Despite a recent surge in Covid cases from the new variant, more than 70 percent of Americans anticipate high levels of enthusiasm for travel this summer. Moreover, travel abroad in 2022 is expected to exceed pre-pandemic levels, as isolation weary Americans take to the air!
Confession; I recently was on a long trip that required sitting on an airplane for more than six hours…and I wore compression stockings … guess I’m getting older (and wiser)!
Have you noticed that being in a car or on an airplane for more than three hours leads to neck and back pain? Soreness, stiffness and swelling in your legs? With a little planning preventing or limiting these problems on long trips, is possible. Also, as people age and/or develop other health problems, they are more vulnerable to develop a more serious problem associated with long trips; deep vein thrombosis (DVT) or blood clots. But problems from long-distance travel can be avoided. The following tips, based research and personal experience, can prevent neck, back and leg pain and stiffness and DVT.
A DVT is a blood clot that forms in a deep vein. The deep veins pass through the muscles and cannot be seen like the veins just under your skin. While it may occur in your arms, it is much more common in the legs, especially the calf muscle when traveling. When a blood clot forms in a leg vein it usually sticks to the vein wall. Often, pain and swelling lead you to the doctor and treatment is rendered before serious complications develop. However, there are two possible complications. One, a pulmonary embolus, occurs when a part of the clot logged in your deep vein of the calf breaks off and gets lodged in the lung. This is a very serious problem that can be fatal. Two, post-thrombotic syndrome, occurs when you have pain and swelling in the calf after a DVT.
The following risk factors for DVT significantly increase the potential for problems when traveling on long trips by air more than 5 hours. Trains, cars and buses also create a risk, but air travel creates a greater risk for the following reasons: reduced cabin pressure, reduced cabin oxygen levels, dehydration and alcoholic drinks, which may increase dehydration and immobility.
health
Airplane seats are “C” shaped and force you to round your neck and back forwards. These exercises are designed to stretch and extend your back in the opposite direction. Please perform slowly, hold for 3-5 seconds and repeat 10 times each hour.
When sitting in an airplane seat, take the neck pillow in the overhead compartment and place it in the small of your lower back. While sitting or standing up, perform postural exercises every 30-45 minutes.
NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
Allergies affect 30 % of adults and 40% of children in the United States. Avoiding the outdoors is often not an option…especially if you enjoy outdoor activities and sports. Not long ago, it was unthinkable that an athlete with serious allergies could compete at a high level, such as the Olympics. Now, in great part due to advanced research, medications and proper management, an Olympic gold medal for those suffering from allergies is a reality. Recently, the National Institute of Allergy and Infectious Disease at the National Institutes of Health have published research on this topic to provide a better understanding and make recommendations.
The most common allergic reactions which athletes suffer from are sneezing, itchy and watery eyes, runny nose and coughing. Moreover, 67% of those with these symptoms also suffer from asthma. The athlete in NEPA is particularly vulnerable when the pollen count is high during spring and fall for several reasons. One, after being indoors all winter, one might develop a heightened sensitivity to allergens. Also, increased rapid and deep breathing during exercise makes athletes more susceptible to significant symptoms when exposed to allergens such as tree, grass and weed pollens.
Allergy Shots/Drops
As mentioned last week, allergy skin testing can be performed to determine the allergens to which you are susceptible. Once determined, allergy shots are effective in building up tolerance to these allergens. If appropriate, you may be able to use allergy drops, administered under the tongue and conveniently used at home.
Pre-Treat
Asthma suffers should use their inhaler BEFORE symptoms occur. A recent study found that pretreatment using a short-acting bronchodilator inhaler within 15 minutes before exercise is very effective in preventing asthma symptoms for more than four hours. It is important to keep a bronchodilator available. If you fail to benefit from this, see your physician for other methods to control your exercise-induced symptoms.
Warm-up/Cool Down
Whether you have allergic respiratory problems from rhinitis or asthma, you many benefit from conditioning your airways with a 10 to 15 minute warm-up before and cool-down after the activity. This may serve to gradually prepare your lungs for an increased demand.
Hydrate
In addition to preventing dehydration on hot and humid days, constant hydration is very important for the athlete with allergies to prevent dry airways in athletes.
Guidelines for Athletes with Allergies from the National Athletic Trainers Association:
Educate Staff
Know the signs and symptoms of asthma (coughing, wheezing, tightness in chest, shortness of breath).
Plan for the Problem
Some schools have a file on each student athlete with a allergic or asthmatic problem which requires medication. The file includes information such as medical doctor release and instruction, emergency contacts and medications. Students must have their medications on hand before they can enter the field. The National Athletic Trainers Association recommends using a peak flow meter to monitor at risk players and can determine when a player can return to the field.
