Osteochondritis dissecans, also called OCD, is the most common cause of a loose body or fragment in the knee and is usually found in young males between the ages of ten and twenty. While this word sounds like a mouth full, breaking down its Latin derivation to its simplest terms makes it understandable: “osteo” means bone, “chondro” means cartilage, “itis” means inflammation, and “dissecans” means dissect or separate. In OCD, a flap of cartilage with a thin layer of bone separates from the end of the bone. As the flap floats loosely in the joint, it becomes inflamed, painful and disrupts the normal function of the joint.
Typically, OCD is found in the knee joint of active young men who participate in sports which involve jumping or full contact. Although less common, it is also found in other joints such as the elbow.
Often, the exact cause of OCD is unknown. For a variety of reasons, blood flow to the small segment at the end of the bone lessens and the weak tissue breaks away and becomes a source of pain in the joint. Long term, OCD can increase the risk of osteoarthritis in the involved joint.
To properly diagnose OCD a physician will consider onset, related activities, symptoms, medical history, and examine the joint involved for pain, tenderness, loss of strength and limited range of motion. Often, a referral to a specialist such as an orthopedic surgeon for further examination is necessary. Special tests specifically detect a defect in the bone or cartilage of the joint such as:
Radiograph (X-ray) may be performed to assess the bones.
Magnetic Resonance Imaging (MRI) may be performed to assess bones and other soft tissues such as cartilage, ligaments, muscles and tendons.
The primary goal of treatment for OCD is to relieve pain, control swelling, and restore the complete function (strength and range of motion) of the joint. The age of the patient and severity of the injury determine the treatment methods. For example, medications assist with pain and inflammation reduction.
Young patients who are still growing have a good chance of healing with conservative treatment. Rest and physical therapy are the conservative treatments of choice. Rest entails avoiding any activity that compresses the joint such as jumping, running, twisting, squatting, etc. In some cases, using a splint, brace and crutches to protect the joint and eliminate full weight bearing, may be necessary for a few weeks. Physical therapy, either as a conservative or post operative treatment, involves restoring the range of motion with stretching exercises and improving the strength and stability of the joint through strengthening exercises. Modalities for pain and swelling such as heat, cold, electrical stimulation, ultrasound, compression devices assist with treatment depending on the age of the patient and severity of the problem.
Conservative treatment can often require 3 to 6 months to be effective. However, if it fails, arthroscopic surgery stimulates healing or reattaches the loose fragment of cartilage and bone. In some cases if the defect is small, surgery involves filling in the defect with small bundles of cartilage. In other cases, the fragment is reattached directly to the defect using a small screw or bioabsorbable device. More recently, surgeons are using the bone marrow of the patient to repair the deficit by stimulating the growth of new tissue (bone marrow stimulation).
In other cases, a plug of healthy tissue from the non-weight bearing surface of a patient's knee relocated to the defect to stimulate healing (osteochondral autograft transplantation OATS). While there are many surgical options for OCD, an orthopedic surgeon will help the patient decide the most appropriate procedure based on age, size of defect, and other factors.
While prevention is not always possible, some measures can be taken to limit risk. For example, if a child playing sports has a father and older brother who had OCD, then it would be wise to consider the following: Avoid or make modifications for sports requiring constant jumping. Cross-train for a sport to avoid daily trauma (run one day and bike the next). Also, do not play the sport all year round (basketball in the fall/winter and baseball in the spring/summer). Seek the advice from an orthopedic or sports physical therapist to learn proper strength and conditioning techniques. Learn proper biomechanics of lifting, throwing, squatting, running, jumping and landing.
Sources: Mayo Clinic

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Fall has arrived in NEPA and walking is a great way to enjoy the fall foliage. Moreover, a new study has found that walking can reduce lower back pain. Researchers in Australia followed more than 700 adults who had a recent onset of lower back pain (and were able to bear full weight without associated leg symptoms) and enrolled them in a walking program under the supervision of a physical therapist. One group walked for 30 minutes, 3-5 times per week and the control group remained inactive. Both groups were followed for more than three years and discovered that the inactive control group was twice as likely to suffer from repeated flare-ups of lower back pain when compared to the walking group.
