In 2000, President Bill Clinton dedicated March as National Colorectal Cancer Awareness Month. The purpose of this designation is to increase public awareness of the facts about colon cancer – a cancer that is preventable, treatable and has a high survival rate. Regular screening tests, expert medical care and a healthy lifestyle, which includes a proper diet and exercise, are essential for prevention. Several studies have demonstrated that exercise can also help prevent colon cancer.
The American Cancer Society estimates that there will be approximately 107,000 new cases of colorectal cancer in 2023. Of these, 52,550 men and women will succumb to the disease. It is the second-leading cause of U.S. cancer deaths for both men and women combined. The good news is incidence and mortality rates are dropping both nationally as well as in northeast Pennsylvania. The bad news is northeast Pennsylvania still has increased incidence and mortality rates when compared to the national average.
Studies show that prevention of this disease is multifaceted and includes: engaging in daily exercise, eating a low-fat diet with little red meat, avoiding smoking, drinking in moderation and having regular colonoscopy screenings.
Early detection is the key to survival. Death from colorectal cancer can be eliminated if caught at the earliest signs of disease. Colorectal cancer progresses very slowly, usually over years. It often begins as non-cancerous polyps in the lining of the colon. In some cases, these polyps can grow and become cancerous, often without any symptoms. Some symptoms that may develop are: blood in stool, changes in bowel movement, feeling bloated, unexplained weight loss, feeling tired easily, abdominal pain or cramps, and vomiting. Contact your physician if you have any of these symptoms.
The risk of colon cancer increases with age, as 90 percent of those diagnosed are older than age 50. A family history of colon cancer increases risk. Also, those with benign polyps, inflammatory bowel disease, ulcerative colitis or Crohn’s disease are at greater risk and should be screened more frequently.
The intestine works like a sewage plant, recycling the food and liquid needed by your body. However, it also stores waste prior to disposal. The longer the wastes remain idle in your colon or rectum, the more time toxins have to be absorbed from you waste into the surrounding tissues. One method in which exercise may help prevent colon cancer is to get your body moving, including your intestines. Exercise stimulates muscular contraction called peristalsis to promote movement of waste through your colon.
Exercise to prevent colon cancer does not have to be extreme. A simple increase in daily activity for 15 minutes, two times per day or 30 minutes, once per day is adequate to improve the movement of waste through your colon. This can be simply accomplished by walking, swimming, biking or playing golf, tennis or basketball. For those interested in a more traditional exercise regimen, perform aerobic exercise for 30-45 minutes four to five days per week, with additional sports and activities for the remainder of the time. For those in poor physical condition, begin slowly. Start walking for five to 10 minutes, two to three times per day. Then, add one to two minutes each week until you attain a 30-45 minute goal.
Medical Contributor: Christopher A. Peters, M.D
Dr. Christopher Peters is a partner of Radiation Medicine Associates of Scranton (RAMAS) and serves as medical director of Northeast Radiation Oncology Centers (NROC). He is an associate professor of clinical medicine at GCSOM. Sources: American Cancer Society/Northeast Regional Cancer Institute, and CA Cancer J Clin.

EVERY MONDAY - Read Dr. Paul J. Mackarey "Health & Exercise Forum!"
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's Articles, visit our Healthcare Forum!
PEOPLE WILL OFTEN ASK ME, “IS THERE SUCH A THING AS AN EXERCISE RUT?” THEY WANT TO KNOW WHY THEY DO NOT SEEM TO BE IMPROVING WITH THEIR EXERCISE PROGRAM…they exercise 3-4 times a week for 30 to 45 minutes and they feel frustrated and STUCK in a rut.
The purpose of this column will be to offer suggestions on how to improve or get more out of a “stale” exercise program. Last week’s column offered tips to improve a stale cardiovascular and strength program. This week we will discuss flexibility and functional training tips and include the components necessary for a healthy mind, body and spirit connection.
Flexibility training involves the careful stretching of the muscles, tendons and joints to improve the range of motion in order to safely perform daily activities and sports without injuring or tearing soft tissues. It is probably the most neglected part of the fitness program. However, while the amount of inherent flexibility varies for each person, a minimal range is necessary as it relates to daily activities and sports. For example, as you age it is important to have enough flexibility in your back, hips and knees to wash your feet, put shoes and socks on. Flexibility exercises should always be performed after a warm –up activity and done slowly and gently.
There are two types of flexibility exercises; dynamic and static. Dynamic stretching is performed with movement such as pushing the ankle up and down like a gas pedal. Passive stretching is performed using an outside force such as using a towel to pull the ankle up in order to stretch the calf. Dynamic should be performed before an activity (before running or playing tennis) and static performed after the activity is over in order to increase range of motion for future activities.