Practice in Climate Control
If possible, find an alternate practice facility with climate control for athletes at risk. Plan practices for these athletes when the pollen count is low. Check the newspaper or internet for pollen counts in your area. Training by the water, (ocean) where there is a breeze and less pollen is helpful.
Sources: American College of Allergy, Asthma, and Immunology. National Athletic Trainers Association.

Read “Health and Exercise Forum” by Dr. Paul J. Mackarey every Monday in The Scranton Times-Tribune. Dr. Mackarey is a doctor of orthopedic and sports physical therapy with offices in downtown Scranton. He is an associate clinical professor of medicine at GCSOM.
Read all of Dr. Mackarey's articles at https://mackareyphysicaltherapy.com/forum/
May is National Bike Month! In fact, Saturday, May 7, 2022 Lackawanna Heritage Valley’s Heritage Explorer Bike Tour is returning in person for the first time since 2019. For those who have a bike, now might be a good time to dust it off and enjoy the many beautiful and well-maintained trails that are available at the Countryside Conservancy at Lackawanna State Park, other locations in the Abingtons or the Lackawanna Heritage Valley Authority. For those who don’t have a bike, it might be a good time to get one!
There are many obvious reasons to bike…cardiovascular fitness, burn calories, improve leg strength and others. But, the real question is, “what are the advantages of biking over other forms of exercise?” Glad you asked…
Prevention is the best management of musculoskeletal problems associated with biking. First, many of the problems associated with biking such as knee pain, buttock soreness, and tendonitis can be prevented through proper fitting. Furthermore, it is important that your equipment be in good working order such as tires, chain, brakes and pedals. Next, be sure to maintain a fairly good fitness level in order to bike safely. If you are a beginner, start slowly. Warm up and slowly bike for 10 to 15 minutes and build up over time. Practice the coordination of stopping, starting, shifting and braking. Work on good strength and flexibility of the hamstrings, quadriceps, calves and gluteal muscles. All of these muscles are necessary to generate pedal force. Balance is also important to safety and can be practiced on and off the bike. Be aware that adaptive equipment can modify your bike for added comfort and safety such as soft handlebar tape, seat post and front fork shock absorbers, padded biking shorts, c-out and gel pad saddle seats, and wider tires.
Be careful not to progress too quickly because inactivity to over activity in a short period of time can create problems. Overuse injuries such as tendonitis, can be avoided by cross training. Bike every other day and walk, run or swim on off days. Make sure to take time off to recover after a long ride. Use ice and massage to sore muscles and joints after riding.
Remember, cycling should be fun! Pain from improperly fitted and poorly maintained equipment is preventable. Excessive workouts and training rides should be kept to a minimum and consider cross-training in between.
EQUIPMENT: Helmets are a must! Also, keep your bike in good condition. Road bikes should have mirrors and reflectors. Use hand signals and obey traffic rules. Dress for weather and visibility. Have a first aid and tire patch kit, tire pump and tools. Seat comfort can be improved with gel cushion or split seat.
BE ALERT: for traffic, parked cars, pedestrians loose gravel and cracks in the road.
SOURCES: American Physical Therapy Association
The last two columns in “Health & Exercise Forum” have been dedicated to the health benefits of exercise for Parkinson’s disease. Specifically, the use of dance was featured as a method to promote strength, balance, coordination and agility in this population. However, dance as a form of exercise and for the promotion of balance, coordination and agility, is not limited to those with neurological conditions…it is beneficial for everyone! In fact, my wife, Esther and I, have always enjoyed our dance classes with Vince Brust!
Like most forms of exercise, if done regularly, dance can have multiple health benefits. If dance is your only form of exercise, make it your goal to sustain the activity for about 30 minutes a day, 3-4 days per week for the most value.
If you have any doubt or reservations about the ability of dance to improve your health and wellness, take notice of the muscle tone, flexibility, agility and coordination of a professional dancer...ballet, modern, hip hop, jazz, etc. They are incredible athletes and artists!
It is common to lose agility and flexibility with age especially if you regularly perform the same limited movements throughout your day and lifetime. This will lead to stiffness and lack of flexibility, especially for new or season activities which can make you more vulnerable for injury and pain. Lower back pain and calf or hamstring strains are most common. Research suggests that dance can help.
For example, in one study it was found that cross-country skiers who received months of dance training showed improvements in joint mobility and muscle flexibility of the spine, as well as their speed and agility.
It is also expected that balance and coordination are also compromised with age. It’s one of the reasons that older adults are so prone to falls. The research also supports the value of dance to offset this problem.
One particular study found that in people over the age of 80 years, social dancing helped improve balance and walking speed, as well as contributing to a more stable walking pattern.