It is good news for those who enjoy walking, however, for many who have not maintained an active lifestyle or have health issues, it is challenging to know where to begin. Also, beginning without a good plan can lead to injury and leave you discouraged. For example, those overweight and de-conditioned should not start a walking program too aggressively. Walking at a fast pace and long distance without gradually weaning yourself into it will most likely lead to problems.
There is probably nothing more natural to human beings than walking. Ever since Australopithecus, an early hominin (human ancestor) who evolved in Southern and Eastern Africa between 4 and 2 million years ago, our ancestors took their first steps as committed bipeds. With free hands, humans advanced in hunting, gathering, making tools etc. while modern man uses walking as, not only a form of locomotion, but also as a form of exercise and fitness. It is natural, easy and free...no equipment or fitness club membership required!
Walking to reduce or control lower back pain is only one of many important reasons to begin a program. According to the American Heart Association, walking as little as 30 minutes a day can provide the following benefits:
Anything is better than nothing! However, for most healthy adults, the Department of Health and Human Services recommends at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous aerobic activity, or an equivalent combination of moderate and vigorous aerobic activity. The guidelines suggest that you spread out this exercise during the course of a week. Also aim to do strength training exercises of all major muscle groups at least two times a week.
As a general goal, aim for at least 30 minutes of physical activity a day. If you can't set aside that much time, try several short sessions of activity throughout the day (3 ten or 2 fifteen-minute sessions). Even small amounts of physical activity are helpful, and accumulated activity throughout the day adds up to provide health benefit.
Remember it's OK to start slowly — especially if you haven't been exercising regularly. You might start with five minutes a day the first week, and then increase your time by five minutes each week until you reach at least 30 minutes.
For even more health benefits, aim for at least 60 minutes of physical activity most days of the week. Once you are ready for a challenge, add hills, increase speed and distance.
Keeping a record of how many steps you take, the distance you walk and how long it takes can help you see where you started from and serve as a source of inspiration. Record these numbers in a walking journal or log them in a spreadsheet or a physical activity app. Another option is to use an electronic device such as a smart watch, pedometer or fitness tracker to calculate steps and distance.
Make walking part of your daily routine. Pick a time that works best for you. Some prefer early morning, others lunchtime or after work. Enter it in your smart phone with a reminder and get to it!
Studies show that compliance with an exercise program is significantly improved when an exercise buddy is part of the equation. It is hard to let someone down or break plans when you commit to someone. Keep in mind that your exercise buddy can also include your dog!
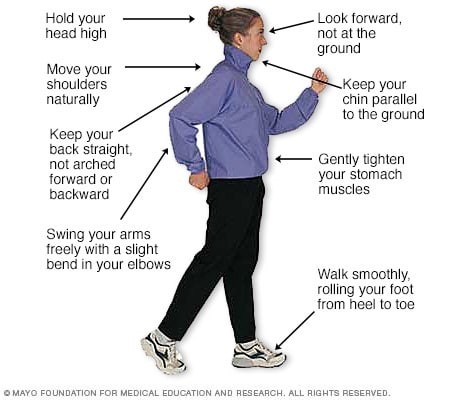
Like everything, there is a right way of doing something, even walking. For efficiency and safety, walking with proper stride is important. A fitness stride requires good posture and purposeful movements. Ideally, here's how you'll look when you're walking:
Sources : Sapiens.org; WebMD; Mayo Clinic, “Health & Science New”
Visit your doctor regularly and listen to your body

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Age-related changes to your body are normal and expected. For example, loss of muscle tone, stiffness in joints, and loss of balance. With effort, some of these changes can be retarded and managed with stretching, strengthening and balance exercises. The brain is no different…it can slow down and lead to memory lapses. However, for most of us, it too can be managed and with a little effort, be kept sharp and clear.
Many experts feel that exercise is the best method to maintain not only physical health but mental health. Regular exercise can prevent the things that contribute to memory loss with age such as; diabetes, high blood pressure, high cholesterol, obesity and stroke.
