Lung Cancer is a deadly disease. Until recently, a chest X-ray, often used only after patients developed symptoms, discovered the disease when it was in its late stages. Over the past few years, however, an effective and safe screening test has been developed and those who are at high risk for lung cancer can now be screened annually using low-dose spiral CT scans.
FACT 1: Each year over 250,000 people in the United States are newly diagnosed with lung cancer.
FACT 2: 90% of individuals who have lung cancer will eventually die of the disease, making lung cancer the most deadly cancer in the United States for both men and women.
FACTS 3: 85% of all lung cancers are caused by smoking.
FACT 4: According to the Pennsylvania Department of Health, 22% of people aged 18 years and older residing in Northeastern, PA smoke.
FACT 5: The best prevention measures are; not smoking or using tobacco products, and avoid second-hand smoke or high air pollution environments.
One of the reasons for the high mortality rate in lung cancer is that the disease is often not discovered until it is advanced and treatment options are limited. Some of the most common signs and symptoms of lung cancer are easily mistaken either for a mild illness or for things such as “smoker’s cough”. By the time many patients are diagnosed, their disease is advanced and may involve lymph nodes or other organs.
For some cancers, there are established screening tests that help to identify these cancers at an earlier stage. For example, routine screenings through colonoscopies, mammograms, and pap smears are well established and have saved thousands of lives. Historically, lung cancer has not had such a screening test. This however, is about to change. This past summer, the United States Preventative Task Force (USPTF), an independent committee charged by congress to evaluate the most current data and make recommendations for disease screening, released a draft of a new proposal for a lung cancer screening test.
The USPTF now recommends that all persons who are at high risk for lung cancer should be screened annually using low-dose spiral CT scans. High risk persons are identified as those who are between the ages of 55 and 79, who have a history of 30 pack years or more of smoking, and who are either still smoking or who have quit within the last 15 years. A “pack year” is defined as smoking 1 pack of cigarettes a day for a year. For example, a person could have 30 pack years of smoking if they smoke 1 pack of cigarettes a day for 30 years. Similarly, they could have a 30 pack year history by smoking 2 packs of cigarettes a day for 15 years.
CT, or computed tomography, scans are a form of three-dimensional imaging used by clinicians to visualize the organs and other anatomy of patients. The scan can detect abnormalities on a patient’s lung with much earlier and with greater sensitivity than an x-ray. Much like a mammogram, low-dose CT scans do not diagnose cancer but are a way to identify patients with abnormalities that need to be investigated further for the possibility of cancer. This new screening test will allow physicians to see possibly cancerous abnormalities of the lung before the disease can spread and become impossible to cure. The scan is non-invasive and generally considered very safe. Low-dose CT scans carry about 5 times less radiation than traditional high-dose CT scans and are equivalent to about 15 x-rays.
It is projected that this new screening practice will save the lives of between 15 and 20% of those diagnosed with lung cancer by detecting cancers before they can progress to the point that they are resistant to medical treatment. The draft of the new proposal for lung cancer screening that the USPTF released this summer was based off of a landmark article in The New England Journal of Medicine in 2011. Once the final document is published, clinicians will be encouraged to adopt these screening practices and insurance companies will use these recommendations to adopt their policies regarding coverage for testing.
While this screening is a major step in the detection and treatment of lung cancer, it is not a substitute for quitting smoking. The best proven methods to prevent lung cancer and its deadly consequences is to not smoke, use other tobacco products, and avoid exposure to second-hand smoke.
If you or a loved one need help quitting tobacco products, you may contact your physician or call 1-800-QUIT-NOW or visit www.lung.org. For more information on the new lung cancer screening guidelines visit: www.cdc.gov
NOTE: These signs and symptoms can be attributed to many different causes and are not exclusive to lung cancer. Always discuss your symptoms with your physician.
Patients who fit all of the below criteria:
*A pack year is defined as 1 pack of cigarettes per day for a year
Medical Contributor: Sarah Bashaw, MD is a graduate of TCMC (presently GCSOM).
Medical Reviewer: Greg Cali, DO, Pulmonologist, Dunmore, PA

Read “Health & Exercise Forum” – Every Monday. This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit: mackareyphysicaltherapy.com/forum/
Most people know that some medicines don’t work well together. However, many may not be aware that what you eat and drink can have an effect on some drugs, too. Natural herbal supplements and other over the counter drugs can also have serious interactions with your prescribed medications. So, it might be wise to talk with your physician or pharmacist to see if there’s anything you should stay away from before you take a medication for the first time.
