ibuprofen, antacid tablets, small tube of lubricant, favorite running snack, and extra shoe laces. One might also consider packing a little money, credit card, ID, emergency contact numbers and medical insurance cards. A cell phone is optional.
your supply bag. In the bag, you might consider all of the above fanny pack items and: A change of clothes such as: extra running shoes, socks, shorts, shirt, water proof wind breaker, according to the weather, especially if rain is predicted. Towels, ace bandages, gauze pads and wrap, antibiotic cream, mole skin, sunscreen, petroleum jelly, safety pins, extra water and favorite sport drink, favorite sport snacks, extra ibuprofen, antacid, anti diarrhea medicine, chemical ice pack, mobile phone, money, credit cards, ID, medical insurance cards.
For those with allergic reactions, remember to pack: epinephrine, antihistamine, and other important medications.
Map and directions to the bus or starting line, course map, race number, and get your timing chip.
Enjoy! Enjoy! Smell the roses, take in the fall foliage and chat with a fellow racer. Savor the moment enjoy the day…you are doing something very special!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

The 27th Steamtown Marathon is three months away and, despite the warm weather, many local runners are deep into training. With serious heat waves of summer, any prolonged endurance activity in minimal to moderate heat can be dangerous if not prepared. Adequate hydration is critically important, not only to those training for a marathon but also for other outdoor endurance activities such as cycling, hiking, long distance power walking, etc
Next to oxygen, water is the nutrient most needed for life. A person can live without food for a month, but most can survive only three to four days without water. Even though proper hydration is essential for health, water gets overlooked as one of the six basic nutrients. Dehydration occurs when the amount of water taken into the body is less than the amount that is being lost. Dehydration can happen very rapidly (i.e. in less than eight hours); the consequences can be life threatening and the symptoms can be alarmingly swift.
In the body, water is needed to regulate body temperature, carry nutrients, remove toxins and waste materials, and provide the medium in which all cellular chemical reactions take place. Fluid balance is vital for body functions. A significant decrease in the total amount of body fluids leads to dehydration. Fluids can be lost through the urine, skin, or lungs. Along with fluids, essential electrolytes, such as sodium and potassium, are also perilously depleted in a dehydrated individual.
The risk of dehydration is not limited to endurance athletes and outdoor enthusiasts. Dehydration is the most common fluid and electrolyte disorder of frail elders, both in long term care facilities and in the community! Elders aged 85 to 99 years are six times more likely to be hospitalized for dehydration than those aged 65 to 69 years.
Is water adequate to prevent dehydration? Will a sports drink improve my performance? While some answers to these questions apply generally to all, others vary according to the temperature, humidity, length of time and intensity of the activity and condition of the athlete.
Proper hydration is essential for the comfort and safety of the recreational and serious athlete. Hydration is critical to maintain cardiovascular function, body temperature and muscle performance. As temperature, humidity, intensity, and duration of exercise increase, so too does the importance of proper hydration. Excessive sweating can lead to a loss of blood volume which requires the heart to work much harder to circulate you blood through your body.
Dehydration is a major cause of fatigue, loss of coordination, and muscle cramping leading to poor performance. Prehydration, (drinking before exercise) is the first step in preventing dehydration. Marathon runners, other long-distance runners, and cyclists often prehydrate1-2 days before a big event. Rehydration, (drinking during or after exercise) is the second step in preventing dehydration. While athletes may be more vulnerable to dehydration, all persons engaging in exercise would benefit from increased performance, delayed muscle fatigue and pain by maintaining adequate hydration. Proper prehydration would include drinking 12-16 ounces of water 1-2 hours before exercise. Athletes with other health issues should consult their family physician before engaging in long distance endurance sports.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Spring is here! So, too, is allergy season and spring sports! It seems this every year at this time a young little league baseball player wheezes as they cross home plate and desperately tries to catch their breath. Players, coaches, umpires, parents watch in dismay, deciding whether they need to call an ambulance. Minutes later the player recovers from this scary situation…until the next time. Could this be an example of exercised-induced asthma (EIA)?