In conclusion, it is easy for fitness enthusiasts to get so focused on maintaining a routine that they allow their program to become stale and ineffective. It is essential to reassess and update your program to prevent stagnation.
Make sure the routine has all three fundamental components of a well-balanced exercise program; cardiovascular, strength and flexibility training. Moreover, to be truly healthy, one must work toward a “Healthy Mind, Body, and Spirit. Therefore, in addition to traditional exercise one must incorporate the following: nutrition; meditation, relaxation techniques, yoga, core fitness; functional/sports specific training; leisure sports and activities
In order to prevent an exercise program from getting stale, one must incorporate all aspects of wellness…a healthy mind, body and spirit!
While each component offers its own specific benefit, the combination of all three cooperatively provides unique value. Too often, fitness enthusiasts concentrate on the exercises they LIKE or are good at more than the ones they NEED.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine
For all of Dr. Mackarey's articles our Health Care Forum
People will often ask me, "Is there such a thing as an exercise rut?" They want to know why they do not seem, to be improving with their exercise program?... they exercise 3-4 times a week for 30 to 45 minutes and they feel frustrated and STUCK in a rut. While initially responding favorably to exercise, after 6 -9 months or more, they do not notice progress in weight loss, strength, tone, endurance or daily function.
Here are a few suggestions on how to improve or get more out of a “stale” exercise program.
Step one is to build an exercise program that is grounded in the basics. Next, Step two, which begins after the basics have been mastered, includes the components necessary for a healthy mind, body and spirit connection and translates into functional activities of daily living including work and leisure sports.
Make sure your routine has all three fundamental components of a well-balanced exercise program:
While each component offers its own specific benefit, the combination of all three cooperatively provides unique value. Too often, fitness enthusiasts concentrate on the exercises they LIKE or are good at more than the ones they NEED. A well-balanced program includes what you like and need!
In fact, recent studies show that those performing all three components surpassed those performing one or any combination of two of the training types when tested for efficient:
Cardiovascular exercise is any activity that raises your heart rate and respiratory rate. This type of exercise strengthens the heart muscle and the muscles that assist in breathing. When these muscles are stronger, they in turn work more efficiently to deliver oxygen to your muscles and other parts of the body. Ultimately, these oxygenated muscles can work harder and longer to burn fat during exercise and at rest.
*Most experts recommend at least 30 minutes of sustained cardio, 3-4 days per week. However, recent studies support the notion of performing 10-15 minutes, twice daily, 4 days per week. For those “stuck” in a fitness rut, to advance your program, cardio should be performed 5-6 days per week for 45-60 minutes.
Strength training is an activity that provides any type of resistance to muscle contraction to build strength in the muscle. The resistance can be without movement against an immovable object such as pushing against a wall (isometric) or with movement such as lifting up or lowering a weight down against gravity (isotonic/dynamic). There are two types of isotonic muscle contraction; concentric, which involves raising the weight against gravity as the muscle shortens and eccentric which involves lowering a weight against gravity as the muscle lengthens.
A standing biceps curl is an example that incorporates both concentric and eccentric contractions. A progressive strength training program includes all three types of muscle contraction. By using the classic bicep muscle curl these photos will demonstrate all three types of muscle contraction:


Sources: National Institutes of Health; American Council on Exercise
Model: Heather Holzman

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” Next Week: Read Stuck in an Exercise Rut…Part II of II!
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine
For all of Dr. Mackarey's articles visit: Mackarey's Health and Exercise Forum!
In Northeastern Pennsylvania, winter is a fun-filled time for outdoor activities. Many people will be enjoying the outdoors hiking, snow shoe hiking, sledding, down-hill and cross-country skiing, snow-boarding, ice-skating and ice fishing. However, frigid, wind, snow, and sleet can play havoc on your skin. It is critical to be keenly aware of the time spent in the cold no matter what age and to recognize the importance of making skin protection part of your daily regimen throughout the entire year. Dry, red, flaking, itchy and scaly skin can make you crazy and uncomfortable. Furthermore, dry and cracked skin is an opportunity for a variety of bacterial, fungal and viral infections to enter your body.
Excessive use of soap and water in the cold winter months can strip away the skin’s natural oils. Use cleansing creams, gentle skin cleansers or bath lotions with moisturizers instead of harsh soap. Following the use of a good skin product, your shin should feel soft and smooth, not tight or dry. Non detergent fragrance free neutral-pH products are helpful and kind to winter skin. Experiment with several mild soaps such as CetaphilR, AveenoR, NeutrogenaR, BasisR or DoveR until you find the right one for you. Dr. Ted Stampien, MD, a local dermatologist in Clarks Summit, recommends that shower gels should be avoided because they contain alcohol.