This otherwise benign citrus fruit changes the way certain cells in your gut break down and metabolize medication through your body -- it can affect more than 50 drugs. It can make some, like fexofenadine (Allegra) for allergies, less effective and make others too strong, including ones that lower your cholesterol like atorvastatin (Lipitor).
Some dairy products, like milk, can make it harder for your body to process certain antibiotics. Minerals in milk like calcium and magnesium are part of the reason, along with the protein casein. If you’re taking antibiotics, ask your physician or pharmacist about the foods or beverages you should stay away from.
Licorice is a popular herbal remedy for digestion and to flavor foods. But glycyrrhizin, a chemical in licorice, can weaken the effect of some drugs, including cyclosporine, used to keep people who’ve had transplants from rejecting their new organs.
According to sources at WebMD, dark chocolate can weaken the effects of drugs meant to calm you down or make you sleep, like zolpidem tartrate (Ambien). It also can boost the power of some stimulant drugs, like methylphenidate (Ritalin). And if you take an MAO inhibitor, used to treat depression, it can make your blood pressure dangerously high.
Alcohol can make certain drugs less effective or even useless, including some blood pressure and heart medicines. It also can make others stronger than they should be or cause dangerous side effects.
Coffee, while typically enjoyable and harmless, contains caffeine which can affect the levels of antipsychotic drugs like lithium and clozapine. It can also but boost the effects (and side effects) of other drugs such as: aspirin, epinephrine (used to treat serious allergic reactions), and albuterol (taken by inhaler for breathing problems). Additionally, it can make it harder for your body to take in and use iron.
Iron supplements can lower the effects of levothyroxine (Synthroid), a medicine that gives you thyroid hormone when your body doesn’t make enough (a condition called hypothyroidism). If you take this medication and a multivitamin, check to see if the vitamin has iron in it. If you need an iron supplement, ask your physician or pharmacist if you can take your medication at different times.
These drugs help with the sneezing and runny nose caused by allergies and are in most cases safe to use. However, when they are combined with other medications it can make blood pressure medications less effective and raise your heart rate. Talk to your physician or pharmacist about other ways to manage your allergies if you take blood pressure medicine safely and effectively.
Vitamin K is the antidote to reverse anticoagulation. So, if you take the drug warfarin, (Coumadin) which is used to treat and prevent blood clots, be aware of how much vitamin K you take in. It can make the blood thinning drug less effective and put you at higher risk of a dangerous blood clot. Broccoli, Brussels sprouts, kale, parsley, and spinach are some of the most common foods high in vitamin K. Try to eat the same amount of these foods every day so the level of warfarin in your blood stays the same.
Ginseng, can also lower the effects of warfarin (Coumadin), putting you at risk for blood clots. And it can make you more likely to have internal bleeding, especially if you take antiplatelet medications (blood thinners) such as heparin or aspirin, as well as nonsteroidal anti-inflammatory drugs like ibuprofen or naproxen. For those who take MAO inhibitors, ginseng can cause headaches, sleep problems, hyperactivity, and nervousness.
While taken by many people with depression, this herbal remedy has not been a proven treatment for that, or any other health condition and it is not benign It increases the action of specific liver enzymes (things that boost certain chemical reactions in your body) that can weaken some medications. Those include cholesterol drugs (Lovastatin and Mevacor), the erectile dysfunction drug sildenafil (Viagra), and digoxin (Lanoxin), used to treat certain heart conditions. These are just a few of the many medications St. John’s Wort can affect.
As with St. John’s Wort, while used by many to help with or prevent high blood pressure, dementia, ringing in the ears (tinnitus), and other conditions, there is no research that supports its value. It can weaken the effect of drugs used to control seizures, including carbamazepine (Tegretol), and valproic acid (Depakote). Ginkgo biloba also has natural blood thinning properties that can increase your risk of bleeding, especially if taken with other blood thinning medications such as aspirin, ibuprofen, warfarin (Coumadin) and clopidogrel (Plavix).
According to WebMD, only about 50% of medication is taken as it’s prescribed. People often take less than they need, take it at random times, or leave big gaps between doses -- all of which can weaken the effects. Make sure you understand your treatment plan and follow your physicians instructions. Moreover, the use of some supplements, as well as what you eat and drink, may have a serious impact on the safety and efficacy of your medications…when in doubt; ask your physician or pharmacist!
Sources: WebMD; National Institutes of Health
Guest Contributor: Dr. Carina Mackarey Pharm.D. is a doctor of pharmacy and clinical pharmacist at Wilkes-Barre VA and Primecare Pharmacy Services in Scranton.

