As most sports enthusiasts know, in 2021 Tiger Woods acquired an Achilles tendon rupture while training at home and in 2023 Aaron Rodgers, a former Green Bay Packer quarterback, did the same in the first game of the 2023/24 NFL season with the New York Jets. As with many sports injuries, it is painful and devastating and best managed by PREVENTION!
Spring is here! Many overjealous fitness enthusiasts will rush to pound the pavement and barely “fit in” a warm-up before participating. But, no matter how limited time is, skipping the warm-up is risky. This time of year, one can expect to feel a little cold and stiff, especially if you are over 40, and therefore a little caution and preparation are in order to avoid muscle/tendon strain, or worse yet, muscle/tendon tears. The Achilles tendon is one of the more common tendons torn. Prevention of muscle tears, including the Achilles tendon includes; gradual introduction to new activities, good overall conditioning, sport specific training, pre-stretch warm-up, stretch, strengthening, proper shoes, clothing, and equipment for the sport and conditions.
This is the second of two columns on Achilles tendon rupture. Last week, I discussed the definition, sign and symptoms of the problem. This week will present examination, treatment and outcomes.
A thorough history and physical exam is the first and best method to assess the extent of the Achilles tendon rupture and/or injury and determine accurate diagnosis. While a complete tear is relatively easy to determine, a partial or incomplete tear is less clear. Ultrasound and MRI are valuable tests in these cases. X-rays are not usually used and will not show tendon damage.
Consultation with an orthopedic or podiatric surgeon will determine the best treatment option for you. When conservative measures fail and for complete Achilles tendon ruptures, surgical intervention is usually considered to be the best option with a lower incidence of re-rupture. Surgery involves reattaching the two torn ends. In some instances, a graft using another tendon is required. A cast or walking boot is used post-operatively for 6-8 weeks followed by physical therapy.
Most people return close to normal activity with proper management. In the competitive athlete or very active individual, surgery offers the best outcome for those with significant or complete tears, to withstand the rigors of sports. Also, an aggressive rehabilitation program will expedite the process and improve the outcome. Walking with full weight on the leg after surgery usually begins at 6 -8 weeks and often requires a heel lift to protect the tendon. Advanced exercises often begin at 12 weeks and running and jumping 5-6 months. While a small bump remains on the tendon at the site of surgery, the tendon is well healed at 6 months and re-injury does not usually occur.
Prevention of muscle and tendon tears is critical for healthy longevity in sports and activities. In addition to the Achilles tendon, the tendons of the quadriceps (knee) and rotator cuff (shoulder) are also vulnerable. A comprehensive prevention program includes; gradual introduction to new activities, good overall conditioning, sport specific training, pre-stretch warm-up, stretch, strengthening, proper shoes, clothing, and equipment for the sport and conditions. Also, utilizing interval training, eccentric exercise (lowering body weight slowly against gravity and proprioceptive and agility drills are essential.
Eccentric Lowering and Lengthening: for the Achillies tendon during exercise. Beginning on the ball of both feet (1a), bend the strong knee to shift the weight onto the weak leg (1b). Slowly lowering the ankle/heel to the ground over 5-6 seconds. Repeat.
Proprioceptive Training: for the Achillies tendon. Standing on a Bosu Ball while exercising the upper body (for example, biceps curls, shrugs, rows, lats) while maintaining balance on the ball.
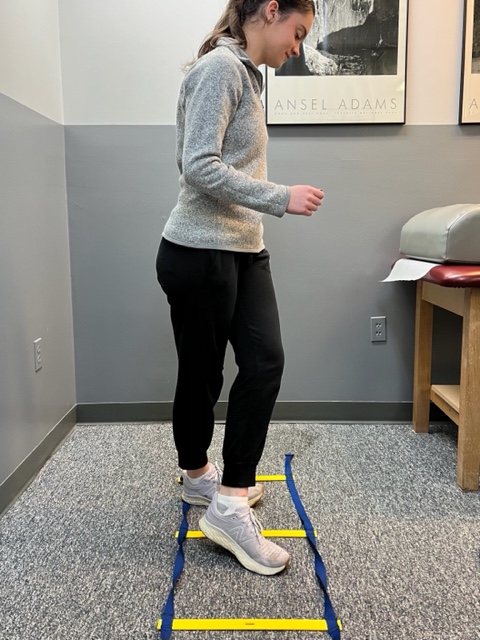
Agility Drills: for the Achilles tendon involves stepping through a “gait ladder” in various patterns and at various speeds.