Dr. Gregory Cali, a local pulmonologist, (lung doctor) was gracious enough to participate in an interview about this problem…exercise-induced asthma (EIA). The topic was chosen in response to an email question from a concerned mother of an athlete with asthma. Dr. Cali informed me that the first thing to know about exercise induced asthma (EIA) is that EIA is not a distinct disease in itself-but is one manifestation or presentation of asthma. Putting it simply, EIA occurs in patients who have develop narrowing of the bronchial tubes ( bronchoconstriction) when they exercise. Some experts would rather we use the phrase exercise induced bronchoconstriction which is what happens when someone has an asthma attack. This bronchoconstriction occurs because of spasm of the tiny muscles of the airways, plugging of the airways with thick mucous, and swelling or edema of the cells lining the airways.
In fact, it is inflammation of the airways, mostly due to allergies, that is at the root of most cases of asthma. This inflammation causes the bronchial tubes to become over-reactive-and predisposed to narrowing- when exposed to certain triggers. Exercise is one of those triggers in susceptible people. The patient with EIA complains of chest tightness, wheezing, and shortness of breath when exercising. Some patients only experience coughing with exercise. Symptoms are usually worse in cold, dry air. This is believed to be due to the drying and cooling of the airways, which occurs with exercise, especially if the patient opens his or her mouth while exercising. Nasal breathing is much better at warming and humidifying air and may help to reduce EIA.
Dr. Cali feels that the most important point about EIA is to make sure a specific diagnosis is made. It is difficult at times to differentiate asthma from the normal breathlessness, which occurs with exercise. The feature of EIA that distinguishes it from normal breathing, or being "out of shape" is the fact that EIA is ALWAYS associated with a decrease in airflow. This can be measured with either a peak flow meter or a spirometer. It is also important that a specific diagnosis be made so that a person will not be labeled as asthmatic when they may be "normal" or have other conditions such as heart problems or anemia.
Dr. Cali also recommends before a person is labeled asthmatic, they have spirometric testing. An improvement in airflow after inhaling. A bronchodilator is an important indicator of asthma. Sometimes a bronchial challenge test is needed to diagnose asthma. In this test, the subject breathes in a known bronchoconstrictor in small quantities and the response is noted. Patients with asthma almost always respond to the inhaled agent by a reduction in airflow.
Inform Coaches – If coaches are made aware, than they can be prepared for the onset of EIA. Provide emergency contacts and medications with instructions, such as inhalers, should be available.
Warm and Moisten Air - Whatever the patient can do to warm and moisten the inhaled air can help prevent EIA. Nose breathing during exercise or wearing a loose covering over the mouth in cold weather may help. Sometimes, in severe cases, switching to an indoor sport like swimming may be necessary.
Start Out Slowly - It is important to start out slowly and warm up first before exercising at full tilt. Slowly jog around the track or field before practice or a game to prepare your lungs for full-speed.
Medications – are often necessary. Quick- acting bronchodilators like Albuterol, used 15-20 minutes before planned exercise, is recommended. This can be repeated once more during the exercise, but if tightness or wheezing occurs, the exercise should be stopped. Many patients with asthma require preventative treatment with anti-inflammatory medications. Inhaled steroids and/or leukotriene inhibitors may have to be added if the asthma is not controlled with Albuterol alone. In fact, some patients with asthma who are overly reliant on quick acting bronchodilator medications can get into serious trouble if they do not use inhaled steroids. Be sure to communicate your needs with your coaches.
Play Smart - In conclusion, people with asthma should not shy away from exercise. With proper precautions, people with asthma should be able to participate in all kinds of sports activities: baseball, football, soccer, swimming, tennis and running (even a marathon)! The key point is that the asthma needs to be under control and monitored by the patient, parents, coaches and doctor as a team.
Visit your doctor regularly and listen to your body.
Medical Contributor: Gregory Cali, DO, pulmonary specialist, Dunmore, PA

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
Ice baths have become a new trend or fad in health and fitness, especially among elite athletes and some celebrities. However, it is far from a new treatment modality. In fact, the Ancient Greeks employed cold-water immersion for fever, pain relief, relaxation and socialization. In addition, Hippocrates documented the use of cold for medicinal purposes for its analgesic benefits.
Ice baths, a type of cryotherapy, is also referred to as cold water immersion (CWI) or cold water therapy. This involves immersing your body in ice water for approximately 5-15 minutes from the neck down at 50-59 degrees. The ice baths are commonly used for pain, delayed-onset muscle soreness (DOMS), and inflammation and mood elevation.