Read Dr. Mackarey’s Health & Exercise Forum – Every Monday
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
For all of Dr. Mackarey's articles visit mackareyphysicaltherapy.com/forum/
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine.
A routine visit to your primary care physician can be overwhelming. In addition to countless forms about insurance and privacy, endless questions about your medical history can be exhausting. A plethora of questions about your medical history is followed up by the health conditions of your closest relatives. While it may seem intrusive and laborious, the health conditions of your parents, grandparents, siblings, aunts and uncles can help them know what to be on the lookout for with you. For example, if your mother has high blood pressure, they might want to keep a closer eye on yours. Both nature (your genes) and nurture (your family’s lifestyle) can have an effect on your health -- and you get both from your parents.
It is important to disclose any ongoing conditions (like diabetes or asthma) or serious illnesses (like cancer or a stroke) your parents, grandparents, and siblings have or had and how old they were when the health problem started. If any of them have passed away, let your doctor know their cause of death and how old they were when they died. They also may ask about things like your family’s lifestyle or diet, because relatives tend to have these in common.
Just because a close relative had a certain condition or illness, that doesn’t necessarily mean you will have it. However, your chances are slightly higher than other people’s. Some health issues that can be passed down include:
Ethnicity refers to the cultures, customs and lifestyle choices of certain groups more than in the general population. Your doctor may ask about your race because people who have roots in certain parts of the world are more likely to have some conditions. For example, African-Americans have a higher chance of having sickle cell anemia and high blood pressure, Caucasians have a higher incidence of cystic fibrosis and Jewish people from Eastern Europe are more likely to carry the BRCA gene mutation and be born with Tay-Sachs disease.
Many people do not know much about their family medical history for a variety of reasons. If possible, ask your closest relatives about their health and the health of other family members such as; aunts, uncles, or cousins. If you’re lucky someone may have kept a family tree, baby books, or other keepsakes that could be of value. If that doesn’t work, there are other options in an internet age;
The U.S. Surgeon General’s office has an easy way for you to collect this kind of information. It’s called My Family Health Portrait. It helps you make a kind of family medical tree that you can share with relatives and download to take to your doctor.
Information about your relatives can often be found in death certificates or medical records such as age at death, cause of death, and ethnic background. The rules are different for each state, but close family members are often allowed to order copies of these. Obituaries, which are often posted online, may also have some information.
For those who don’t know much about your relatives and don’t have time to research it on your own, there are companies that can help fill out your family tree. Once you know the names of your relatives, you can try to contact them or find obituaries or death certificates.
For some, it may be helpful or necessary to have genetic or DNA testing performed. A conversation with your primary care physician will help make an informed decision.
Not everyone will be able to provide a thorough and comprehensive medical history for their physician. For example, adopted children or those who lost parents at an early age often lack access to a strong family history. Do your best to talk to your doctor about the information you do have or tell them that you don’t know much about your family health history. They can help you sort through it and maybe even tell you where else to look. Even if you’re missing some facts, any information you have can be useful.
SOURCES: WebMD; National Institutes of Health

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
For all of Dr. Mackarey's articles visit: https://mackareyphysicaltherapy.com/forum/
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM
October is National Physical Therapy Month. The American Physical Therapy Association (APTA) would like the nation to recognize the positive role physical therapy plays in your health and wellness. We are passionate about what we do! No, we don’t save lives, but we do save lifestyles and quality of life! PT’s are great people. We have a special gift to provide healthcare unique to our field. For example, while many different health care professionals treat back pain, PT’s are some of the very few working to rehabilitate stroke and head injury victims, amputees, children with cerebral palsy and other serious neurological and orthopedic disorders.
In honor of physical therapy month and the thousands of dedicated physical therapists working hard to keep you healthy and mobile, I would like to share some health and wellness pearls of wisdom.
Remember, we cannot control our gene pool or what happens to our bodies, however, we can control our lifestyles. Research suggests that lifestyle may play the biggest role on how healthy you are and how long you live. The food you eat, what you drink, if you smoke, how active you are and how you handle stress are critical factors that determine your longevity. Research also tells us that smoking, physical inactivity, and poor eating habits are the leading causes of death, in that order.
One, to be truly healthy, one must have a health mind, body and spirit. A healthy mind requires education and intellectual stimulation. The body requires a good diet and physical activity while the spirit thrives on faith and hope. Strive to find balance and address all three elements of health and wellness.