One proven method to prevent dry winter skin even when using regular soap is to moisturize your skin immediately after bathing to trap in water in the surface cells and then gently pat dry. For severe dryness, Dr. Stampien also recommends that you apply a second coating of moisturizing cream after you pad dry for further protection. He notes that creams are more moisturizing than lotions or gels. For extremely dry skin apply baby oil or almond or vitamin E oil to moist skin. Also, if your skin is so dry that it itches, apply 1% hydrocortisone to the area followed by a thick moisturizing cream. Try thicker creams such as Eucerin and Lubriderm and use cosmetics with moisturizers.
Many people forget to protect their skin from the sun in the winter. However, when the winter sun is reflected off the snow and ice it can be very strong on an unprotected face, especially the cheeks and lips.
WhWhile SPF 15 is considered adequate protection, dermatologists recommend a minimum of SPF 30 or greater for most people. Choose a sunscreen with ingredients that block both UVB and UVA rays. Apply lotion liberally to all exposed skin before you go outside. Remember to include the lips, ears, and around eyes. Sunscreens are available in lotion, gel, spray, cream and sticks. Some are made fragrance-free, hypoallergenic, or especially for sensitive skin or children. Dr. Stampien states that patients with sensitive skin or eczema typically tolerate sunscreens that contain zinc and titanium oxide such as Blue LizardR, SolbarR and NeutrogenaR and that these patients should avoid sprays and gels as these products usually contain alcohol which can sting upon application.
UVUV-blocking ski goggles or sunglasses with wraparound or large frames protect your eyelids and the sensitive skin around your eyes, common sites for skin cancer and sun-induced aging. Goggles and sunglasses also help reduce the risk of cataracts later in life.
However, the sun is a good source of Vitamin D. Recent studies show that people may be developing Vitamin D deficiency due to over protection from the sun. For those concerned about overprotection from both UVA and UVB rays and becoming Vitamin D deficient, Dr. Stampien, suggests using Vitamin D supplements of 600-1000 IU. He feels that this provides adequate levels of Vitamin D to maintain healthy bones and muscles and may lower the risk of certain cancers.
The longer you soak in water, the more skin oils you lose. Therefore, in the winter it is wise to limit baths and showers to 5 minutes or less and use tepid water. Avoid very hot water. Also, only wash your face once or twice a day in the winter. Cool water wiping without soap is recommended if washing your face more than once per day.
Keep your house temperature at 68-70 degrees and use a portable humidifier with 40-50% humidity levels in rooms that you spend a lot of time in such as the kitchen, TV and bedroom.
Natural fibers such as cotton and silk are skin-friendly. However, DryTech products like those made by Nike and UnderArmor wick sweat away and prevent chaffing when participating in outdoor activities.
As with all matters of health and wellness, a diet rich in vegetables, fruits, grains, seeds, and nuts is essential. Additionally, certain foods such as avocados offer niacin, an inflammation-reducing agent which can improve complexion. Yellow and orange produce such as carrots, cantaloupes and apricots are also recommended. Keep in mind that alcohol and caffeine are diuretics that can cause the body and skin to lose fluid and nutrients. Stay hydrated.
Smoking causes vasoconstriction of the blood vessels which limits blood flow of oxygen and nutrients to the skin and other tissues. Daily exercise to improve circulation and adequate sleep to replenish and recharge you body, contribute to health and wellness.
Low humidity and cold temperatures can lead to skin breakdown and cause dry, scaly and uncomfortable feet. Coat your feet generously with lotion and sleep with cotton socks to maintain moisture. Remember, dry and cracked skin can allow bacterial, fungal and viral infections to enter the body.
Skin conditions are often a symptom of a much more serious underlying medical problem. For example, problems with the thyroid, liver, or kidney or cancer can be associated with skin ailments. If problems persist, seek medical attention.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM
For all of Dr. Mackarey's articles visit: Mackarey's Health and Exercise Forum
Tomorrow is Valentine’s Day! And, while you may wonder what that has to do with health and wellness, you might be surprised to learn that love can be good for your health! Studies show that it is in our DNA to seek out good relationships and that these solid relationships can lead to a happier, safer and healthier life. Conversely, infatuation and less committed, volatile relationships that are “on and off,” are very stressful and unhealthy. But those fortunate to participate in a stable and satisfying long-term relationship are the beneficiaries of many health benefits! Whether you have spouse, partner, or close friend, (love is love is love), feeling connected, respected, valued, and loved is critically important to your health and wellness!
The US Department of Human Services found that couples in a committed long-term relationship are less likely to require sick visits to their physician. And, when hospitalized, these “love birds,” have shorter hospital stays. One theory for this health benefit is that couples in good relationships watch after each other to ensure regular healthy visits for routine care and testing. Consequently, they are less likely to have unexpected serious illnesses.