Moderate-intensity dance, performed continuously for at least 30 minutes on a regular basis has been found to reduce the risk of death from cardiovascular disease in some studies. Moreover, it has been more effective in prevention than average-pace walking ...and is less boring!
Most activities of daily living (walking, climbing stairs) occur in a linear and forward directon. However, dance has not set direction and can move in multiple planes (forwards, backwards, and sideways with diagonal and rotational components.
These unlimited movements, not only improves agility, coordination, and balance, but also strengthens muscles that often get forgotten like your core and abdominals.
As with any cardiovascular exercise, dance is a form of aerobic exercise which burns calories. This is especially true if performed a minimum of moderate-intensity for 30 minutes or longer.
According to the American Diabetes Association, aerobic exercise can support weight loss.
Weight-bearing exercise is the cornerstone for any osteoporosis prevention program and dance is a prime example.
According to the National Osteoporosis Foundation, high-impact, weight-bearing exercises, such as certain forms of dance, can help maintain bone strength and even build new bone mass. This slows the development and progression of osteoporosis. It is also well established that low-impact weight-bearing exercise (dancing with the impact of jumping etc.) is effective in bone loss prevention. Dance can be whatever intensity you want it to be, depending on your mood, energy level, and physical limitations.
Like most forms of exercise, especially aerobic, dance can improve cognitive health. In addition to releasing special hormones, it can also improve circulation and oxygenation to the brain to enhance brain health.
Some research suggests that dance can help create new connections between brain regions involved in long-term memory and improve mood, cognitive acuity and mental energy.
Physicians and physical therapists often recommend dance as a form of rehabilitation following brain injury, stroke or dementia.
One study found that out of many different types of exercise (including dance, swimming, golf, cycling, tennis, and others) dance was the only one associated with a lower risk of dementia for people in the study. Experts believe the benefit was due to a combo of social interaction and mental focus...that is not to say that the aforementioned types of exercise do not have value.
Dancing can contribute to your mental health by improving mood and reducing stress. As Morrie advised in Mitch Albom’s best-selling book, Tuesdays with Mori, “dance like nobody’s watching”...it can be very invigorating!
Dance participants ranked mood enhancement as the number one reason for participation! One study examining people’s motivation for dancing, “mood enhancement” ranked top on the list. The dancers felt that the activity is expressive and allows you to escape and “let your hair down.”
Some studies also suggest that dance therapy might also reduce depression, especially in those who have serious illnesses, such as breast cancer or Parkinson’s (read last week’s column). Researchers feel that this may be due to increased endorphins and lower cortisol levels.
The pandemic has taught most of us a valuable lesson ... some of us have a serious need to socialize and some do not. For those like me, who thrive on being among others, dance classes and dance-style workouts often take place in groups, which allows for social bonding in a fun, light and breezy environment.
Depending on your marital status and the specific style of dance you choose (salsa, tango or swing dancing), you may even be paired up with a partner every week!
While exercise on treadmill, bike or elliptical can be great exercise, it also can be boring and repetitive. Research suggests that any form of exercise can boost self-esteem.
When dancing, however, you get all the benefits of exercise, while simultaneously learning a new skill. It can be incredibly rewarding and satisfying to master the skill, especially with others such as learning the tango.
SOURCE: “Greatest” Debra Sullivan, Ph.D., MSN, R.N., CNE, COI

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.comPaul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine GCSOM.
For all of Dr. Mackarey's articles visit www.mackareyphysicaltherapy.com/forum
“Dance like nobody’s watching!” This is one of my favorite quotes from Mitch Albom’s book, Tuesdays With Mori, because it represents interesting facts about human behavior. One, of course, is the ability to be comfortable in your own skin. The other, maybe less obvious benefit is that challenging your balance through dancing, even if it’s not pretty, is very effective in maintaining or improving quality of life for those with challenges in gait and balance, as found in Parkinson’s disease (PD). In fact, “Dance for PDR”, a new and popular treatment for PD, has recently been validated in the scientific literature as a valuable treatment tool for those with PD.
Research published in the Journal of Neural Transmission, shows that dancing is shown to help people with PD improve their ability to walk and enhances their quality of life. The program was applicable to those at various stages of PD, including those using walkers. Moreover, the results found that, in addition to physical improvements, participants also had psychological and social benefits through camaraderie, joy of movement and less isolation.
Participants, none of whom had ever engaged in a dance class before, performed a structured dance program for 16 sessions over 8 weeks. Each class was 75 minutes long with seated warm-up activities 50% of the time. Results showed: 10%improvement in overall movement, 26% improvement in walking and 18% improvement in tremor.