Two, keep it simple. Should I walk, run, swim, or ride? Do I use free weights, barbells, rubber tubing or lifting machines at a gym? The answer is KEEP IT SIMPLE! You don’t need to join an expensive gym with a personal trainer to get in shape. Bands, light dumbbells, walking at the mall, and biking will all get you in shape. It must be convenient and consistent. Physical activity is one of the most important factors in improving a lifestyle in a positive way. But, it does not have to be complicated. A minimum of 30-45 minutes of physical activity, 3-5 days per week will have many positive effects on your body. But, the studies also show that engaging in 10-15 minutes of activity 2-3 times per day, is also valuable to your health…even at work!
Three, be realistic. Expect that exercise will take time to have a noticeable benefit. Don’t get overly ambitious and set yourself up for failure.
Four, be religious. Be religious about exercise and diet but don’t get too compulsive. Studies show if you are too compulsive, you will probably not keep it up for life.
Five, ask a professional. There are a million misconceptions about health and fitness. For example, some people still think you can spot reduce! Ask a professional, (medical doctor, physical therapist, nutritionist, exercise physiologist), if you have a question about beginning a diet or exercise program. If you have health issues or concerns, see your primary care physician first.
Six, there is no secret to a long and healthy life. According to the National Institutes of Health (NIH), while genes play an important role, lifestyle plays the biggest role on how healthy you are and how long you live. The food you eat, what you drink, if you smoke, how active you are and how you handle stress are critical factors that determine your longevity. The NIH research has found that smoking, physical inactivity, and poor eating habits are the leading causes of death, in that order.
Seven, find a fitness mentor or role model. I have the good fortune of meeting many patients over the years that serve as my health & fitness role models. I continue to be inspired by those who overcome their disabilities and injuries through hard work and determination to regain health, wellness and function. Find someone who inspires you!
Eight, find a spiritual mentor or role model. Learn a lesson from “the greatest generation.” The WWII generation rarely complained, worked hard and placed great emphasis on God and responsibility to family. Try to associate with people whose “glass of water is always half full.”
Nine, do the right thing. When it comes to exercise, do the right thing. Get good advice, wear the appropriate clothing and shoes and eat and drink appropriately for the activity. Walk and run in running shoes, eat plenty of whole grains, fruits and vegetables with a good balance of protein and carbohydrates. Drink plenty of water before and during endurance activities. Make proper adjustments for different temperatures.
Ten, have FUN! A healthy lifestyle doesn’t have to be drudgery. There are plenty of good and flavorful healthy food choices. An occasional cheat is good. Also, there are plenty of fun activities and exercise options. Run, walk, swim, bike, hike a canyon, cross-country ski, downhill ski. Use the elliptical, recumbent bike, or stairmaster, recumbent stepper. Alternate routines, cross-train, or play a sport like tennis, golf (walk the course), racquetball or squash. Mix it up. IF YOU WANT TO EXERCISE FOR LIFE - YOU MUST HAVE FUN!

Read Dr. Mackarey’s Health & Exercise Forum – Every Monday
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
For all of Dr. Mackarey's articles visit: https://mackareyphysicaltherapy.com/forum/
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine.
October is National Breast Cancer Awareness Month and there is good news to report!
A recent study in the Journal of the American Medical Association from Harvard has found that regular exercise can improve the survival of patients with breast cancer. I have discussed these findings with local physician, Dr. Christopher Peters of Northeast Radiation Oncology Center and he says that he regularly councils his patients about the value of exercise in the recovery from breast cancer. As found in the study, he recommends aerobic exercise such as walking and/or biking and mild resistance exercise. He also encourages patients to enroll in a formal rehabilitation program, especially to prevent a frozen shoulder if invasive surgery was performed.
Previous studies have shown many benefits of exercise for breast cancer patients including improving immune functioning and controlling depression. However, new research recently presented at the American Association for Cancer Research annual meeting was the first report to conclude that physical exercise may improve survival in breast cancer patients. Additional studies have shown other benefits of exercise. For example, a study conducted at Vanderbilt University found that women who had high activity levels throughout life were less likely to develop endometrial cancer. At the Hutchinson Cancer Research Center in Seattle, researchers found that exercise with moderate intensity can reduce serum markers of inflammation (C-reactive protein), which, when elevated, are associated with chronic disease and poor cancer survival.