Sources: MayoClinic.com;Christopher C Nannini, MD, Northwest Medical Center;Scott H Plantz, MD, Mount Sinai School of Medicine

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

As most sports enthusiasts know, in 2021 Tiger Woods ruptured his Achilles tendon while training at home and in 2023 Aaron Rodgers, a former Green Bay Packer quarterback, did the same in the first game of the 2023/24 NFL season with the New York Jets. As with many sports injuries, it is painful and devastating and best managed by PREVENTION!
Spring is here and as the days continue to get longer and temperatures begin a slow steady rise, athletes and weekend warriors are eager to get outdoors to play and exercise. However, be mindful of the weather (damp and rainy), temperature (cool mornings and evenings) and winter “dust” on your muscles and tendons. Many overjealous fitness enthusiasts will rush to pound the pavement and barely “fit in” a warm-up before participating. But, no matter how limited time is, skipping the warm-up is risky.
This time of year, one can expect to feel a little cold and stiff, especially if you are over 40, and therefore a little caution and preparation are in order to avoid muscle/tendon strain, or worse yet, muscle/tendon tears. The Achilles tendon is one of the more common tendons torn. Prevention of muscle tears, including the Achilles tendon includes; gradual introduction to new activities, good overall conditioning, sport specific training, pre-stretch warm-up, stretch, strengthening, proper shoes, clothing, and equipment for the sport and conditions.
A muscle contracts to move bones and joints in the body. The tendon is the fibrous tissue that attaches muscle to bone. Great force is transmitted across a tendon which, in the lower body, can be more than 5 times your body weight. Often, a tendon can become inflamed, irritated, strained or partially torn from improper mechanics or overuse. Although infrequent, occasionally tendons can also snap or rupture. A tendon is more vulnerable to a rupture for several reasons such as a history of repeated injections of steroids into a tendon and use of medications such as corticosteroids and some antibiotics. Certain diseases such as gout, arthritis, diabetes or hyperparathyroidism can contribute to tendon tears. Also, age, obesity and gender are significant risk factors as middle-aged, overweight males are more susceptible to tendon tears. Poor conditioning, improper warm-up and cold temperatures may also contribute to the problem.
Tendon rupture is very painful and debilitating and must not be left untreated. While conservative management is preferred, surgical management is usually required for complete tears. The purpose of this column is to present the signs, symptoms and management of Achilles tendon ruptures.
The Achilles tendon (also called the calcaneal tendon), is a large, strong cordlike band of fibrous tissue in the back of the ankle. The tendon (also called the heel cord) connects the powerful calf muscle to the heel bone (also called the calcaneus). When the calf muscle contracts, (as when you walk on the ball of your foot), the Achilles tendon is tightened, tension is created at the heel and the foot points down like pushing a gas pedal or walking on tip of your toes. This motion is essential for activities such as walking, running, and jumping. A partial tear of the tendon would make these activities weak and painful, while a full tear through the tendon would render these activities impossible.
With age, the Achilles tendon (and other tendons) gets weak, thin, and dehydrated, thus making it prone to inflammation, degeneration, partial tear or rupture. The middle-aged weekend warrior is at greatest risk. A full or complete tear (Achilles tendon rupture) usually occurs about 2 inches above the heel bone and is associated with a sudden burst of activity followed by a quick stop or a quick start or change in direction, as in tennis, racquet ball, and basketball.
In some instances, the tendon can be injured by a violent contraction of calf when you push off forcefully at the same time the knee is locked straight as in a sudden sprint. Other times, the tendon is injured when a sudden and unexpected force occurs as in a trip off a curb or sudden step into a hole or a quick attempt to break a fall.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
Next Week: Achilles tendon Part II of II
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

I have been advising my patients to exercise, keep active, and walk as long as they can in order to stay mobile and healthy. However, seniors often tell me activities that require prolonged walking is limited by ankle pain from arthritis. They often ask, “What is arthritis of the ankle?” How does it happen? What can I do about it?