Specifically, aerobic exercise may be most beneficial. Aerobic exercise is any type of sustained exercise that strengthens the heart and lungs to improve the body’s use of oxygen. This may include running/jogging, brisk walking, cycling, swimming, rowing, and the use of a treadmill, elliptical, stepper or similar device, at light to moderate intensity which requires the use of oxygen to adequately meet the oxygen demands of the body for an extended period of time. The generally accepted time and frequency is at least 30 minute sessions performed three or more times per week. Two 15 minute or three 10 minute sessions are also valuable. For those with back, hip, knee and other lower body pain, consider low-impact or partial weight-bearing activities such as a recumbent bike or stepper or upright bike instead of a treadmill.
The benefits of a healthy diet are well-documented. Specifically, a Mediterranean-style diet comes highly recommended. It focuses on plenty of fruits and vegetables with fish instead of red meat and olive oil instead of butter. Researchers found people who closely adhered to a Mediterranean diet were nearly 20% less likely to have thinking and memory problems.
Exercise your brain just as you do your body. Make time each day to challenge your brain. Learn something new to keep your mind sharp. Play cards, read a book, do crossword puzzles or other word games, take a class or learn play a musical instrument.
Human beings are social animals and in the right setting, we stimulate and challenge each other. Join a book club, fitness center, or a community center. Consider volunteering, taking an art or photography class. Social interaction can prevent isolation which can lead to depression and depression is associated with dementia.
Without adequate sleep, attention and concentration is compromised. Studies show that those who have normal restful sleep outperform those who are restless and sleep deprived. Some tips for better sleep are: avoid big meals before bed, keep a consistent sleep and wake up time, avoid nicotine, caffeine and alcohol close to bedtime. “
Consider an afternoon “power nap!” Recent studies show that an afternoon nap was rejuvenating to the mind and body. Participants improved on mental skills such as memory, calculation, orientation and attention.
Cortisol is the hormone associated with stress. Recent studies have found that elevated cortisol levels were associated with poorer overall cognitive functioning, including memory, language, and processing speed.
Try yoga, massage, breathing techniques to relax. Progressive muscle relaxation (PMR) techniques can be very effective…try it on YouTube!
Smoking is clearly one of the worst things you can do to your body AND MIND! Smoking can lead to early memory lose in part due to small strokes in the brain. Do whatever it takes to quit; nicotine replacement, medication, or counseling.
There are many medical conditions and medications associated with memory loss. Regular medical check-ups can prevent, diagnose and treat some of these conditions such as; depression, diabetes, thyroid disease, vitamin deficiencies, and drug interactions or side effects. For example, sleep aid and anxiety drugs associate with memory loss.
In addition to common tricks such as word association, sticky notes, use your smart phone for appointments and reminders. If you don’t know how to use a smart phone, it is time to learn something new…and that is a healthy brain activity!
SOURCES: WebMD; Harvard Health

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Congratulations to more than 1,000 courageous runners who finished the 27th Annual Steamtown Marathon today. Most, if not all of you are waking up this morning with a little less jump in your step than you had yesterday.
As active people by nature, many of you will resist the logic of rest, despite the pain and stiffness in your muscles and joints. Therefore, I would like to offer some words of wisdom, based on science, to encourage you to adequately rest and allow your body to recover.
With adequate rest and recovery, an elite runner can quickly regain full form in 3-4 weeks, while an average runner may require 4-6 weeks. Meb Keflezighi, an elite American runner and winner of the 2014 Boston Marathon, is an excellent example of the merits of rest and recovery. However, he discovered it by accident…following the 2012 New York City Marathon, Meb developed a foot infection which required three weeks rest. With the Olympic Trials just 70 days away, Meb quickly regained his pre-injury fitness level to win the 2012 US Olympic Marathon Trials and join the US Olympic Team in London. It may be that his injury was fortuitous and allowed him adequate recovery time, (that he might not have otherwise allowed), preparing him for intensive training leading up to the trials.