In the current study, conducted at Harvard University, researchers compared survival rates in women with breast cancer with exercise levels in terms of metabolic equivalent (MET) hours per week. While women with high activity levels of exercise had the best outcomes, even women with moderate exercise benefited.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
Back to school also means back to sports. Countless students are participating in tennis, soccer, cross country running, gymnastics, and other sports. These student athletes and others who engage in recreational sports and exercise can be vulnerable to excessive training for all the right and wrong reasons. Parents, family members, coaches, teachers, athletic trainers, friends and health providers must be aware of potential for exercise abuse…as part of the “fitspiration” movement.
It takes only a cursory glance through social media to become aware of the “fitspiration” movement. This catchy term may accompany posts of workout videos, pictures depicting physical activity, or pictures of individuals showing off the muscular bodies they obtained through dedication to rigorous exercise regimens. In a sense, exercise and fitness have become trendy in our society, with more strenuous exercise routines being perceived as more impressive. Cars boast bumper stickers with numbers such as “13.1,” “26.2,” or even “50,” referring to the distances so proudly conquered by runners. When we hear a friend has decided to commit to a rigid training schedule to complete a marathon, we are often in awe of their self-control and motivation, wishing we were that dedicated. But can exercise be a bad thing? The answer is complicated. Exercise is one of the best things we can do for our health. I have heard physicians say that if all the benefits of exercise could be bottled up into a pill; pharmaceutical companies would be fighting for the chance to sell it. However, it can get complicated when one’s reasons for exercising stem from a potentially destructive place, rather than a pursuit of health.
Exercise bulimia is a term used to refer to the excessive use of exercise to burn calories or try to keep a low body weight. It is not a medical diagnosis in and of itself, but the notion of using exercise to make up for excessive calorie consumption or maintain an unhealthily low body weight can occur in both anorexia nervosa and bulimia nervosa. Moreover, when excessive exercise occurs in combination with a significantly low body weight, an intense fear of gaining weight, a disturbed body image, undue influence of body shape on self-worth, or a failure to recognize the seriousness of the condition, an individual would meet the criteria for anorexia nervosa.
Anorexia nervosa can cause serious complications in all body systems. Some examples include disrupted functioning of the heart, reduced lung capacity, hormonal imbalance, amenorrhea, (loss of the menstrual period in women), changes in brain structure, and in severe cases, difficulty with memory. The hormonal changes associated with amenorrhea, especially when coupled with extreme exercise, can lead to reduced bone density and can put women at high risk of stress fractures. Stress fractures are breaks in the bone that occur from overuse through large amounts of exercise rather than the traumatic bone breaks we typically think of where an obvious event results in a broken bone.
Because exercise bulimia can be a part of an eating disorder with potentially life-threatening consequences, it is important to be aware of the warning signs that someone’s exercise routine might be part of an eating disorder. Signs of exercise bulimia may include:
While the definition of exercise bulimia implies a voluntary engagement in excessive exercise for weight loss, my experience from being on female track and cross country teams in high school and college has shown me that anorexia nervosa does not always fit the mental picture we may have of someone who refuses to eat at all or even of exercise bulimia where an individual compulsively engages in excessive exercise. During cross country, the mileage we ran likely would have been considered excessive by the average person. Our team often trained 7 days a week with run-length ranging from 5-12 miles. Most runs were at least 7 miles, and some of my teammates had long runs in excess of 12 miles. The men on our team ran even farther. In hindsight, one of my teammates may have met the criteria for a diagnosis of anorexia nervosa. Her weight was significantly below normal, she feared weight gain, did not eat sufficient calories to replenish what she burned on runs, and despite knowing she was thin, did not fully recognize the potential health consequences due to her low weight. However, it was not a clear cut problem. She was not an obvious candidate for an eating disorder because she was not pursuing the excessive exercise; she was simply following her coach’s training plan. If she did not exercise to the extent she did, the amount of food she ate would have been considered normal, so seeing her eating habits alone did not trigger any red flags. Finally, cross country runners are known for being lean, often even emaciated; it was a common side effect of the sport often not given a second thought. Thankfully, this runner never fell victim to the dangerous downward spiral that is sometimes seen in patients with anorexia nervosa. However, it is important to be aware of the unsuspecting ways in which an eating disorder can sometimes present.
Treatment of eating disorders typically involves a multi-pronged approach with nutritional counseling, psychotherapy, and general medical care playing a role. The nutritional counseling aims to help the patient restore a healthy diet to attain a healthy weight, the psychotherapy aims at getting to the root of the issues that may have contributed to the onset of the eating disorder, and general medical care may be necessary to manage any complications from the eating disorder depending on its seriousness. Educational programs about eating disorders and risk factors have also been shown to be successful in helping to prevent eating disorders.