Your family physician will examine your ankle to determine if you have arthritis. In more advanced cases you may be referred to a specialist such as a podiatrist, orthopaedic surgeon or rheumatologist for further examination and treatment. X-rays will show if the joint space between the bones in the ankle is getting narrow from wear and tear arthritis. If rheumatoid arthritis is suspected, blood tests and an MRI may be ordered. The diagnosis will determine if you problem if minor, moderate or severe.
In the early stages your treatment will be a conservative, nonsurgical approach, which may include; anti-inflammatory medication, orthopedic physical therapy, exercise, activity modifications, supplements, bracing, etc. You and your family physician, podiatrist, orthopedic surgeon or rheumatologist will decide which choices are best.
When conservative measures no longer succeed in controlling pain and deformity, improving strength and function then more aggressive treatment may be necessary.
SOURCES: Rothman Institute, Philadelphia, PA and American Academy of Orthopaedic Surgeons
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
As most sports enthusiasts know, Aaron Rodgers, former Green Bay Packer quarterback and recent New York Jets QB (for just over a minute and half) suffered a season ending injury when he tore his Achilles tendon in the first game of the 2023/24 NFL season. Since then, I have been answering many questions from patients and sports fans about the nature of the Achilles Tendon rupture injury, recovery, and how to prevent it.
As the days continue to get shorter and temperatures begin a slow steady decline, athletes and exercise enthusiasts will work harder to warm-up and exercise during the winter months. A little caution and preparation are in order to avoid muscle/tendon strain, or worse yet, muscle/tendon tears, especially Achilles Tendon rupture. The Achilles tendon is one of the more common tendons torn.
This is the second of two columns on Achilles tendon rupture. Last week, I discussed the definition, sign and symptoms of the problem. This week will present examination, treatment and outcomes.
A thorough history and physical exam is the first and best method to assess the extent of the injury and determine accurate diagnosis. While a complete tear is relatively easy to determine, a partial or incomplete tear is less clear. Ultrasound and MRI are valuable tests in these cases. X-rays are not usually used and will not show tendon damage.
Consultation with an orthopedic or podiatric surgeon will determine the best treatment option for you. When conservative measures fail and for tendons completely torn, surgical intervention is usually considered to be the best option with a lower incidence of re-rupture. Surgery involves reattaching the two torn ends. In some instances, a graft using another tendon is required. A cast or walking boot is used post-operatively for 6-8 weeks followed by physical therapy.
Most people return to close to normal activity with proper management. In the competitive athlete or very active individual, surgery offers the best outcome for those with significant or complete tears, to withstand the rigors of sports. Also, an aggressive rehabilitation program will expedite the process and improve the outcome. Walking with full weight on the leg after surgery usually begins at 6 -8 weeks and often requires a heel lift to protect the tendon. Advanced exercises often begin at 12 weeks and running and jumping 5-6 months. While a small bump remains on the tendon at the site of surgery, the tendon is well healed at 6 months and re-injury does not usually occur.
Prevention of muscle and tendon tears is critical for healthy longevity in sports and activities. In addition to the Achilles tendon, the tendons of the quadriceps (knee) and rotator cuff (shoulder) are also vulnerable. A comprehensive prevention program includes: gradual introduction to new activities, good overall conditioning, sport specific training, pre-stretch warm-up, stretch, strengthening, proper shoes, clothing, and equipment for the sport and conditions. Also, utilizing interval training, eccentric exercise (lowering body weight slowly against gravity – Photo 1) and proprioceptive and agility drills are essential (Photos 2 & 3).


In PHOTO 1a & 1b: Eccentric Lowering and Lengthening: for the Achillies tendon during exercise. Beginning on the ball of both feet (1a), bend the strong knee to shift the weight onto the weak leg (1b). Slowly lowering the ankle/heel to the ground over 5-6 seconds. Repeat.