Experts feel that social isolation is associated with unhealthy behavior and depression. Happy, loving and committed couples are far less likely to suffer from depression. Furthermore, these couples are less likely to engage in risky and unhealthy behaviors such as excessive drinking and drug abuse.
Researchers have found a strong relationship between marital status and blood pressure. Happily married couples have the lowest, while unhappily married couples have the highest. Happy singles scored somewhere in between. It is also interesting to note that non married committed couples and well-adjusted singles with strong support groups had lower blood pressure.
Studies show that long-term committed couples have far less anxiety than new romance. MRI brain scans found both groups showed high activation in areas of the brain related to romance, but only new couples had activation of the area of the brain associated with anxiety.
A CDC report on pain included a study of more than 127,000 adults and found that married people were less likely to complain of headaches and lower back pain. In fact, one study showed, when a happily married couple held hands, pain thresholds improved and, the happier the marriage, the greater the effect
Similar to the findings on pain, there is a strong link between happy and committed couples and stress management. The support and love from a strong and healthy relationship provides good coping methods to help overcome adversity…job loss, illness etc.
Solid loving relationships can boost your immune system. In fact, researchers at Carnegie Mellon University found that people who exhibit positive emotions are less likely to get sick after exposure to cold or flu viruses.
It may be that a wound from “Cupid’s Arrow” will heal faster when you are in a loving relationship. Researchers at Ohio State University Medical Center gave married couples superficial wounds and followed their healing time. The wounds healed nearly twice as fast in spouses who interacted warmly compared with those who behaved with hostility.
Strong research indicates that married people live longer. Researchers found that people who had never been married were 58% more likely to die than married people. Some reasons purported were mutual financial, emotional and physical support and assistance from children. One common denominator for a short life span is loneliness and those in a healthy relationship may live longer because they feel loved and connected.
A study in the Journal of Family Psychology showed that happiness depends more on the quality of family relationships than on the level of income. So, according to the research, when it comes to a long, happy and healthy life…love is more important than money!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM
For all of Dr. Mackarey's articles visit our "Health and Exercise Forum"
We are more than one month into the New Year and many people are still talking about their health and fitness goals. As you probably know, losing weight and getting fit are the most popular resolutions, however, for many who have not maintained an active lifestyle in years, it is challenging to know where to begin. Moreover, beginning without a good plan can lead to injury and leave you discouraged. For example, those overweight and de-conditioned should not start a walking program to aggressively. Walking at a fast pace and long distance without gradually weaning into it will most likely lead to problems.
There is probably nothing more natural to human beings than walking. Ever since Australopithecus, an early hominin (human ancestor) who evolved in Southern and Eastern Africa between 4 and 2 million years ago, that our ancestors took their first steps as committed bipeds. With free hands, humans advanced in hunting, gathering, making tools etc. while modern man uses walking as, not only a form of locomotion, but also as a form of exercise and fitness. It is natural, easy and free...no equipment or fitness club membership required!
“There’s no question that increasing exercise, even moderately, reduces the risks of many diseases, including coronary heart disease, breast and colon cancer, and Type 2 diabetes,” said Dr. Jennifer Joyce, MD, professor of family medicine at GCSOM. “Research has even shown that you could gain two hours of life for each hour that you exercise regularly.”
According to the American Heart Association, walking as little as 30 minutes a day can provide the following benefits:
Anything is better than nothing! However, for most healthy adults, the Department of Health and Human Services recommends at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous aerobic activity, or an equivalent combination of moderate and vigorous aerobic activity. The guidelines suggest that you spread out this exercise during the course of a week. Also aim to do strength training exercises of all major muscle groups at least two times a week.
As a general goal, aim for at least 30 minutes of physical activity a day. If you can't set aside that much time, try several short sessions of activity throughout the day (3 ten or 2 fifteen minute sessions). Even small amounts of physical activity are helpful, and accumulated activity throughout the day adds up to provide health benefit.
Remember it's OK to start slowly — especially if you haven't been exercising regularly. You might start with five minutes a day the first week, and then increase your time by five minutes each week until you reach at least 30 minutes.
For even more health benefits, aim for at least 60 minutes of physical activity most days of the week. Once you are ready for a challenge, add hills, increase speed and distance.
Keeping a record of how many steps you take, the distance you walk and how long it takes can help you see where you started from and serve as a source of inspiration. Record these numbers in a walking journal or log them in a spreadsheet or a physical activity app. Another option is to use an electronic device such as a smart watch, pedometer or fitness tracker to calculate steps and distance.
Make walking part of your daily routine. Pick a time that works best for you. Some prefer early morning, others lunchtime or after work. Enter it in your smart phone with a reminder and get to it!