Parkinson’s disease is a chronic, degenerative disease that leads to slowness of movement, balance disorders, tremors, and difficulty walking. PD results from the loss of dopamine-producing nerve cells in the brain. Dopamine is critical to stimulate the nerves of the muscular system in the body. PD affects approximately 1.5 million people in the USA with 60,000 new cases each year according to the National Parkinson Foundation. Most people know someone affected by PD. PD typically affects those over 65 years of age and only 15% are under 50.
While there is no current cure for PD, exercise is well documented to relieve some of its symptoms. Specifically, exercise can help keep muscles strong, joints mobile, and tissues flexible. Exercise will not stop PD from progressing, but it will improve balance, enhance walking ability, reduce muscle weakness, and minimize joint stiffness. In 2007, a study published in the Journal of Neuroscience revealed that exercise may benefit individuals with PD because exercise encourages the remaining dopamine cells to work harder to produce more dopamine. Also, the researchers discovered that exercise decreases the rate at which dopamine is removed from the brain.
Exercise to improve strength, balance, and flexibility can be performed independently at home or supervised at a rehab or exercise facility. Supervised exercise can include physical therapy, recreational therapy, water therapy, yoga, and Tai Chi. Physical therapy can improve walking ability, enhance balance, reduce fatigue, increase strength, promote flexibility and minimize pain. Physical therapy uses movement techniques and strategies as well as various pieces of equipment to enhance an individual’s level of independence and improve his quality of life. PT can also incorporate leisure activities (e.g. golfing and ballroom dancing) to reduce the symptoms and associated limitations of PD. Tai Chi, a total mind and body workout, is a series of individual dance-like movements linked together in a continuous flowing sequence. Particular benefits for people with PD include reduced stress, increased energy, improved concentration and focus, better circulation and muscle tone, and significant improvements in balance.
According to Dance for PDR,their programoffers internationally acclaimed dance classes for people with Parkinson’s disease in Brooklyn, New York and, through a network of partners and associates, in more than 120 other communities and 16 countries. In Dance for PD classes, participants are empowered to explore movement and music in ways that are refreshing, enjoyable, stimulating and creative. For more information visit: www.danceforpd.org
So, if you like to dance, “keep on dancing!” If you don’t dance and notice some changes in balance and coordination, or if you have PD…it’s a good time to start! “Dance like nobody’s watching!”

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com. Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit www.mackareyphysicaltherapy.com/forum
Parkinson’s disease (PD) is a chronic, degenerative disease that leads to slowness of movement, balance disorders, tremors, and difficulty walking. PD results from the loss of dopamine-producing nerve cells in the brain. Dopamine is critical to stimulate the nerves of the muscular system in the body. PD affects approximately 1.5 million people in the USA with 60,000 new cases each year according to the National Parkinson Foundation. Most people know someone affected by PD. PD typically affects those over 65 years of age and only 15% are under 50. However, actor, Michael J. Fox brought national attention to the disease in 1991 when he was only 30 years old. Juvenile Parkinson’s, those diagnosed under the age of 40, is rare and only represents 7% of all those with PD.
While there is no current cure for PD, exercise can relieve some of its symptoms. Although PD affects an individual’s ability to move, exercise can help keep muscles strong, joints mobile, and tissues flexible. Exercise will not stop PD from progressing, but it will improve balance, enhance walking ability, reduce muscle weakness, and minimize joint stiffness. In 2007, a study published in the Journal of Neuroscience revealed that exercise will benefit individuals with PD because exercise encourages the remaining dopamine cells to work harder to produce more dopamine. Also, the researchers discovered that exercise decreases the rate at which dopamine is removed from the brain.
Depending on the stage of the disease and the level of assistance required, exercise to improve strength, balance, flexibility and ambulation for those with PD, can be performed independently at home or supervised at a rehab or fitness facility. Supervised exercise can include physical therapy, recreational therapy, water therapy, yoga, and Tai Chi… AND DANCE! Physical therapy can improve walking ability, enhance balance, reduce fatigue, increase strength, promote flexibility and minimize pain. Physical therapy uses movement techniques and strategies as well as various pieces of equipment to enhance an individual’s level of independence and improve his quality of life. Recreational therapy incorporates leisure activities (e.g. golfing and ballroom dancing) to reduce the symptoms and associated limitations of PD. Recreational therapy adapts these activities to meet the specific needs of the person with PD. The modified activities are taught by professionals who have significant knowledge and experience in this area. Water therapy is especially helpful to people with PD because the water provides enough buoyancy to lessen the amount of balance required to perform essential exercises. The cushioning effect of the water allows for freedom of movement while providing the appropriate level of resistance necessary to achieve the desired results. Using a combination of physical and mental exercises, yoga promotes flexibility, reduces stress levels, and increases stamina and strength in individuals with PD. Tai Chi, a total mind and body workout, and is a series of individual dance-like movements linked together in a continuous flowing sequence. Particular benefits for people with PD include reduced stress, increased energy, improved concentration and focus, better circulation and muscle tone, and significant improvements in balance.
