New Year’s Resolutions are very predictable. While most New Year Resolutions are health oriented, I purport that a healthy mind, body and spirit requires a healthy lifestyle. Interestingly, the ten most popular resolutions listed below, all have an impact on a healthy life.
SOURCE: A. Powell, About.com Guide

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's articles, visit our exercise forum!
Happy Holidays! It is at this time of year that we celebrate life with great hope and faith. People of many faiths take time to reflect, respect, and resolve. Christians celebrate Christmas, the miraculous birth of Christ, the Son of God, and the Messiah. Jews celebrate Chanukah, the miraculous festival of lights, when one night’s oil provided enough light and safety for 8 nights. Both major faiths promote healthy lifestyles for the mind, body and spirit. These faiths are grounded in hope, faith, love and peace. It is no surprise that studies repeatedly demonstrate that faithful and spiritual people live longer and healthier lives! At this turbulent time in the world, it is important to note that people of all faiths benefited equally!
With this in mind, I purport, that to be truly healthy, one must have faith because complete health is multidimensional. Socrates preached this message to his students thousands of years before Christ. One must have a healthy mind, which requires intellectual stimulation with attainable goals related to education and intellect. One must have a healthy body by eating well, engaging in physical activity and have attainable goals related to his/her body. Likewise, one must have a healthy spirit with faith, hope, prayer and meditation, comrades and counsel, and set attainable spiritual goals.
How being religious or spiritual has been shown to benefit your mind, body and spirit.
High blood pressure (hypertension) can lead to heart disease and stroke, which are the leading causes of death in the United States, according to the Centers of Disease Control (CDC). It affects 1 in every 3 adults and only half of these people have their blood pressure under control. Well, religion and spiritually may help …
The health benefits of religion or spirituality are well documented. One study conducted at Duke University Medical Center on 4,000 subjects, older adults who described themselves as religiously active were 40% less likely to have high blood pressure when compared to those less active. Moreover, they were surprised to find that those who described themselves as spiritual rather than religious also were less likely to develop high blood pressure.
Research also indicates that religious people are more satisfied with their lives than those without faith. A sociology study determined that high satisfaction among church goers may be due to the strong social bonds that are developed within a religious congregation. Regular church attendees see the same people weekly and often more often, when participating in rewarding and gratifying church-related volunteer work.
In an impressive study published in the Journal of the American Medical Association, researchers interviewed 345 late-stage cancer patients to assess their spirituality as it related to their illness. 88% stated that they were religious as it related to their coping mechanisms. It was determined that those using religion for coping demonstrated a 7.4% rate of resuscitation as compared to 1.8% for those not using religion as a coping mechanism.
According to a Duke University study of 1,718 older adult participants, those described as “highly spiritual” were 50% less likely to have high levels of anti-inflammatory proteins that weaken the immune system and have been linked to some cancers, viral infections and autoimmune diseases. The outcome was similar for those who attend religious services at least once a week.
Those who attend religious services more than once per week are found to live and additional 7 years when compared to those who never attend services. Again, researchers feel that the social benefits of a belonging to a strong religious community may be a large part of the associated longevity. Additionally, the lifestyle of religious people is often healthier: members of these communities rarely engage in risky and unhealthy behaviors such as smoking, excessive drinking, indiscriminate, unprotected sex, etc.
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice in Scranton and Clarks Summit and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's articles, visit our exercise forum!
Every December, as we finish the last of the leftover turkey, patients begin to talk about the holiday season and gift shopping. This conversation invariably leads to suggestions for gift ideas related to health, exercise and fitness. The suggestions below offer a wide variety of fitness related gifts, some expensive and frivolous and others reasonably priced and practical. I hope it makes your shopping a little easier.
Dry Tech is the best thing that has happened to exercise apparel since “jogging suit” was donned by all the “cool dudes” in the 70’s and 80’s . It is has great style and even better function. The specially made material is light weight and breathable and wicks moisture from the skin to the outer layers. Therefore, it will not get heavy with sweat which can weigh you down and cause friction with your skin which can lead to chaffing and blisters. The following exercise apparel is now available in Dry Tech:
NOTE: Shoes are a very important aspect to safe and comfortable exercise but are unique for running and other specific sports (tennis, basketball). Sneakers may be too difficult to buy for someone else. A gift certificate to an athletic shoe store (Scranton Running or Dick’s) may be a better choice.
For walking and hiking enthusiasts, trekking poles can be the perfect gift, especially for those over 50 and when on uneven terrain or inclement weather. The research is compelling…less stress on the lower back, hip, knee and ankle, as well as improved balance and safety. Leki, Black Diamond, and Trekology are good name brands while LL Bean and REI are reputable companies.
An exercise mat is helpful if you decide to exercise at home. Also, a required equipment for participating in yoga or Pilates classes is a mat.
These are essential for those interested in home exercise. For the average beginner, 3-5-8-10 pound (two of each) weights will be adequate. Dumbbells are good for shrugs, biceps, and triceps, bent over rows and lats, and lunges. Incremented and stackable dumbbells are also available by Bowflex SelecTech 552 (5-52 pounds for $299). and NordicTrack $189. Sandbags, which can be purchased as graduated weights from 1 to 5 pounds, are good for leg extensions, hamstring curls, hip hikes and hip abduction.
These cheap and versatile bands are also essential for a home program. The bands come in different colors to represent the amount of resistance with yellow being the easiest and black the most difficult. They are useful for upper and lower body. For specific band exercises visit a previous column in “Health & Exercise Forum” at The Times Tribune or www.mackareyphysicaltherapy.com
NOTE: Peloton, NordicTrack, SoulCycle are some of the companies that offer interactive exercise programs (usually through an internet subscription) for aerobic exercise using bikes, treadmills, ellipticals or rowing machines.
This can be an opportunity for someone to either get the proper advice from a professional to begin a fitness program or to revamp and tune up an old stale program. Word of mouth is a good way to find a reputable certified trainer.
Peloton – ($2,495 bike, $3,495 treadmill); Mirror Exercise – ($1,495); Tonal ($3,995.) FightCamp – ($1,219.); Forme Studio ($2,495.)
These devices use GPS technology to help the user track their activity to get more out of their exercise routines. They monitor activity, heart rate, distance, location, calories, and more. Some examples are:
Sometimes you need professional help to get started and stay focused. Just as with a personal trainer, a qualified and licensed nutritional counselor will assist you in establishing a safe and effective program to meet your nutritional and dietary goals. Again, ask around to see who has a good reputation or who may be a good fit for the recipient of your gift.
These gifts can be purchased at most local sporting goods stores or on-line.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice, located in Scranton and Clarks Summit, and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's articles, check out our exercise forum!
Holiday shopping is stressful for your body, causing backache, as well as your wallet. Even the “online shopper” is at risk when you consider the hours sitting with poor posture on your electronic device. But I do believe that “in person” shopping is worse for backache… driving from store to store, getting in and out of the car while bundled in a sweater and winter coat can add stress to your spine. Often, the expert shopper carries package after package from the store to the car, repeatedly. Six, eight, or ten hours later, the shopper arrives home exhausted with the backache slowly increasing, only to realize that 15 or 20 packages must be carried from the car into the house. This dilemma is compounded by the fact that the rain turned to sleet, and the sleet to snow. You are slipping and sliding all the way from the car to the house while carrying multiple packages of various sizes and shapes, fighting through the already developing backache. The shopping bags get wet and tear, forcing you to tilt your body as you carry the packages. Of course, no one is home to help you unload the car and you make the trip several times alone. You get into the house exhausted and crash onto the couch because your backache is too much to do anymore at this point. You fall asleep slouched and slumped in an overstuffed pillow chair. Hours later you wake up with a stiff neck and lower back pain. You wonder what happened to your neck and back.
Plan Ahead: It is very stressful on your spirit, wallet and back to do all of your shopping in the three weeks available after Thanksgiving. Even though we dislike “rushing” past Thanksgiving to the next holiday, try to begin holiday shopping in before
Use the Internet: Supporting local businesses is important. However, Internet shopping can save you lots of wear and tear. Sometimes, you can even get a gift wrapped.
Gift Certificates: While gift certificates may be impersonal, they are easy, convenient and can also be purchased over the internet.
Perform Stretching Exercises: Stretch intermittently throughout the shopping day…try the three exercises below, gently, slowly, hold 3 seconds and relax, repeat 5 times.