The Effects of Running 26.2 Miles on the Body:
(RunNow.com - Jim Peskett)
One of the most obvious effects of running a marathon is significant muscle and joint pain and stiffness. It will set in after you sit for a while and attempt to get up and move around. For most, it will be more pronounced the day after the marathon, as you get out of bed and limp to the bathroom. Studies show that the leg muscles, (especially the calf muscles) display significant inflammation and necrosis (dead tissue) in the fibers of the muscle. In other words, the trauma to the muscles is so severe that tissue damage causes muscle cells to die. Consequently, studies found that muscle strength, power and endurance is compromised and required significant time to recover… sometimes as long as 4-6 weeks!
Additionally, many runners report severe bone and joint pain following the race. Some studies report findings of microfractures or bone bruising from the repeated and prolonged pounding of the marathon. It is purported that the stress on the joints may be related to: weight and body type, running shoes, running style and mechanics. While not dangerous, again, it is important to respect the stress placed on the body and allow adequate healing…LISTEN TO YOUR BODY!
Creatine kinase is an enzyme found in the brain, skeletal muscles and heart. It is found in elevated levels in the presence of cellular damage to these tissues, for example, following a heart attack. Similarly, significantly elevated creatine kinase levels are found in the blood of runners up to 4 days post marathon, demonstrating extensive tissue damage at the cellular level. It is important to note, that these enzyme markers are present, even if a runner does not experience muscle soreness. So, adequate rest for healing and recovery is required, regardless of soreness.
It is not a coincidence that the runners are more likely to contract colds and flu after intensive training or running 26.2 miles. The immune system is severely compromised after a marathon and without adequate recovery; a runner can become ill and ultimately lose more training time or will underperform.
FALSE: As stated above, enzyme levels that indicate cellular damage to the tissues are present in the post-marathon runner, even in those without significant pain.
FALSE: In addition to rest, drink, drink, drink - 24 ounces of water for every 2 pounds you lose after the marathon. This is based on pre and post exercise weight. You just burned 2,600 calories so avoid diet soft drinks. You need the glucose (sugar) boost. Also, don’t drink alcohol and use minimal amounts of caffeine (the equivalent of 1-2 cups of coffee). First, drink plenty of water and sports drinks (Gatorade) to prevent a diuretic like caffeine from messing up your fluid balance.
FALSE: Studies clearly show that the VO2 Max, (the best measurement of a runner’s endurance and fitness), is unchanged after one week of inactivity. And, after two weeks, the loss is less than 6% and can be regained quickly. Moreover, it is important to remember, without adequate rest and recovery, performance is comprised, not by the loss of VO2 Max, but by muscle-skeletal tissue damage, which renders the leg muscles of the runner weaker. Remember Meb Keflezighi!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

It is one week away from the 27th Steamtown Marathon. This column is dedicated to all the runners preparing for the big day. One small piece of advice; start slowly, avoid the first mile adrenaline sprint downhill, and enjoy the journey! Remember, only one Olympic marathon winner (Juan Zabala, Argentina, 1932) was in the lead at the 5 mile mark. Lesson: The last miles matter more than the first!
Today, I hope to address some common questions for the novice marathon runner or for those coming from other locations to run in the race. What should you pack? How should I dress? What supplies will I need?
Elite runners are so experienced that they know exactly what to pack in preparation for the big marathon day. However, those, running in marathon for the first or second time usually have lots of questions. First, what you need and what you can bring will depend on your support team. If you are running alone and will not have family or friends meeting you along the way, then you are limited to a fanny pack and a few supplies. If you have a support team, then they can carry a bag with supplies, meet you along the course and you can have a sense of security.
Remember; do not do anything different on race day. Try out special clothing, water with supplements and snacks on a practice run. Also, experiment with your best pre-race meal. You will be getting up at 5-6:00am to catch the bus from Scranton to Forest City. You may want to pack breakfast to eat in the high school gym such as; bagel, peanut butter, jelly, banana and coffee or Gatorade. Moving your bowels before the race is a must.
Dress: Columbus Day Weekend in NEPA could bring 30 to 40 degree temperatures when you catch the bus in Scranton and at the 8:00 am race starting time in Forest City.