In theory, the cold water lowers the temperature of your skin and body by vasoconstriction (narrow) of the blood vessels. When you get out of the cold, water the vasodilatation (widen) of the blood vessels. Immediately, this brings fresh oxygen and nutrient-rich blood back to the tissues to warm the body and in the process, reduce pain, inflammation and promote healing.
If you have the following health conditions, ice baths may not be the best therapeutic modality for you. Before you consider trying an ice bath, consult with your physician to avoid potentially serious problems:
While some studies have shown that subjects report less muscle soreness following CWI when compared to rest, most studies suggest that the reported effects are placebo. Also, reports of improved circulation, reduced inflammation and improved recovery or performance has not been scientifically validated. In view of this, it is recommended that those considering the use of CWI for pain and inflammation management, reduced muscle soreness, and mood elevation, should consult their physician to determine if the potential risks are worth the purported benefits.
SOURCES: nih; health.com; health.clevelandclinic.org; prevention.com

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
During a recent “lunch-and-learn” meeting at our office, several younger staff members were discussing the use of supplements to compliment their fitness routines. One such staff member, Lily Smith, a physical therapy student aid at our clinic from the University of Scranton, is also a serious weight training and fitness enthusiast and shared her experience with creatine supplements with the hope of educating others, especially those preparing to “get fit” in 2024!
A National Health Interview survey found the creatine use among adolescents and young adults to be 34%. It is also very popular in the military with 27% average usage. While athletes and exercise enthusiasts use protein shakes and creatine supplements with hopes to improve size, strength and performance, it appears that most users do not have a full understanding of the risks and benefits. In view of this, today address the use of creatine in strength training and make recommendations based on the literature.
As long as I can remember, young athletes would take or do anything that they believed would improve their speed, strength, agility and athletic edge in order to succeed in sports. Running with weights wrapped around the ankles, drinking raw eggs and whole milk, and consuming copious amounts of beef, pork, and chicken were not unusual. Today, it may not be much different. However, the products do not come from our kitchen cabinet and tremendous misinformation is associated with it. Creatine is one example that was purported to enhance performance as early as the 1970’s but only gained popularity in the 1990’s. 40% of all college athletes and 50% of professional athletes admit to using creatine at some point, despite a lack of scientific evidence to support its effectiveness or safety.
This supplement is a natural substance that turns into creatine phosphate in the body. Creatine phosphate helps produce adenosine triphosphate (ATP), which provides energy for muscles to contract. While the body produces some creatine, it can also be found in foods rich in protein such as meat and fish. Manufacturers claim that creatine use will improve strength, increase lean muscle mass and aide in the recovery from exercise induced fatigue.
While creatine is popular among young people due in part to its availability, very little research has been done in people under 18 years of age. Even in the few studies conducted on adults, the results regarding efficacy are mixed. Some studies show that creatine may improve strength performance due to the recovery cycle of ATP. In theory, the use of creatine is purported to allow one to recover more quickly from exercise. For example, shortly after lifting heavy weights to failure, a quick recovery might allow the weight lifter to lift an additional set of repetitions to increase the duration of intensive training. Therefore, based on this theory, one must work out to complete failure during training to benefit from creatine. However, it is important to remember, there is no evidence that this purported benefit is realized in performance improvement in weight training or endurance sports.
Furthermore, no studies support the notion that it improves performance in endurance sports. Also, research does show that not all users are affected by creatine the same way. Most users fail to find any benefit at all. More concerning to this author is the fact that there are no guidelines for safety or disclosure of side-effects from long term use. Make no mistake, based on the research and current wisdom, CREATINE IS AN UNPROVEN TREATMENT SUPPLEMENT!
If one decides that creatine is a product they would like to use, despite the lack of evidence for its effectiveness, there are recommendations that one should follow for proper use. But there is no consistently established dose. Some studies have found 25 grams daily for 14 days as a “kickstart” dose or “loading” phase followed by 4-5 grams (or 0.1 g/kg of bodyweight) daily for 18 months with few side effects such as: muscle cramps, dehydration, upset stomach, water retention/bloating with weight gain. It is important to remember when establishing a dosage that many weight training supplements already contain creatine and in high doses excess creatine is excreted by the kidneys. It is also recommended that creatine users “wean off” the product when they decide to discontinue use.