It can sometimes be a fine line between a healthy passion for exercising and eating well and the start of an eating disorder. Especially in athletes where extreme exercise is part of the sport and putting in extra training is rewarded, it is valuable to be aware of the signs and symptoms of exercise bulimia to help prevent a loved one from crossing over that line. Though serious health consequences are possible in the setting of an eating disorder, treatment and recovery are very possible.
For More Information: www.nationaleatingdisorders.org
GCSOM Guest Author: Mary Pelkowski, MD4 is a student in the Geisinger Commonwealth School of Medicine MD Class of 2022. She grew up in Sayre, PA and graduated from Notre Dame High School. She received her undergraduate degree in biology with a minor in chemistry from Saint John Fisher College in Rochester, NY.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
For all of Dr. Mackarey's articles visit: https://mackareyphysicaltherapy.com/forum/
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
82 million adults spend an estimated 28 billion dollars on gym memberships each year! WHY? There are many reasons we exercise. Some people exercise to prevent illness such as cardiovascular disease or osteoporosis. Others exercise for mental health and as a stress release; others do it to improve strength, flexibility, and endurance to prepare for a sport. However, the number one reason people exercise is TO LOOSE WEIGHT!
When it comes to losing weight, patients have asked me a wide variety of questions over the years. However, certain questions are consistent. “What exercise is the best to burn calories?” “Even though I exercise 2-3 times per week, why can’t I lose weight?” “What is BMR?” “If I eat a Snickers bar, how much exercise do I need to do to burn it off?” “Are there any tools that I can use to help me track my calories and exercise output?”
Have you ever heard people say that they never felt better or burned more calories as they did when they ran? Well, they may be right! The following numbers are based on the average male weighing 150 pounds: running 6 miles per hour will burn 700+ calories (11-12 calories per minute); vigorously skipping with jump rope or fast cycling will do the same; vigorous walking at 4 miles per hour and moderate biking will burn 600+ calories (10 calories per minute). The 400-500 calorie club includes the following activities: slow jogging, swimming, football, basketball, baseball, tennis, skiing, and moderate walking (3.5 miles per hour). Light gardening burns more calories than golfing using a cart (250 vs. 180).
How many times have you heard people say, “It is hard for me to lose weight because I have a slow metabolism?” What does that mean? To explain this in detail you first must understand BMR. BMR is basic metabolic rate. It is the number of calories that your body requires to operate basic body functions that you don actively control, such as continuing to breathe, and keep your cells and organs working each day. The BMR is influenced by age, height, gender, body fat, and fitness level. BMR is inherently different (high or low) in each individual. While you can’t change your gender or height, you can influence some things to influence your BMR and burn more calories at rest. One, exercise for longer durations, with greater intensity and more frequently. Two, lower your body fat by eating less calories, especially fat and carbohydrates in your diet. Simply, eat less calories than you burn! Three, improve you muscle/fat ratio by weight training.
BMI: < 18.5 = Underweight
BMI: 18.5 – 24.5 = Normal Weight
BMI: 25. - 29.9 = Overweight
BMI: >30. = Obestiy
For example, I am a 57 year old male, weighing 150 pounds at 5 feet 8 inches tall with a BMI of 22.8
*Calculate you BMI by entering you gender, height and weight and find how many calories per food item at:
There are several tools available for free online to help with tracking calories and exercise visit Prevention Magazine at: www.myfooddiary.com or try the App “Lose It”
BMI Calculator – to calculate your BMI
Calorie Burner – to calculate how many calories are burned with various activities
Daily Calorie Calculator – Find how many calories are in specific foods and what you need to do to loose or gain weight.
So remember, the number one reason we exercise is TO LOSE WEIGHT! But depending on exercise alone to lose weight is an exercise in futility. Losing weight is an intelligent and consistent combination of a balanced diet with portion control, proper nutrition, adequate exercise and activity grounded in lifestyle changes.

Read Dr. Mackarey’s Health & Exercise Forum – every Monday
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
A patient recently asked me if it is safe to take the Moderna, Pfizer-BioNTech, or J&J COVID-19 vaccine during pregnancy? While this is far outside my area of expertise, I took the opportunity to research the matter further and discuss the findings with local pediatricians, Dr Anders Nelson and Dr. Stanley Blondek. They are both strong supporters of vaccinating nursing mothers.