If you choose the convenience of a home exercise program, consult your physician or physical therapist for recommendations regarding: (1) the types of exercise best suited for you and those which you should avoid, (2) the intensity of the workout, (3) the duration of your workout, and (4) any physical limitations you may have.
The type of exercise that works best for you depends on your symptoms, fitness level, and overall health. Your exercise program should address not only strength but also flexibility and endurance and should include all body parts: face, mouth, neck, torso, arms, legs, hands, and feet. Some general exercise suggestions include:
Since individuals with PD are at risk for falling and freezing (becoming rigid), work out in a safe environment and, if possible, when someone is present. Avoid slippery floors, poor lighting, throw rugs, and other potential dangers (e.g., watch out for the pooch because he might want to join in the fun). If you have difficulty balancing, exercise sitting down, lying on the bed or within reach of a grab bar or securely installed rail. Stop and rest if you feel tired during your exercise program since overexertion can make your PD symptoms worse.
Contributions: Janet Caputo, DPT, OCS,

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” Next Week: Part II of II: Dance for Parkinson ’s Disease.
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.comPaul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit: http://www.mackareyphysicaltherapy.com/forum
In 2000, President Bill Clinton dedicated March as National Colorectal Cancer Awareness Month. The purpose of this designation is to increase public awareness of the facts about colon cancer – a cancer that is preventable, treatable and has a high survival rate. Regular screening tests, expert medical care and a healthy lifestyle, which includes a proper diet and exercise, are essential for prevention. Several studies have demonstrated that exercise can also help prevent colon cancer.
The American Cancer Society estimates that there will be approximately 150,000 new cases of colorectal cancer in 2021. Of these, 52,980 men and women will succumb to the disease. It is the second-leading cause of U.S. cancer deaths for both men and women combined. The good news is incidence and mortality rates are dropping both nationally as well as in northeast Pennsylvania. The bad news is northeast Pennsylvania still has increased incidence and mortality rates when compared to the national average.
Studies show that prevention of this disease is multifaceted and includes: engaging in daily exercise, eating a low-fat diet with little red meat, avoiding smoking, drinking in moderation and having regular colonoscopy screenings.
Early detection is the key to survival. Death from colorectal cancer can be eliminated if caught at the earliest signs of disease. Colorectal cancer progresses very slowly, usually over years. It often begins as non-cancerous polyps in the lining of the colon. In some cases, these polyps can grow and become cancerous, often without any symptoms. Some symptoms that may develop are: blood in stool, changes in bowel movement, feeling bloated, unexplained weight loss, feeling tired easily, abdominal pain or cramps, and vomiting. Contact your physician if you have any of these symptoms.
The risk of colon cancer increases with age, as 90 percent of those diagnosed are older than age 50. A family history of colon cancer increases risk. Also, those with benign polyps, inflammatory bowel disease, ulcerative colitis or Crohn’s disease are at greater risk and should be screened more frequently.
The intestine works like a sewage plant, recycling the food and liquid needed by your body. However, it also stores waste prior to disposal. The longer the wastes remain idle in your colon or rectum, the more time toxins have to be absorbed from you waste into the surrounding tissues. One method in which exercise may help prevent colon cancer is to get your body moving, including your intestines. Exercise stimulates muscular contraction called peristalsis to promote movement of waste through your colon.
Exercise to prevent colon cancer does not have to be extreme. A simple increase in daily activity for 15 minutes, two times per day or 30 minutes, once per day is adequate to improve the movement of waste through your colon. This can be simply accomplished by walking, swimming, biking or playing golf, tennis or basketball. For those interested in a more traditional exercise regimen, perform aerobic exercise for 30-45 minutes four to five days per week, with additional sports and activities for the remainder of the time. For those in poor physical condition, begin slowly. Start walking for five to 10 minutes, two to three times per day. Then, add one to two minutes each week until you attain a 30-45 minute goal.
Dr. Christopher Peters is a partner of Radiation Medicine Associates of Scranton (RAMAS) and serves as medical director of Northeast Radiation Oncology Centers (NROC). He is an associate professor of clinical medicine at GCSOM.
Sources: American Cancer Society/Northeast Regional Cancer Institute, and CA Cancer J Clin.

This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
Spring is just around the corner so it is time for running enthusiasts to lace up their sneakers, get outside and run! Runners are addicted to running for good reason. There is nothing like it! No exercise offers so much in such little time. For example, the caloric expenditure while running is higher than for most other exercises, including biking. Also, it allows for fresh air and beautiful scenery with a minimal investment in clothing or equipment. It requires little skill and time to learn. Runners suffer from less depression, colds and flu symptoms, and experience less pain due to an endorphine release (natural chemical in the brain associated with euphoria and pain control) that is greater than found in other sports and activities. These are some of the motives that cause people to run every day, in spite of the constant loading and wear and tear on the joints.