Remember, an average adult in the United States receives 1 to 2 grams of creatine each day from a normal, well-balanced diet. Creatine is naturally found in meat, poultry and fish and theoretically, one could increase their creatine intake through dietary changes. Some manufacturers recommend 10 to 30 grams per day with a maintenance dose of 2 to 5 grams per day for athletic performance. Creatine is available in many forms; tablets, capsules and powder. It should be kept in a cool, dry place out of direct sunlight.
Creatine use is not recommended if you are pregnant, breast feeding, have kidney disease or bipolar disorder. There are many reported side effects associated with creatine use such as; water retention, nausea, diarrhea, cramping, muscle pain and high blood pressure. It is recommended that users consume large quantities of water when taking creatine to prevent dehydration. It may be very dangerous to use creatine when dehydration or weight loss is associated with an activity such as wrestling or summer sessions during football.
Furthermore, some studies show that large amounts of carbohydrates may increase the effects of creatine and caffeine may decrease the effects. Users are warned that using creatine with stimulants such as caffeine and guarana (a Brazilian plant extract similar to caffeine found in energy drinks) can lead to serious cardiac problems. The effects of creatine supplements on the many organ systems of the body are unknown. High doses may cause kidney damage. Although no cases have been reported in the literature, it is not known how it may interact with other supplements, over-the-counter medications and prescription drugs.
In conclusion, despite the lack of scientific evidence that creatine is more effective than proper nutrition and effective weight training, it remains a popular, easily available supplement purported to improve strength, endurance and performance in athletes. While relatively safe if taken as directed, it is always wise to consult your physician, especially if you have a history or risk of kidney problems. And, by the way, Lily did not feel that creatine supplements made any significant difference, positively or negatively. She no longer uses it due to the expense, inconvenience and lack of scientific evidence to support its efficacy.
Sources: University of New England; Medicine & Science in Sports & Exercise; NIH and Lily Smith, PT student, University of Scranton, Student PT aide, Mackarey Physicla Therapy
.Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
As most sports enthusiasts know, Aaron Rodgers, former Green Bay Packer quarterback and recent New York Jets QB (for just over a minute and half) suffered a season ending injury when he tore his Achilles tendon in the first game of the 2023/24 NFL season. Since then, I have been answering many questions from patients and sports fans about the nature of the Achilles Tendon rupture injury, recovery, and how to prevent it.
As the days continue to get shorter and temperatures begin a slow steady decline, athletes and exercise enthusiasts will work harder to warm-up and exercise during the winter months. A little caution and preparation are in order to avoid muscle/tendon strain, or worse yet, muscle/tendon tears, especially Achilles Tendon rupture. The Achilles tendon is one of the more common tendons torn.
This is the second of two columns on Achilles tendon rupture. Last week, I discussed the definition, sign and symptoms of the problem. This week will present examination, treatment and outcomes.
A thorough history and physical exam is the first and best method to assess the extent of the injury and determine accurate diagnosis. While a complete tear is relatively easy to determine, a partial or incomplete tear is less clear. Ultrasound and MRI are valuable tests in these cases. X-rays are not usually used and will not show tendon damage.
Consultation with an orthopedic or podiatric surgeon will determine the best treatment option for you. When conservative measures fail and for tendons completely torn, surgical intervention is usually considered to be the best option with a lower incidence of re-rupture. Surgery involves reattaching the two torn ends. In some instances, a graft using another tendon is required. A cast or walking boot is used post-operatively for 6-8 weeks followed by physical therapy.
Most people return to close to normal activity with proper management. In the competitive athlete or very active individual, surgery offers the best outcome for those with significant or complete tears, to withstand the rigors of sports. Also, an aggressive rehabilitation program will expedite the process and improve the outcome. Walking with full weight on the leg after surgery usually begins at 6 -8 weeks and often requires a heel lift to protect the tendon. Advanced exercises often begin at 12 weeks and running and jumping 5-6 months. While a small bump remains on the tendon at the site of surgery, the tendon is well healed at 6 months and re-injury does not usually occur.
Prevention of muscle and tendon tears is critical for healthy longevity in sports and activities. In addition to the Achilles tendon, the tendons of the quadriceps (knee) and rotator cuff (shoulder) are also vulnerable. A comprehensive prevention program includes: gradual introduction to new activities, good overall conditioning, sport specific training, pre-stretch warm-up, stretch, strengthening, proper shoes, clothing, and equipment for the sport and conditions. Also, utilizing interval training, eccentric exercise (lowering body weight slowly against gravity – Photo 1) and proprioceptive and agility drills are essential (Photos 2 & 3).