According to the CDC, no safety concerns were found in animal studies: Studies in animals receiving a Moderna, Pfizer-BioNTech, or Johnson & Johnson (J&J)/Janssen COVID-19 vaccine before or during pregnancy found no safety concerns in pregnant animals or their babies. Human studies supported these findings. In fact, in one study, vaccine-generated antibodies were also present in all umbilical cord blood and breast milk samples taken from the study, showing the transfer of antibodies from mothers to newborns.
Moreover, in humans, in the largest study of its kind to date, researchers at Massachusetts General Hospital (MGH), Brigham and Women’s Hospital and the Ragon Institute of MGH, MIT and Harvard have found the new mRNA COVID-19 vaccines to be highly effective in producing antibodies against the SARS-CoV-2 virus in pregnant and lactating women. The study also demonstrated the vaccines confer protective immunity to newborns through breast milk and the placenta.
Long before COVID-19, breastfeeding has always demonstrated many benefits for both mother and child. Expectant mothers typically do all they can to ensure their baby’s health. A wholesome diet, regular exercise and avoiding harmful habits like smoking are all important things a woman should do during pregnancy. However, there is something additional mothers can do AFTER their child’s birth that can be equally, if not more, important and has been around as long as human life itself… breastfeed! While far from new, it is has been rediscovered for it tremendous benefits and gaining popularity.
Nursing your baby immediately after birth helps solidify the bond between you and your baby. Moreover, the health benefits to baby begin right away. That’s because your breasts produce colostrum beginning during pregnancy and continuing through the early days of breastfeeding. Colostrum precedes breast milk and has plenty of antibodies to help keep your baby healthy. Colostrum is extremely easy to digest, and is therefore the perfect first food for your baby. Also, as the La Leche League (LLL) tells new mothers, “Colostrum has a laxative effect on the baby, helping him pass his early stools, which aids in the excretion of excess bilirubin and helps prevent jaundice.” Jaundice is common in newborns and is usually treated by placing the baby under special lights. LLL also points out that the concentration of immune factors is much higher in colostrum than in mature milk, which comes in after about two weeks.
The positive effects continue for both mother and baby as the child grows from newborn to infant. Breast-fed babies are, for example, less prone to sudden infant death syndrome (SIDS), an unexplained death of a healthy infant while sleeping. The peak incidence of SIDS occurs when a baby is about three months old. It is an unspeakable tragedy that affects entire families. While we must be very clear that breastfeeding is not a guarantee against SIDS, newer studies have shown that infants who were never breastfed may have two to three times the risk of dying of SIDS. Although the actual mechanism is unknown, some theories are that breastfeeding may provide defense against SIDS because it lowers a baby’s risk of infection through antibodies passed on by mom or because human milk is ideally equipped to nurture human brains -- and the brain controls sleep cycles.
Are there ever reasons why either mother or baby should not breastfeed? While extremely unusual, there are contraindications for breastfeeding. Mothers who must take certain medicines may be unable to nurse. There are also some conditions in newborns – some treatable – that may limit or prevent breastfeeding. Your physician (obstetrician/gynecologist or pediatrician) or midwife should be consulted before you take any medications, vitamins or herbals.
It is recommended that you exclusively breastfeed your baby for the first six months and continue for at least the first year. After that, it’s up to you. It’s also important to know that every baby is a unique individual. Don’t become alarmed if your child doesn’t seem to adhere to what the textbooks say. Instead, turn for support to some reliable and trustworthy: your physician, midwife and the La Leche League.
SOURCES: Le Leche League is an international nonprofit organization that distributes information on and promotes breastfeeding. www.lllusa.org; Centers for Disease Control (CDC); Harvard Gazette
Contributor: Kathryn N Swatkowski, CNM …has been a Certified Nurse Midwife for 20 years, taking care of women throughout their life-span from adolescence through menopause

This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquiries related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit: https://mackareyphysicaltherapy.com/forum/
Covid-19 has certainly redefined the workplace as many employees continue to work from home. Prolonged hours sitting at a workstation that may not be optimal has also changed the way we define workplace health and safety. It may be more important than ever to pay close attention to designing an ergonomic workstation, changing position, and stretching regularly to prevent injury.