To be a competitive runner and have longevity in the sport, optimal form is necessary. Moreover, a recent study shows that a runner can decrease the stresses on the lower body and reduce the incidence of stress fractures when trained to run with proper form using visual feedback while on a treadmill. The application of this information has significant implications for training programs for runners for the prevention and recovery from injury. One such low impact method is called the “Pose Running Technique,” by Dr. Nicholas Romanov. It is a “soft landing” method which promotes; an S-like body position with slightly bent knees, a slightly forward lean at the ankles to employ gravity and momentum, lifting the feet up under the hips, and landing on the ball of the foot under the body to absorb the center of mass.
It is my opinion, that the best runners, with the least injuries, such as Jordan Hoyt, speedster from Abington Heights, employ these techniques naturally. Additionally, many of the world’s best runners use coaches and trainers to assist them in their quest for success and injury prevention by using perfect form. However, for the rest of us, we must learn to maximize the efficient use of the body as it works with, not against gravity. We must learn to run “soft” to prevent injuries.
A slight upward tilt of the head to allow a view of the horizon ahead should be most comfortable. Avoid looking down or up to extremes. Do not rock or rotate the head while running.
Loose and relaxed shoulders set the tone for a good run. Keep them level without tilting side to side or rotating left to right. Avoid holding the shoulders in a tight and high position.
Loose and relaxed arms also set the tone for a good run. A good arm swing is always in forward motion in a linear direction and stays between the waist and lower chest. Never clench the fist. Do not rotate or twist the arms across the body.
If the head, shoulders and arms are in correct position, then the torso will be upright. An erect running posture is necessary to promote efficient movement and breathing. The posture that you assume when taking a deep breath is the correct torso position for good breathing while running.
The hips will follow the position of the parts above in a linear forward direction. However, if the torso leans forward because the head hangs down then the hips will tilt downward. If the arms swing and torso rotates side to side, then the hips will also rotate.
Sprinters need to lift the knees high to thrust the lower legs forward. Long distance runners cannot maintain a high knee lift for a long period of time, however, a slight knee lift with a shorter but quicker stride is more efficient. Proper running requires the foot to softly strike the ground with the knee slightly bent. If the knee is fully extended in front of the body upon impact, the stride is too long and the force too great.
To excel as a runner, when the foot hits the ground it should land lightly, between the heel and the midfoot. The ankle is flexed and rolls quickly forward to the toes to push off the ground with maximum force. The calf muscle propels the runner forward. Efficient running has a quiet and springy landing. A loud foot slap on impact is a sign of poor form and results in excessive force transferred to the lower leg. The foot should spend as little time as possible in contact with the ground…thus a soft runner “floats” when they run.
SOURCES: Runner’s World, Pose Running Technique (www.posetech.com), Journal of Orthopaedic and Sports Physical Therapy.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
Pre-pandemic we saw increased popularity of local races such as the Steamtown Marathon and Scranton 1/2 Marathon. With that, local interest in running was exploding and will hopefully return to normal soon. However, during the pandemic, especially when fitness centers were closed, many took seasoned and beginner runners to the streets to improve fitness and alleviate stress. However, as a health care provider, I am seeing a significant number of first time runners visit my office with a wide variety of injuries that are very preventable with a modicum of good judgment.
Runners are addicted to running for good reason. There is nothing like it! No exercise offers so much in such little time. Caloric expenditure is higher than in most other exercises, including biking. Running also allows for fresh air, beautiful scenery, minimal investment in clothing or equipment, little skill and time to learn. Moreover, the benefits are many; runners suffer from less depression, colds and flu symptoms, and experience less pain due to an endorphin release (a natural chemical in the brain associated with euphoria and pain control.)
This column will be dedicated to those who are interested in beginning a running program for all the reasons mentioned above and more. The program is designed to promote a safe and gradual introduction or return to running as form of exercise. The initial goal is to help you attain 30 minutes (approximately 2 miles) of running at a slow, relaxed and safe pace. This 30 minute goal is the standard used in most research that shows improvement in weight control, cholesterol, heart disease, blood pressure and adult onset diabetes. The 8 week program is a simple and safe program that begins with more walking than running and gradually reverses the proportion. The first two miles are the hardest and once mastered; one can begin to build on mileage and intensity if desired. For those interested in advancing to a half or full marathon, I recommend the book “The Marathon” by Jeff Galloway who advocates a run/walk program as you increase distances. Visit his website at: www.jeffgalloway.com.