In PHOTO 1a & 1b: Eccentric Lowering and Lengthening: for the Achillies tendon during exercise. Beginning on the ball of both feet (1a), bend the strong knee to shift the weight onto the weak leg (1b). Slowly lowering the ankle/heel to the ground over 5-6 seconds. Repeat.
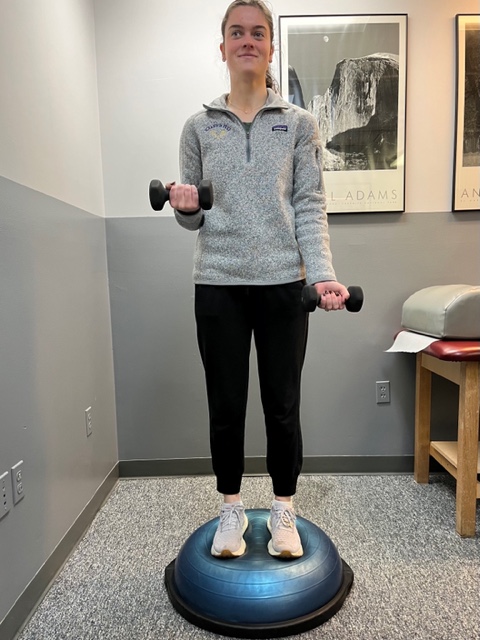
In PHOTO 2: Proprioceptive Training: for the Achillies tendon. Standing on a Bosu Ball while exercising the upper body (for example, biceps curls, shrugs, rows, lats) while maintaining balance on the ball.
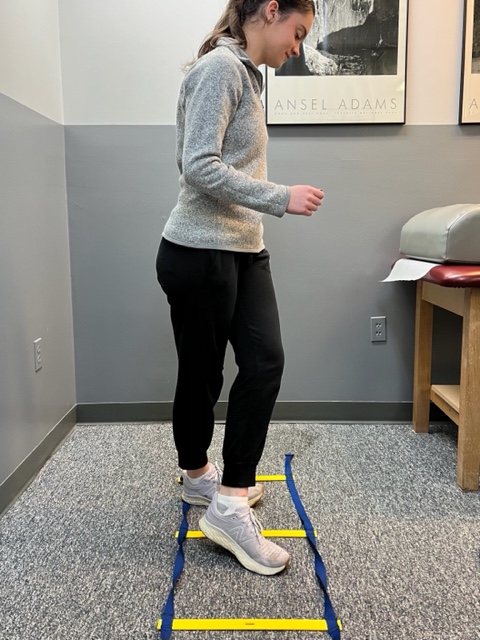
PHOTO 3: Agility Drills: for the Achilles tendon involves stepping through a “gait ladder” in various patterns and at various speeds.
MODEL: Kerry McGrath, student physical therapy aide at Mackarey Physical Therapy
Sources: MayoClinic.com;Christopher C Nannini, MD, Northwest Medical Center;Scott H Plantz, MD, Mount Sinai School of Medicine

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's articles, visit our exercise forum!
Runners will attempt to conquer 26.2 miles from Forest City to downtown Scranton in the 26th Annual Steamtown Marathon this Sunday. Participants may want to consider new research that suggests the use of compression socks may prevent post race blood clots.
Completing the long and arduous 26.2 mile journey is not an easy task. In fact, the mechanical and physiological toll on your body is tremendous; from painful joints, muscles, tendons, to black and blue toes. Not so obvious, however, is the damage to your deep veins and tissues of the circulatory system. New research indicates that strenuous endurance exercise, such as marathon running, stimulates the clotting mechanisms in your body in response to the multiple micro traumas sustained over 2 or more hours. While most healthy athletes will naturally heal from post exercise clot formation, others may be at risk…those traveling more than 1 hour (by car, bus, train or plane). The risk increases substantially for those with a longer period of travel/sitting post-race, history of previous trauma, blood clots or have the genetic predisposition for clot formation.