Clothing:
Accessories:
If you don’t mind the little pack on your butt, a fanny pack can be valuable. In it, you will want supplies such as: small bandages, small roll of medical tape, ibuprofen, antacid tablets, small tube of lubricant, favorite running snack, and extra shoe laces. One might also consider packing a little money, credit card, ID, emergency contact numbers and medical insurance cards. A cell phone is optional.
your supply bag. In the bag, you might consider all of the above fanny pack items and: A change of clothes such as: extra running shoes, socks, shorts, shirt, water proof wind breaker, according to the weather, especially if rain is predicted. Towels, ace bandages, gauze pads and wrap, antibiotic cream, mole skin, sunscreen, petroleum jelly, safety pins, extra water and favorite sport drink, favorite sport snacks, extra ibuprofen, antacid, anti diarrhea medicine, chemical ice pack, mobile phone, money, credit cards, ID, medical insurance cards.
For those with allergic reactions, remember to pack: epinephrine, antihistamine, and other important medications.
Map and directions to the bus or starting line, course map, race number, and get your timing chip.
Enjoy! Enjoy! Smell the roses, take in the fall foliage and chat with a fellow racer. Savor the moment enjoy the day…you are doing something very special!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Like many of you, I have always enjoyed the outdoors...walking, running, biking, hiking etc. However, recently, I have been more concerned about being safe, (getting older and more cautious, distracted drivers) when doing these activities on the side of the road.
Almost 15 percent of all motor vehicle injuries to people happened to those not in cars but while walking, running or hiking, so one needs to be safe. In fact, over 4,000 walkers or runners were fatally hit by a motor vehicle according to the Centers for Disease Control (CDC). These statistics continue to increase as the number of distractions to drivers increases (phone calls, texts, etc). Consequently, walkers, runners and cyclists must be more aware than ever to prevent injury from motor vehicles and stay safe.
Source: http://www.runnersworld.com
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

Have you ever noticed high level athletes warming up before a game or competition walking or running backwards? You may also see fitness enthusiasts in gyms emulating these athletes to improve their fitness or performance. I found the concept of backward walking, (also called retro walking) interesting and decided to research the topic for more information and validation. Walking backward does have many therapeutic benefits, however, before you attempt this activity on a treadmill or elliptical, please consult your physician and physical therapist and have a spotter nearby.
At a recent meeting of The American College of Sports Medicine, several studies were presented on the topic of backward waking. Most of the research was conducted while moving backward on a treadmill and an elliptical machine. When comparing two groups recovering from knee injuries, the backward motion group showed significant improvement in strength in the quadriceps (front thigh) and hamstring (back thigh) muscles when compared to the traditional forward walking group. Furthermore, the muscles of the front (tibialis anterior) and back (gastro/achilles) of the shin/ankle also demonstrated an increase in strength and endurance with backward walking. One explanation is that forward motion is routine in daily living that it has become very efficient and does not tax or stress the muscles the body. While this efficiency prevents fatigue in daily activities, it may not stress the muscles enough to gain strength as quickly as an unfamiliar exercise.
Due in great part to the increased strain of performing an unfamiliar exercise, backward walking on a treadmill or backward pedaling on an elliptical, offered a greater cardiovascular benefit and caloric expenditure than forward motion at all levels. Specifically, walking backward on a treadmill at 2.5 mph at grades of 5% - 10% has been found to significantly increase cardiovascular endurance than walking forward under the same conditions. This knowledge is useful for healthy individuals in need of greater cardio exercise. However, it may also serve as a precaution for those with cardio problems and should consult their physician prior to engaging in this activity.
A recent study in the International Journal of Obesity, found that those who performed new activities or increased the intensity of an activity, even if for a short duration (interval training) expended more energy and burned more calories than those who worked out at the same pace consistently for a longer duration. Moreover, when engaging in a new activity such as backward walking, even more calories were burned. This phenomenon may be due to the fact that routine activities such as forward walking are performed more efficiently and easily.