Studies show that compliance with an exercise program is significantly improved when an exercise buddy is part of the equation. It is hard to let someone down or break plans when you commit to someone. Keep in mind that your exercise buddy can also include your dog!
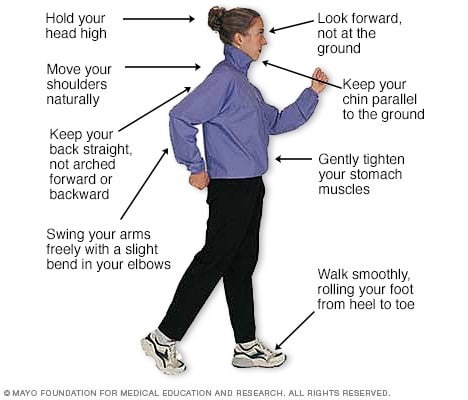
Like everything, there is a right way of doing something, even walking. For efficiency and safety, walking with proper stride is important. A fitness stride requires good posture and purposeful movements. Ideally, here's how you'll look when you're walking:
Sources : Sapiens.org; WebMD; Mayo Clinic
* Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine.
For all of Dr. Mackarey's articles: Visit our Healthcare Forum!
For those trying to lose weight or “get in shape” for the New Year (number one resolution), a better understanding of the role sugar plays in your diet and overall health may be valuable. You have probably noticed a lot of attention being paid to sugar lately. Many television stars, like Ellen DeGeneres, have shared their experiences using a “sugar cleanse” when they need to lose a few pounds and get healthier. I have had several patients and friends tell me the same thing.
For 4-6 weeks these people decide to avoid all refined sugars with the goal of losing weight and improving their health and wellness. Well, what is all the fuss about? Terms like simple sugars and simple carbs, which are purported to be bad, and complex carbs, suggested to be good, are being used ad nauseam. While medical research does not support the value of a short term “sugar cleanse,” it may have value for another reason. For example, it would be very beneficial if one engages in a “sugar cleanse” for the purpose of changing their palate with the hope of developing long term healthy eating habits, especially for those with diabetes.
So, with this in mind, I decided to find the answers to some simple questions about the fuss over sugar. What is a simple sugar? What is a complex sugar? Which sugars are good for you?
Sugars, along with starches and fibers, are one of three types of carbohydrates (also referred to as a carb). A carb is “simple” or “complex,” based on its chemical composition and how it is processed in the body. It gets a little complicated because some foods have both simple and complex carbs. Typically, simple carbs are chemically more “simple” and basic, and therefore they are broken down more easily and serve as a quick source of energy. Some of these carbs are naturally simple (like fruit and milk) while others are processed or refined sugars such as those used in candy, soda and baked goods.
To determine if a food product has good or bad simple sugar, you must also know how much fiber, vitamins and minerals are in the food. A food with a higher sugar content combined with a low fiber, vitamin or mineral content will be worse than a food with the same sugar content but high fiber and vitamins or minerals. For example: a candy bar, which is high in sugar without fiber or vitamins or minerals, is not as healthy as a fresh orange, which contains fiber, vitamins and minerals along with its simple sugar (fructose).
Examples of simple carbs:
Complex carbs have a more complicated chemical makeup and take more time for the body to break down for use as energy. Therefore, these are considered “good” carbs because they provide a more even distribution of energy for the body to use during activity. They cause a more consistent and gradual release of sugar into the blood stream (as opposed to peaks and valleys caused by simple carbs) and provide energy to function throughout the day. Additionally, “good” carbs have the added benefit of providing vitamins, fiber, and minerals that are missing from simple carbs.
Examples of complex (carbs):
Remember that carbohydrates fuel the body and are an important source of energy, especially for active and athletic people. However, carefully selecting the type of carb you eat is critical to peak function and performance.
Sources: www.everydayhealth.com; www.yourdictionary.com; Mayo Clinic
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine.
For All of Dr. Mackarey's articles: visit our healthcare forum!
The beginning of a “New Year” is often associated with renewal and a fresh start to improve ourselves in many ways: financially, socially, mentally, physically and spiritually. Self-help books are best sellers, fitness centers are crowded and weight loss programs are full of well-intenders this time of year. But one relatively novel New Year’s resolution has also gained tremendous popularity. “DRY JANUARY!”
Dry January first began as a public health campaign in 2013 by the U.K. nonprofit, Alcohol for Change, with 4,000 participants. Almost 10 years later, the challenge has become a cultural lexicon as nearly 20% of adults in the U.S. plan to participate. As it turns out, the self-imposed detox has multiple benefits…including saving money! Even though it is January 23rd, it is not to late to start…dry February!