Compression socks are familiar to most people as the tight knee-high support stockings worn after a surgical procedure such as a knee or hip replacement to prevent blood clots. They are made with a special fabric and weave design to provide graduated compression (stronger compression at foot and ankle and less at the top of the sock) to promote better circulation and movement of fluids from the foot, ankle and calf back to the upper leg and ultimately the heart. Compression socks work similarly in runners. As the stagnant fluid with lactic acid and other byproducts of exercise is removed from the space, fresh blood, nutrients and oxygen is replaced to foster healing of micro damage to tissue and promote more efficient use of the muscles.
The Journal of Strength and Conditioning Research published a study that found wearing compression socks improved running performance. However, similar studies have failed to support this claim. One finding that has been repeatedly supported in the literature, including The British Journal of Sports Medicine, found that compression socks worn in soccer players and runners improved the rate and magnitude of recovery. Moreover, recent studies, including a study with the Boston Marathon, have demonstrated the reduction in clotting mechanisms in those wearing compression socks AFTER the marathon, as compared with those wearing “sham” socks. Benefits seem to be less obvious for short duration activities or when running 10km or less.
In conclusion, only time will tell if compression socks will improve performance in runners will or be merely a fad based on placebo or true fact supported by scientific research. Based on current wisdom, these socks may offer value and benefit AFTER activities of long duration (more than 1 hour) or long distance running (more than 10km) to expedite the recovery from exercise-induced blood clot formation, muscle soreness from the accumulation of lactic acid and other muscle damage byproducts.
It is this author’s opinion that this product is worth a try. However, whenever you try something new for your sport, trials should occur during practice and if successful used during competition. Consider trying a lower compression to begin (the socks come in different degrees of compression). Even if one is hesitant to use the product while running, it appears the greatest value of the sock is after a prolonged training session or competition to reduce exercise-induced muscle soreness and prevent blood clots, especially in athletes at risk for clotting and those traveling for an hour or more after the race. Additionally, in view of the fact that some studies which showed only minimal to moderate improvement in well-trained athletes, it may be that those in greater need, such as deconditioned individuals attempting to begin a fitness program and novice weekend athletes, may benefit more from compression socks than elite athletes.
TAKE HOME: Runners, cyclists, triathletes, soccer players and others participating in endurance sports should consider compression socks, if not during the activity, certainly following the activity for 24 to 48 hours…especially those at risk for blood clots and those traveling for more than one hour after the race.
Sunday consider trying compression socks and see if they work for you during and more importantly, after your long training runs.
Where to find compression socks:
2XU Compression Racing Sock – www.2XU.com
Scranton Running Company – Olive Street - Scranton
Visit your family doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's articles, visit our exercise forum!
Fall is here, cross-country running season has begun and the 26th Steamtown Marathon is only a few weeks away! With that in mind, running injuries, some very specific to women, are on the increase…
While driving to or from work have you noticed more local running enthusiasts in the past few years? Moreover, have your noticed that most of the runners are women? Scranton Running Company has contributed to NEPA’s participation in a national trend; more women are engaged in running than men! Female runners account for 9.7 million runners (57%) while 7 million males run on a national level.
With this surge, the female runner has been subjected to a host of related injuries, including shin splints, which often lead to stress fractures. New research has found that stress fractures may be related to the loss of weight and body mass associated with the sport.
A recent study from Ohio State University found that female runners with a Body Mass Index (BMI) below 19 may have a higher risk of developing stress fractures than women with a BMI of 19 or above. Furthermore, the study also found that these women took longer to recover from these injuries.
According to Timothy Miller, MD, “When body mass index is very low and muscle mass is depleted, there is nowhere for the shock of running to be absorbed other than directly into the bones. Until some muscle mass is developed and BMI is optimized, runners remain at increased risk of developing a stress fracture,”
The study also found that female runners with a BMI of 19 or higher with severe stress fractures required 13 weeks to recover from their injuries and return to running. Runners with a BMI lower than 19, however, took more than 17 weeks to recover.
They concluded that women should know their BMI and consult with a medical professional to maintain a healthy number. Additionally, women should cross-train and include resistance training to improve the strength and muscle mass of the lower extremities to prevent injury.
The current BMI wisdom, according to the National Institutes of Health, is 19.8 for men and 24 for women, however, strong and competitive women tend to have a BMI of 26. A BMI of 18 is considered malnourished.