We challenge our body when we inefficiently perform a new motor skill such as backward walking and burn more calories. In other words, if you want to burn more calories without exercising for longer periods of time, than try a new activity and engage in higher intensity, intermittently, for part of the time. For example, walk backward on the treadmill for 30 minutes at 2.5 mph, but do so at a 5 – 10% incline for 1-2 minutes every 5 minutes.
Some studies show that using other muscle groups by performing different exercises not only prevents boredom, but also protects your muscles and tendons from overuse and joints from wear and tear. Specifically, the knee joint and the patella joint (the joint where the knee cap glides on the knee), benefits from backward walking due to less stress and compression forces on the joint. The thigh and ankle/foot muscles benefit from using a different form of contraction while lengthening the muscle. Some authors propose that this may also prevent strains and pulls and may be valuable to strengthen those with a history of shin splints and flat feet (pronation).
Mixing up your program prevents boredom. As a rule, those willing to change their exercise routine are more compliant and continue to exercise longer than those stuck in the same routine. A new challenge to improve distance, speed, and resistance while exercising in a different direction will be refreshing to your program.
Prevention of falls by improvement in balance and coordination has received a great deal of attention in the past few years. This is not only valuable to the athlete but may be even more important to those over 50. With age, balance centers are slow to react to changes in inclination, elevation, rotation and lateral movements. This slow reaction time leads to falls that may cause fractures, head injuries and more. Working on this problem by challenging the vestibular and balance centers before it is seriously compromised is important and backward walking is one way for this to be effectively accomplished.

Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

As summer fads and cool fall nights are upon us, many of us will prepare to put away some of our warm weather toys…closing the pool, storing kayaks and boats and packing up the “slip and slide.” However, one activity that can last well into the fresh breeze of fall is cycling. In fact, many feel that fall is the best time of year to jump on a bike and enjoy the ride! If you are looking for a kick start to riding your bike this fall, consider the 20th and final Tour de Scranton on Sunday, April 15, 2024. It is a fun-filled, noncompetitive bike ride through Scranton and neighboring communities. Tom and Betty Moreken, with the help of dedicated friends and countless supporters have raised over $400,000.00 to benefit addiction treatment and prevention in honor of their daughter Erin, a victim of drug addiction. I have had the privilege to know Tom and Betty and have always admired their resilience and selflessness to turn a negative into a positive and do something good for others. They and their friends truly represent everything that is good about the people of NEPA!
So dust off your bikes and join the fun at Tour de Scranton. Hopefully, it will entice you to ride the many beautiful and well-maintained trails that are available at the Countryside Conservancy and other locations in the Abingtons and the Lackawanna Heritage Valley Authority.
Tour de Scranton is the official “kick off” to biking season in NEPA. This year, on Sunday, September 15th, the 20th annual and final Tour de Scranton will offer a selection of several routes and distances for the novice and experienced rider at its non-competitive bike ride for riders of every age and skill level. This event supports “The Erin Jessica Moreken Drug & Alcohol Treatment Fund” which provides charitable gifts to qualified local organizations or individuals struggling with the disease of addiction. For more information visit: www.tourdescranton.com.
There are many obvious reasons to bike…cardiovascular fitness, burn calories, improve leg strength and others. But, the real question is, “what are the advantages of biking over other forms of exercise?” Glad you asked…
Prevention is the best management of musculoskeletal problems associated with biking. First, many of the problems associated with biking such as knee pain, buttock soreness, and tendonitis can be prevented through proper fitting. Furthermore, it is important that your equipment be in good working order such as tires, chain, brakes and pedals. Next, be sure to maintain a fairly good fitness level in order to bike safely. If you are a beginner, start slowly. Warm up and slowly bike for 10 to 15 minutes and build up over time. Practice the coordination of stopping, starting, shifting and braking. Work on good strength and flexibility of the hamstrings, quadriceps, calves and gluteal muscles. All of these muscles are necessary to generate pedal force. Balance is also important to safety and can be practiced on and off the bike. Be aware that adaptive equipment can modify your bike for added comfort and safety such as soft handlebar tape, seat post and front fork shock absorbers, padded biking shorts, c-out and gel pad saddle seats, and wider tires.