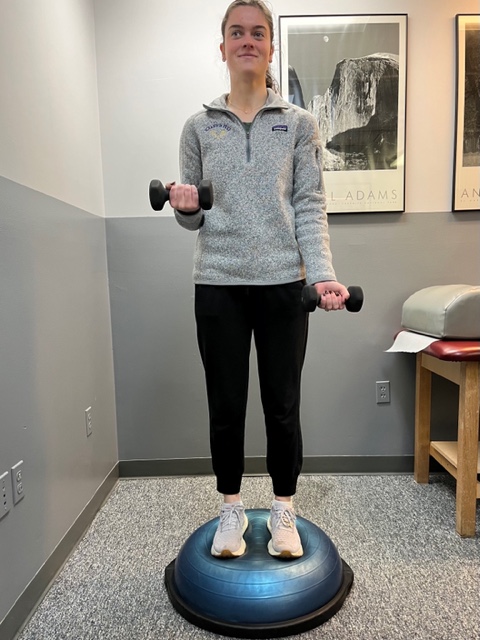
In PHOTO 2: Proprioceptive Training: for the Achillies tendon. Standing on a Bosu Ball while exercising the upper body (for example, biceps curls, shrugs, rows, lats) while maintaining balance on the ball.
PHOTO 3: Agility Drills: for the Achilles tendon involves stepping through a “gait ladder” in various patterns and at various speeds.
MODEL: Kerry McGrath, student physical therapy aide at Mackarey Physical Therapy
Sources: MayoClinic.com;Christopher C Nannini, MD, Northwest Medical Center;Scott H Plantz, MD, Mount Sinai School of Medicine

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's articles, visit our exercise forum!
As most sports enthusiasts know, Aaron Rodgers, former Green Bay Packer quarterback and recent New York Jets QB (for just over a minute and half) suffered a season ending injury when he tore his Achilles tendon in the first game of the 2023/24 NFL season. Since then, I have been answering many questions from many about the nature of the injury and how to prevent it.
As the days continue to get shorter and temperatures begin a slow steady decline, athletes and exercise enthusiasts will work harder to “fit in” a warm-up before running or other activities during the winter months. But, no matter how limited time is, skipping the warm-up is risky. This time of year, one can expect to feel a little cold and stiff, especially if you are over 40, and therefore a little caution and preparation are in order to avoid muscle/tendon strain, or worse yet, muscle/tendon tears. The more commonly torn tendon is the Achilles tendon . Prevention of muscle tears, including the Achilles tendon includes; gradual introduction to new activities, good overall conditioning, sport specific training, pre-stretch warm-up, stretch, strengthening, proper shoes, clothing, and equipment for the sport and conditions.
A muscle contracts to move bones and joints in the body. The tendon is the fibrous tissue that attaches muscle to bone. Great force is transmitted across a tendon which, in the lower body, can be more than 5 times your body weight. Often, a tendon can become inflamed, irritated, strained or partially torn from improper mechanics or overuse. Although infrequent, occasionally tendons can also snap or rupture. A tendon is more vulnerable to a rupture for several reasons such as a history of repeated injections of steroids into a tendon and use of medications such as corticosteroids and some antibiotics. Certain diseases such as gout, arthritis, diabetes or hyperparathyroidism can contribute to tendon tears. Also, age, obesity and gender are significant risk factors as middle-aged, overweight males are more susceptible to tendon tears. Poor conditioning, improper warm-up and cold temperatures may also contribute to the problem.
Tendon rupture is very painful and debilitating and must not be left untreated. While conservative management is preferred, surgical management is usually required for complete tears. The purpose of this column is to present the signs, symptoms and management of Achilles tendon ruptures.
The Achilles tendon (also called the calcaneal tendon), is a large, strong cordlike band of fibrous tissue in the back of the ankle. The tendon (also called the heel cord) connects the powerful calf muscle to the heel bone (also called the calcaneus). When the calf muscle contracts, (as when you walk on the ball of your foot), the Achilles tendon is tightened, tension is created at the heel and the foot points down like pushing a gas pedal or walking on tip of your toes. This motion is essential for activities such as walking, running, and jumping. A partial tear of the tendon would make these activities weak and painful, while a full tear through the tendon would render these activities impossible.