According to the CDC, one drink per day is considered moderate drinking for women and two per day for men. But some studies have found that excessive drinking has increased by 21% during the COVID-19 pandemic. While everyone participating in Dry January will benefit, those exceeding the moderate amount will notice the most significant positive changes. According to a 2019 study from the University of Sussex, more than 80% of Dry January participants felt substantial physical and cognitive improvements and describe being in “more control.”
It is important to remember, while complete abstinence is the principle goal, any reduction of consumption is also productive and valuable.
Full Disclosure: I am personally participating in Dry January and can attest to its value and benefit! And, even if you are not “going dry” this January, you can participate by offering strong support for those who do!
The number one resolution each year is to lose weight. Dry January can help attain that goal. A glass of regular beer has about 150 calories, and a serving of wine has about 120 (5 oz.) and 200 (8oz). These calories do not have high nutritional value and, moreover, can stimulate your appetite. Drinking can make you more impulsive with less discipline to resist the cheese fries and lava cake. Controlling alcohol consumption will also contribute to weight loss.
While a glass of red wine with dinner may have some health benefits, overconsumption may have the opposite effect. For those consuming more than one drink per day, giving up or cutting back on alcohol may lower blood pressure and triglyceride levels. For those with atrial fibrillation, studies found that even one single drink per day was linked to a 16% increase in developing the abnormal heart rhythm compared to non drinkers.
For those with or at risk for high blood pressure, abstaining or reducing alcohol intake can reduce your blood pressure. Normal blood pressure is below 120/80. You have high blood pressure if yours is above 130/80. Talk to your physician.
For those with or at risk for liver disease, abstaining or reducing alcohol intake is critical. Toxins in your body are filtered by the liver and alcohol is toxic to your cells. Heavy drinking (15 drinks for men and 8 for women per week) will eventually lead to liver problems such as fatty liver, cirrhosis and other problems. Keep in mind that all is not lost… your liver can repair itself and even regenerate. So, abstaining or reducing is beneficial.
Some studies show that heavy drinking is associated with certain cancers, including esophagus, mouth, throat, and breast. While it is less clear if abstinence lowers the risk, most physicians would recommend it if you are at risk or diagnosed with the disease.
There is a very strong relationship between alcohol dependence and cognitive function, especially memory. Studies show that prolonged abuse can affect perception of distances, impair motor skills and feel or read emotions. The good news: the brain can heal and regain some of these abilities.
While a drink or two may allow you to relax and fall asleep, it will also make you wake up repeatedly during the night. Alcohol interrupts your REM or deep stage of sleep. It also affects your breathing, especially if you suffer from sleep apnea. Additionally, consumption may increase the need to get up more often to urinate.
Some studies show that even moderate drinking may weaken your body’s immune system for 24 hours. For those consuming large amounts of alcohol over time, the immune system and the body’s ability to repair itself is compromised. Abstinence or reduction may help you keep illnesses at bay.
There is a strong relationship between alcohol use and traumatic injuries and death. Studies show that alcohol plays a role in at least 50% of all serious trauma injuries and deaths from burns, drowning, and homicides. It’s also involved in four out of 10 fatal falls and traffic crashes, as well as suicides. It was found that reducing your drinking by a third can lower the number of injuries and sick days.
For most, social use of alcohol is healthy and allows us to relax with friends and family and compliment a good meal. However, for those who regularly drink alone, or down multiple drinks a day, it could turn into an unhealthy habit. And, for those who can’t control usage, it may lead to a condition called alcohol use disorder. This disorder is associated with depression, anxiety and low self-esteem. Abstinence or reduction may allow you to focus on relationships, work, and health.
While drinking may “put you in the mood,” it may also negatively affect performance, especially for those who over consume. For men, overconsumption is associated with erectile dysfunction and women often notice a loss of sexual interest and vaginal dryness. Less time at the bar may lead to more time in bed!
Warning: Dry January can be difficult for those suffering from prolonged alcohol abuse. Heavy drinkers may experience physical and emotional symptoms of withdrawal and should consult their physician. Some symptoms include: cold sweats, racing pulse, nausea, vomiting, shaky hands, and intense anxiety. In extreme cases, some may experience seizures or hallucinations. Your doctor or substance abuse therapist can offer guidance and may prescribe medication like benzodiazepines or carbamazepine to help you get through it.
Sources: WebMD, Cleveland Clinic

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!”
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine.
For all of Dr. Mackarey's articles: visit our healthcare forum!
There is a very good chance that the cold temps and snow will return soon! Winter in NEPA can be the perfect opportunity to try something new. For example, for those who enjoy running or walking you can continue to do so in the winter, with a few adjustments. Equipment, such as treaded sneakers, allows you to run or walk in the snow. Snow shoes are a great way to hike and walk in the snow while cross country skiing simulates running in the snow. But, in the last few years, another outdoor activity has become a winter sport; mountain biking in the snow has become popular.