The appearance of an arch in a weight bearing position does not automatically exclude the individual from excessive supination or pronation. Consult a podiatrist or an orthopedic physical therapist to determine the propensity toward supination, pronation or neutrality of the foot and ankle.
Note: New Balance, Brooks, Asics, Mizuno & Saucony all make quality running shoes to accommodate a supinated, pronated or normal foot.
Mon.Wed.Fri.Sat: Run 1 minute. Walk 2 minutes. Repeat 10 Times
Tues.Thurs: Walk 30 minutes
Sun: Rest
Mon.Wed: Run 2 minutes. Walk 1 minute. Repeat 10 Times
Fri.Sat: Run 3-4 minutes. Walk 1 minute. Repeat 6-7 Times
Tues.Thurs: Walk 30 minutes
Sun: Rest
Mon.Wed: Run 5 minutes. Walk 1 minute. Repeat 5 Times
Fri.Sat: Run 6 minutes. Walk 1 minute. Repeat 4 Times
Tues.Thurs: Walk 30 minutes
Sun: Rest
Mon.Wed: Run 8 minutes. Walk 1 minute. Repeat 3 Times THEN: Run 3 minutes
Fri.Sat: Run 10 minutes. Walk 1 minute. Repeat 2 Times THEN: Run 8 minutes
Tues.Thurs: Walk 30 minutes
Sun Rest
Mon.Wed: Run 12-13 minutes. Walk 1 minute. Repeat 2 Times THEN: Run 2-4 minutes
Fri.Sat: Run 14-15 minutes. Walk 1 minute. Repeat 2 Times THEN: Run 2 minutes
Tues.Thurs: Walk 30 minutes
Sun: Rest
Mon.Wed: Run 16-17 minutes. Walk 1 minute. THEN: Run 12-13 minutes
Fri.Sat: Run 18-19 minutes. Walk 1 minute. THEN: Run 10-11 minutes
Tues.Thurs: Walk 30 minutes
Sun: Rest
Mon.Tues.Wed: Run 20-22 minutes. Walk 1 minute. THEN: Run 7-9 minutes
Fri.Sat: Run 24-26 minutes. Walk 1 minute. THEN: Run 3-5 minutes
Thurs: Walk 30 minutes
Sun: Rest
Mon.Tues.Wed: Run 27-28 minutes. Walk 1 minute. THEN: Run 1-2 minutes
Fri.Sat: Run 29-30 minutes. Walk 1 minute. THEN: Run 0-1 minutes
Thurs: Walk 30 minutes
Sun: Rest
SOURCE: Runner’s World

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” NEXT WEEK…RUN WITH GOOD FORM!
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
Injuries due to falling are a very common problem in the elderly. Hip fractures are the most common injury due to falling in the seniors. According to the American Academy of Orthopaedic Surgeons, each year more than 300,000 people are hospitalized for hip fractures in the United States. These fractures represent 72% of all fracture costs, totaling more than 12 billion dollars in 2005 and, not surprisingly, 90% occurred in those 65 and older. Most hip fracture patients who previously lived independently will require family assistance, home or long term care and 50% will require a cane or walker.
A recent study by the American Physical Therapy Association found that patients benefited from a physical therapy evaluation to determine their risk level for falling. If a high-risk level is found on a falls assessment, physical therapy interventions can be successfully employed to improve strength, balance, and coordination and falls prevention. Also, a well-balanced diet, exercise, Calcium with vitamin D supplements and medications can help prevent or retard osteoporosis and prevent hip fractures.
***Always perform slowly, alternate right and left sides, limit other distractions and concentrate on the exercise to retrain the brain, 10-20 times each 2-3 times per day.
***Caution: Do not do standing exercises without assistance or supervision if needed
Face a countertop and hold onto it with both hands. Hike your hip and knee up to 90 degrees as if you are marching. Hold the position for 3-5 seconds on one leg and lower slowly. Repeat this on the other leg and alternate 10 times.

Face a countertop and hold onto it with both hands. Lift your leg up 30 degrees as if you are spreading your legs apart. Hold the position for 3-5 seconds on one leg and lower slowly to cross over the middle. Repeat this on the other leg and alternate 10 times.