Be careful not to progress too quickly because inactivity to over activity in a short period of time can create problems. Overuse injuries such as tendonitis, can be avoided by cross training. Bike every other day and walk, run or swim on off days. Make sure to take time off to recover after a long ride. Use ice and massage to sore muscles and joints after riding.
Remember, cycling should be fun! Pain from improperly fitted and poorly maintained equipment is preventable. Excessive workouts and training rides should be kept to a minimum and consider cross-training in between.
EQUIPMENT: Helmets are a must! Also, keep your bike in good condition. Road bikes should have mirrors and reflectors. Use hand signals and obey traffic rules. Dress for weather and visibility. Have a first aid and tire patch kit, tire pump and tools. Seat comfort can be improved with gel cushion or split seat.
BE ALERT: for traffic, parked cars, pedestrians loose gravel and cracks in the road.
SOURCES: American Physical Therapy Association
Visit your doctor regularly and listen to your body.
Keep moving, eat healthy foods, and exercise regularly

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

“When is it safe for my child to start weight training?” This is a very common question asked by parents of young athletes who are looking for advice regarding their children’s participation in weight training. This month, for example, I received three such inquiries. While some who are eager to get a “competitive edge” may not be satisfied with the answer, these recommendations are grounded in the scientific literature and medical specialist with the hope to prevent injury and dispel fear and fallacy.
Weight training, weight lifting or resistive training all describes the use of a resistive force on a muscle to improve strength. While much attention has been given to the benefits of weight training in adults, much less has been written about its application in children.
According to the Journal of Pediatric Orthopedics, children less than 12 years old are considered prepubescent or before puberty. Teenagers who are between 12 and 19 are considered to be adolescents. Studies consistently demonstrate that strength gains are much more significant in adolescents than in preadolescents. It is important to note that these strength gains are not only from the enlargement of muscle fibers (hypertrophy), but also from the improvement in the coordination and efficiency in muscle contraction and the recruitment of motor units and fibers within the muscle.
Preadolescents lack the hormones necessary to develop masculine characteristics. Adolescents begin to produce the hormones of testosterone and androsterone to develop secondary sexual characteristics such as pubic hair and enlarged genitalia. In view of this, age 13-14 is the optimal age to safely begin and benefit from a well-designed weight training program.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

While many people celebrate the Labor Day holiday by firing up the grill, others will be shopping to get their students ready for the school year. One item on the shopping list should be a good quality and well-fitted backpack…to prevent lower back pain!
In 2018, the government of India announced a ban on homework and recently in Poland; the government ministers did the same. Can you imagine…a ban on homework? In an effort to promote student health and address recent surges in the incidence of back pain in the young, there will be no homework for students in grades one and two.
It was estimated that the majority of students ages 7 – 13 in India were carrying almost half their body weight. Not surprisingly, medical practitioners noticed a dramatic increase in reported cases of back pain among this group and decided to take action. In addition to the homework ban for grades one and two, Indian authorities have also implemented a limit of 10% of the student’s body weight.
Back pain in students seems to be universal. Each year, as students in the United States prepare to return to school from summer vacation, the subject of backpacks arises. The good news: when compared to purses, messenger bags, or shoulder bags, backpacks are the best option to prevent lower back pain. The bad news is, most of the 40 million students in the USA using backpacks, are doing so incorrectly.
Studies have found more than 33% of children had LBP that caused them to miss school, visit a doctor, or abstain from activity. Also, 55% of children surveyed carried backpacks heavier than the 10-15% of their body weight, which is the maximum weight recommended by experts. Additionally, the study noted that early onset of LBP leads to greater likelihood of recurrent or chronic problems. Backpacks that are too heavy are particularly harmful to the development of the musculoskeletal system of growing youngsters. It can lead to poor posture that may lead to chronic problems.
The following information on backpack safely is based, in part, by guidelines from The American Physical Therapy Association. Parents and teachers would be wise to observe the following warning signs of an overloaded and unsafe backpack:
Consider the following suggestions to promote backpack safely and prevent back injury:

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy in Scranton and Clarks Summit. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!