Many mountain biking enthusiasts in NEPA enjoy 7-8 months of trail riding at our beautiful state parks. Now, with a few modifications, mountain bikers can continue year round. In fact, the adventure in the snow may be an exciting new experience. If winter biking is not your thing, maybe winter walking, running, snow shoeing or cross-country skiing will suit you better.
The physical and psychological benefits of outdoor activities are many: each season brings its own unique beauty, and winter is no different. Most will not have to abandon outdoor activities, but some adjustments in equipment, clothing, and food are necessary for each season and the temperature changes that it brings.
While recommended, it is not necessary to purchase a bike specifically for mountain biking in the snow. With a few simple modifications and adjustments, you can prepare a regular mountain bike for winter use.
In addition to rocks and stumps, winter biking offers the challenges of snow banks and ice chunks. The air pressure in your shock system will be affected by temperature. Additional air pressure will be required to improve shock absorption and in extreme cases, using less viscous oil will be required.
Pressure - lower the air pressure in the tires 5-10 psi lower than normally used in the summer to improve traction.
Treads – Just as with winter car tires, a larger tire with more volume and large, widely space knobs will improve traction. Some special winter tires offer studs for improved performance on the ice.
Disc Brakes – that are self-cleaning and mounted away from the snow are best for winter biking. However, brakes should be examined and cleaned intermittently for snow and ice accumulation.
Platform Pedals – allow the rider to quickly plant the foot for balance when sliding.
It is important to layer clothing. Use DryTech or UnderArmor type materials (headgear, gloves, shirts and pants) to allow sweat to breath away from the skin to the next layer of clothing. Use a facemask to cover your mouth and nose to prevent frost bite and warm air before it enters the lungs. Chemical hand and toe warmers are great. Try winter running or walking shoes as described below.
There are running shoes specifically designed for use in wet, cold and sloppy winter conditions. These “winterized” running shoes, which can also be used for walking, offer waterproofing, sealed seams, gaiter collars to keep out snow and slop, slip resistant fabric, anti-roll stability features, anti-microbal material and aggressive tread patterns for traction on slippery surfaces. Some shoe recommendations for both winter walkers and runners include:
. Some shoe recommendations for winter runners and walkers from The Runner’s World Magazine include:
For winter walkers, walking or trekking poles will improve balance and safety when briskly walking in winter conditions. I am a strong proponent of using these tools. They are lightweight, adjustable, and collapsible. Some examples are: Black DiamondR Trail Explorer 3 Trekking Poles - $59.99 andMountainsmithR FX Lite Trekking Poles - $35.09. For an inexpensive alternative, an old pair of ski poles will work just fine.
These activities should also be considered as a viable option for the winter walker and runner. These are great cross-training alternatives with tremendous aerobic benefits.
Snowshoes work by distributing your weight over a larger surface area so your foot does not sink completely into the snow. Commonly used by fur traders, trappers and forest rangers, snow shoeing has become very popular among many outdoor exercise enthusiasts. It is relatively safe and inexpensive. Some snowshoes include the Tubbs Flex TRK - $169. (REI) and Redfeather Hike - $149.00 (Cabelas).Boots and poles are also required, but ski or trekking poles along with hiking boots or winter running shoes can be used.
Cross country skiing has also gained tremendous popularity among winter outdoor exercise enthusiasts. It is a cross between running and skiing in which the participant propels through a snow-covered trail by pushing and gliding with a running or fast-walking motion. Some examples of equipment packages that include boots, pole, bindings and skis are Alpina Sports Tour – no wax for $229.00 and Rossignol XT from LL Bean at $224.00.
Many of the area’s state parks, such as Lackawanna and Promised Land, offer wonderful trails for winter walking, hiking, running, snow shoeing, cross-country skiing and biking.
For the more casual walker in need of protection from the snow and ice, it may be treacherous just to walk the dog or go to the bank, post-office or grocery store. Consider traction devices that easily slip on and off your shoes or boots such as StabilicersR (cleats-type device) or YaktraxR (chain-type device).
Visit your doctor regularly and listen to your body.

NEXT MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum” every Monday.
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles: visit our healthcare forum
Osteoarthritis, the most common type of arthritis, is often considered to be a normal part of aging. Usually by the age of forty our joints, especially those which are weight bearing (lower spine, hips, knees, ankles, feet) begin to show signs of wear and tear. The cartilage begins to thin, joint surfaces are not as smooth, and fluid which lubricates the joint becomes diluted, dehydrated and less protective. Consequently, these aging joints become stiff, sore, weak, and sometimes swollen.