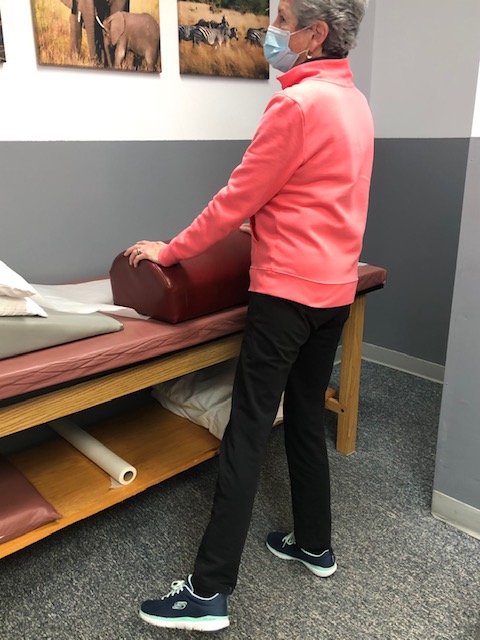
Face a countertop and hold onto it with both hands. Bend your hip and knee down to 45 degrees to a squatting position. Hold the position for 3-5 seconds on both legs and return to standing slowly. Repeat this 10 times. Once strong enough try on one leg at a time and alternate.
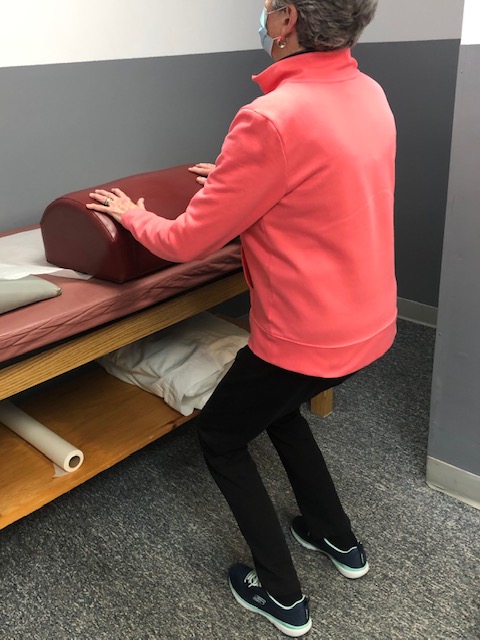
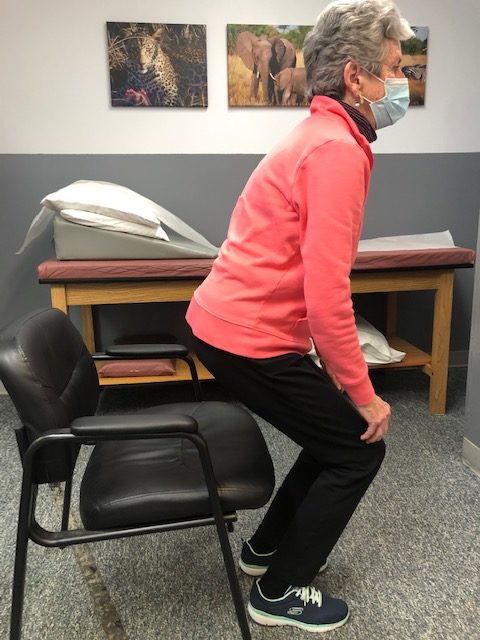
Sit in a chair with arm rests. Get out of chair only using your legs. Hold the position for 3-5 seconds and return to sitting. If necessary, use 1 or 2 arms to assist. Repeat this 10 times. Focus on trunk core stabilization and leg strength. Use more leg muscles and less arm muscles as strength improves.
Place a straight line on the floor and practice “walking the line” with the right then left foot on the line.
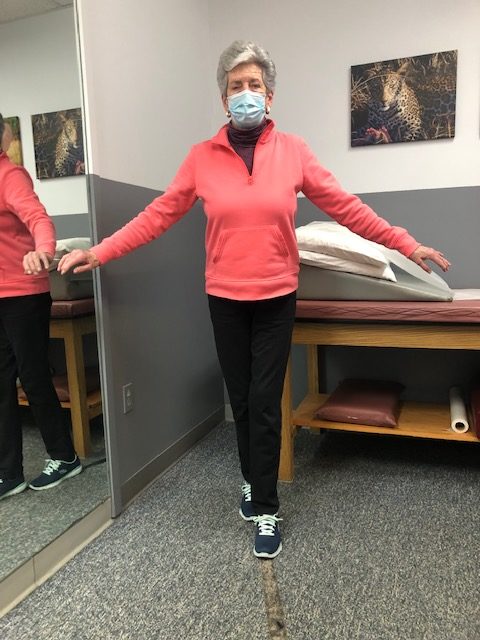
Hold onto a chair while bending one knee and shifting your weight to the other leg. Hold for 3-5 seconds and repeat with the other leg. Increase time 10 -15 -20 seconds as tolerated.

If you feel you or a loved one may be at risk for falling or a hip fracture, ask your family physician if a physical therapy consultation for a falls prevention program to prevent hip fractures may benefit you.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit www.mackareyphysicaltherapy.com/forum