Since 1894 Labor Day has been designated as the national holiday that pays tribute to the contributions and achievements of American workers. Research supports the notion that healthier employees are happier and more productive. When employers encourage healthy behavior and safety at work, they benefit in many ways. For example, in addition to improving job satisfaction and productivity, healthy employees save money by using less sick time, worker’s compensation benefits and health benefits. For example, according to the Centers for Disease Control and Prevention, approximately 75 percent of employers” health care costs are related to chronic medical problems such as obesity, diabetes, high blood pressure, and high cholesterol. Deconditioned, overweight employees are more likely to suffer from these preventable conditions and are at greater risk for injury. Employers, please consider using this holiday as an opportunity to start a health promotion program at your workplace…have a health fair, offer healthy snacks, encourage walking, smoking cessation, exercising at lunch, and offer fitness club stipends.
Lower back pain, one of the costliest illnesses to employers, is one example of a problem which can be prevented with a good health and safety program. It is widely accepted in the medical community that the best treatment for lower back pain (LBP) is prevention. Keeping fit, (flexible and strong), practicing good posture, and using proper body mechanics are essential in the prevention of LBP. At our clinic, significant time and effort is spent emphasizing the importance of these concepts to our patients, employees, and the businesses we work with through industrial medicine programs. A comprehensive approach can produce significant reductions in LBP injuries through an onsite safety program which promotes education, wellness, body mechanics, lifting techniques, postural and stretching exercises and ergonomics.
As little as 10 extra pounds puts great stress on your lower back. It also makes it more difficult to maintain good posture. Eat well, exercise regularly and don’t smoke. Smokers have a much higher incidence of LBP and failure from lower back surgery.
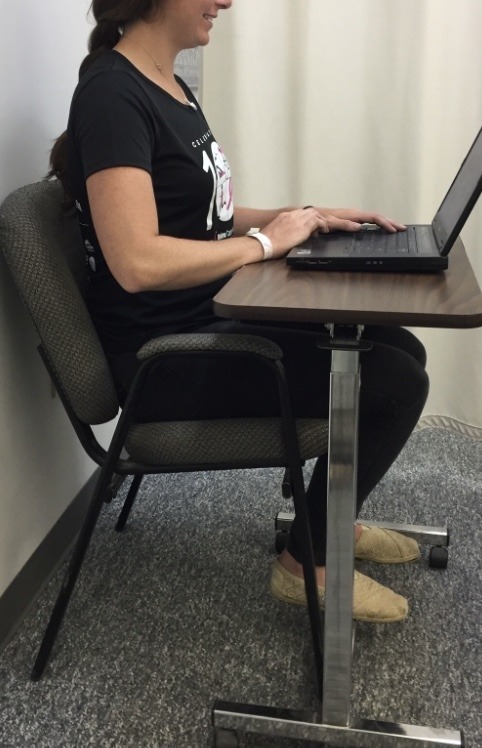
Good posture is critical for a healthy back. When sitting, standing or walking maintain a slight arch in your lower back, keep shoulders back, and head over your shoulders. In sitting, use a towel roll or small pillow in the small of the back.
Perform postural exercises throughout the day. Most of the day we sit, stand, and reaching forward and bend our spine. These exercises are designed to stretch your back in the opposite direction of flexion. Please perform slowly, hold for 3-5 seconds and repeat 6 times each 6 times per day.
Chin Tuck: Tuck your chin back to bring your head over shoulders.
Shoulder Blade Pinch: Pinch your shoulder blades together.
Standing Extension: While standing, put your hands behind back and extend lower back 10-20 degrees.
Good Body Mechanics and ergonomics are also important in the prevention of LBP. When lifting, think twice. Think about the weight, shape and size of the object. Think about where the object is going and the surface resistance of the floor. Does it require two people to lift? Can I safely lift that high or bend that low?

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
For all of Dr. Mackarey's articles visit : https://mackareyphysicaltherapy.com/forum/
“I was nervous and forgot to ask my doctor questions about my diagnosis!” “When the nurse asked me, I could not remember my medications!” These are two examples of the many frustrations patients have when visiting their physicians. Research shows, those who prepare in advance for their physician visits, have more satisfaction than those who just show up for their appointment. Moreover, for patients seeing multiple physicians, such as specialists, often communication is poor and your participation in the process can be invaluable. There are things you can do to prepare for your physician visits...
Remember, your health is too important to rely on memory for accuracy…so be a proactive participant. With technology, it has never been easier to keep a medical journal to improve accuracy and communication. There are several “Apps” such as “mymedicalapp.com” that allow you to do this on your phone, tablet or lap-top computer and offer privacy code features.
SOURCES: www.webmd.com; National Institutes of Health – National Institute on Aging “A Guide for Older People - Talking With Your Doctor”

This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit https://mackareyphysicaltherapy.com/forum/