Body mass index (BMI) is a measure of body fat based on height and weight of adult men and women over 20 years of age, according to the National Institutes of Health.
BMI = (weight in pounds / height in inches squared) X 703)
Example 1: a person who weighs150 pounds and is 68 inches (5 feet 8 inches) tall has a BMI of 22.8
Example 2: a person who weighs 110 pounds and is 66 inches (5 feet 5 inches) tall has a BMI of 17.7
Underweight < 18.5%
Normal weight 18.5 to 24.9%
Overweight 25 to 29.9%
Obesity 30 and over
A stress fracture is fatigue damage to bone with partial or complete disruption of the cortex of the bone from repetitive loading. While standard x-rays may not reveal the problem, a bone scan, and MRI will. It usually occurs in the long bones of the leg, mostly the tibia (shin bone) but also the femur (thigh) and foot. Occasionally, it occurs in the arm.
FEMALE RUNNERS WITH BMI LOWER THAN 19 – is a primary risk factor.
10-21% of all competitive athletes are at risk for stress fractures. Track, cross country and military recruits are at greatest risk. Females are twice as likely as males to have a stress fracture. Other athletes at risk are: sprinters, soccer and basketball players, jumpers, ballet dancers are at risk in the leg and foot. Gymnasts are also vulnerable in the spine while rowers, baseball pitchers, golfers and tennis players can experience the fracture with much less frequency in the ribs & arm.
The problem is much more prevalent in weight bearing repetitive, loading sports in which leanness is emphasized (ballet, cheerleading) or provides an advantage (distance running, gymnastics).
Stress fractures usually begin with a manageable, poorly localized pain with or immediately after activity such as a shin splint. Over time, pain becomes more localized and tender during activity and then progresses to pain with daily activity and at rest.
Source: Ohio State University, Science Daily
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy!
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Paul's Articles, visit our exercise forum!
Patients frequently ask me about the purpose of colorful tape worn by athletes on their shoulders, elbows, knees and other areas during the competition. It turns out that this look is more than “just a fashion statement!” Medical researchers have studied and published on this topic to assess its value.
The tape worn by competitive athletes is called Kinesio Tape (KT). It has become very popular in athletes using repeated overhead use of their shoulder as in volleyball, basketball and tennis. It is also used for other joints and muscles such as elbow, wrist, knee, calf and ankle. It is a special flexible tape designed to mimic the qualities of human skin. KT is very different that other forms of athletic tape. It is latex free with acrylic adhesive that is heat activated. It can be worn in the shower or pool. The cotton fibers allow for quick drying and evaporation and can be worn for 3-4 days. KT is approximately the same thickness as skin and can be stretched 30% to 40% of its length at rest.
Some reports propose that the tape has several benefits. It provides stimulation of the muscles and tissues that support the shoulder, improves space in the joint to limit pain and inflammation from impingement, and improves sensory stimulation to improve coordinated movement of the arm. Studies have found that those athletes using KT on the shoulder reported significantly less pain with overhead activities as compared to a sham tape application. No differences were reported in range of motion or ability to perform daily activities.
Impingement – when one or more of the rotator cuff muscles gets pinched between two bones. This is very common and very painful especially when you attempt to raise your hand over your head.
Rotator Cuff Tear – the rotator cuff is made up of muscles which hold the joint together. A rotator cuff can become torn (partially or fully) due to trauma such as falling on the shoulder or following wear and tear from years of overhead activities. Rotator cuff tears are common both in athletes and in the older population.
Rotator Cuff Tendonitis – inflammation of one or more of the rotator cuff tendons is often caused by overuse. Repetitive overhead activities can cause this problem.
Bursitis – inflammation of a fluid filled sack that tries to lubricate and protect the shoulder from impingement.
This is just a partial list of some of the more common problems, which can result in shoulder pain from impingement. All of these conditions are uniquely different and need to be treated differently. Some of these conditions respond well to oral medications, others to injection, others to physical therapy and still others may need surgery. If you have shoulder pain that lasts for more than three days or you notice that you cannot raise your hand over your head, you need to see either your family doctor or an orthopedic surgeon.

Read Dr. Mackarey’s Health & Exercise Forum – every Monday next week “Frozen Shoulder”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
To read all of Dr. Mackarey's articles visit: https://mackareyphysicaltherapy.com/forum/
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.