Most people with osteoarthritis report additional pain and stiffness in the winter and early spring due to cold, damp weather and NEPA has plenty of it! The cold, for example, restricts the flow of blood to the joints, leading to more pain and stiffness. While moving to a warmer and less humid climate is one solution, it is not practical for most. But all is not lost because there are other alternatives to protect and keep your joints healthier this winter and early spring.
A paraffin bath is one of the best methods to apply heat to your hands and feet to ease pain and stiffness associated with osteoarthritis. A special heating unit works like a crock pot to melt the wax to liquid form. The hands and/or feet are dipped into the wax several times to create a warm coating around the entire area. A 20 to 30 minute treatment while watching TV or listening to good music will provide pain relief, improve mobility in the joints and bring life back to winter damaged skin. $39.99 to $159.99 (www.bedbathandbeyond.com).
Hot packs, electric and microwavable, offer heat to bring blood flow and lessen joint pain and stiffness. They are great for neck and lower back pain, depending on the shape of the pad. Consider rectangle for lower back and cylinder/round to wrap around neck and joints of arms and legs. SourceMed.com offers an electric pad which creates moist heat for $59.95 and a microwave “bed buddy” (herbal or nonherbal) can be found for $9.99 to $43.95 at TheWarmingStore.
Hand and toe warmers are small packets placed in the gloves or boots of skiers, campers and hikers to keep the hands and feet warm. These throw away warmers can also be used by anyone with cold hands or feet whether you are shoveling snow, attending an outdoor event in the cold or sitting in a cold, drafty room watching TV. (Walmart, Dick’s, www.amazon.com)
Supportive sleeves for the joints can provide protection and warmth year round, but especially during the cold winter and early spring. Those made with neoprene material offer warmth and compression and can be valuable when participating in activities such as skiing, walking, running, basketball name a few. Additionally, it can be helpful for those having joint pain with daily activities such as grocery shopping or house work. These devices should not be used when sitting for prolonged periods of time or sleeping. There is no scientific evidence that supports the use of cooper or magnets weaved into the sleeves for additional pain relief. (available at most pharmacies and medical equipment stores)
Similar to neoprene sleeves, compression shorts, pants and shirts can be invaluable to those participating in outdoor activities in cold temps. UnderArmor, Reebok, Nike, and others make these products which can also be worn indoors for those working in cool, drafty environments.
It seems obvious how and why hot water and massaging water jets can soothe the sore joints and muscles. To ensure additional pain and stress relief, add a candle, soft music and a cocktail!
If you suffer from osteoarthritis to the joints of your lower body, you would be well-advised to limit impact activities such as running and basketball. Instead, walk, swim, use the elliptical and bike to protect your joints.
As above, if you have arthritis in the joints of the upper body, use low weights, avoid push-ups and dips, which transfer your body weight through the arms.
As many of you know, I love outdoor activities year round. However, with age I have become a little more sensitive to the cold…which can be a problem when you are skiing, skating, snowshoeing, or hiking. Fortunately, technology has made it possible to be “warm in the cold!” I love my heated vest because it not only keeps me warm, but I require less layers and less bulk to be toasty. These products come with a rechargeable battery. Heated gloves are also available. Vests and jackets range in price from $60.00 to $200.00 but you don’t have to by the most expensive to get a good result. Visit www.ororowwear.com; www.ihoodwarm.com; www.amazon.com
These over-the-counter, non prescription drugs include aspirin and ibuprofen (Advil, Motrin) which are very effective in the treatment of the pain and inflammation associated with arthritis. A topical NSAID, Voltaren, is also available over-the-counter. However, like all drugs, they are not without their risks so one must consult with their primary care physician and pharmacist before using them. For example, NSAIDs can thin the blood, irritate the stomach and may interact with other medications.
Topical analgesics or pain relievers can be rubbed into or sprayed on the skin over the affected area. Some products are counterirritants using menthol, methylsalicylate and camphor which provide a sensation on the skin other than pain. Salicylate based products can work like aspirin to provide relieve from mild pain and inflammation. Capsaicin based products can also provide temporary relief due to the counter stimulation of warmth and tingling. A few things to keep in mind when using these products: one, discuss it with your physician or pharmacist. Two, topical agents are more effective in superficial joints such as the fingers, toes, wrist, elbow, knee and shoulder than in the deep tissues of the hip, buttocks, or lower back. Three, wash your skin thoroughly ater using these products and before using heat, cold or electric stimulation.
The therapeutic benefits of massage are well documented. However, like most treatments, it is important to find a qualified professional that meets your needs. Licensed physical therapists, physical therapist assistants and massage therapists are the best choice. Benefits include; relief from pain, headaches, muscle spasm, and stress, improved relaxation, posture, and breathing.

This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles visit our Health and Exercise Forum