With age, the Achilles tendon (and other tendons) gets weak, thin, and dehydrated, thus making it prone to inflammation, degeneration, partial tear or rupture. The middle-aged weekend warrior is at greatest risk. A full or complete tear (Achilles tendon rupture) usually occurs about 2 inches above the heel bone and is associated with a sudden burst of activity followed by a quick stop or a quick start or change in direction, as in tennis, racquet ball, and basketball.
In some instances, the tendon can be injured by a violent contraction of calf when you push off forcefully at the same time the knee is locked straight as in a sudden sprint. Other times, the tendon is injured when a sudden and unexpected force occurs as in a trip off a curb or sudden step into a hole or a quick attempt to break a fall.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog Next Week: Achilles tendon Part II of II.
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's articles, visit our exercise forum!
Ankle swelling is a common symptom that occurs when your body retains fluid in the lower legs, ankles and feet. Most people have experienced it at some point in their lives and it often resolves on its own with elevation and muscle movement. While it is usually benign and occurs on both sides of the body, in some instances immediate medical attention is required. The most common causes of ankle swelling are:
Prolonged Positions – you have probably noticed swelling in your ankles and feet after a long trip by plane or car. Some may also experience symptoms after a long day at work sitting or standing in one position for an extended period of time. It may be the most common cause of lower leg swelling and easiest to resolve.
Diet- excessive salt in your diet is associated with swelling in the lower legs, especially when associated with other risk factors for swelling such as organ function or obesity.
Varicose Veins – when the valves in the blood vessels which carry blood from the legs back to the heart are damaged, blood and fluid can collect in the lower legs. Prolonged standing or sitting without intermittent movement with worsen the condition.
Pregnancy – during pregnancy, the body retains more fluids than usual and most women experience some form of swelling in the lower legs, ankles and feet.
Medications – certain drugs can cause fluid retention in the lower legs such as: anti-inflammatory medications, steroids, diabetes medications, antidepressants and cardiac medications.
Blood Clots – blockages in the blood vessels of the lower leg can limit the movement of fluid from the legs back to the heart. It is often present in only one leg and associated with warmth, pain, and cramping. It is a serious condition and requires immediate medical attention.
Trauma/Infection – after a trauma or injury such as an ankle sprain, bruise or fracture, the damaged tissue leaks fluid surrounding the affected area. Also, when specific area of the lower leg can becomes infected, as in the case of a cut or splinter in the ankle or foot that has not healed properly, swelling occurs in the surrounding tissues. These situations are often associated with warmth, pain and limited to the side of the injury. Treatment to injured tissues and the infection is required.
Lymphedema – swelling in the lower leg can occur when there is a blockage in the lymphatic system is blocked or when lymph nodes are removed in surgery for cancer. Medications, massage, compression garments, and elevation, can address the symptoms.
Obesity – due to the excessive weight placed on the tissues of the legs, ankle and feet and adipose tissue in the abdomen compressing blood vessels, obesity is one of the most common causes of lower leg swelling. It also complicates all of the above conditions associated with swelling in the legs.
Diseases – such as those of the kidney, heart, and liver are associated with swelling in the lower legs.
Change Positions – on a long plane ride or sitting all day at school or work – get up and walk around every 30-45 minutes. Set a timer on your phone to remind you.
Exercise – regular exercises keeps the muscles and blood vessels in you lower extremities healthier. Also, intermittent movement of the leg muscles throughout the day, even when sitting, serve to prevent swelling. Try ankle pumps and toe curls.
Elevation – when sitting or lying down, try elevating your ankles and feet on a pillow to allow gravity to assist fluid movement in your legs.
Low-Sodium Diet – read the labels on your food and you will be shocked by how much sodium is in most foods, especially canned soups and vegetables. But, there are low-sodium options and don’t add more salt to your food.
Weight Loss – maintaining a healthy BMI is the single best thing you can do, not only for lower leg swelling, but for your overall health and wellness.
Compression Socks – for most people, over-the-counter compression socks will adequately prevent fluid retention in the lower legs. For comfort, begin with the lightest compression possible. 12-15 or 15-20 mm of mercury is a good start and put them on as soon as you get up in the morning, before swelling begins.
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in ”The Sunday Times - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Paul's articles, check out our exercise forum!