Model: Paul Mackarey, PT, DPT, Clinic Director, Mackarey PT
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at Geisinger Commonwealth School of Medicine. For all of Dr. Mackarey's articles, visit our exercise forum!

As most sports enthusiasts know, Aaron Rodgers, former Green Bay Packer quarterback and recent New York Jets QB (for just over a minute and half) suffered a season ending injury when he tore his Achilles tendon in the first game of the 2023/24 NFL season. Since then, I have been answering many questions from patients and sports fans about the nature of the Achilles Tendon rupture injury, recovery, and how to prevent it.
As the days continue to get shorter and temperatures begin a slow steady decline, athletes and exercise enthusiasts will work harder to warm-up and exercise during the winter months. A little caution and preparation are in order to avoid muscle/tendon strain, or worse yet, muscle/tendon tears, especially Achilles Tendon rupture. The Achilles tendon is one of the more common tendons torn.
This is the second of two columns on Achilles tendon rupture. Last week, I discussed the definition, sign and symptoms of the problem. This week will present examination, treatment and outcomes.
A thorough history and physical exam is the first and best method to assess the extent of the injury and determine accurate diagnosis. While a complete tear is relatively easy to determine, a partial or incomplete tear is less clear. Ultrasound and MRI are valuable tests in these cases. X-rays are not usually used and will not show tendon damage.
Consultation with an orthopedic or podiatric surgeon will determine the best treatment option for you. When conservative measures fail and for tendons completely torn, surgical intervention is usually considered to be the best option with a lower incidence of re-rupture. Surgery involves reattaching the two torn ends. In some instances, a graft using another tendon is required. A cast or walking boot is used post-operatively for 6-8 weeks followed by physical therapy.
Most people return to close to normal activity with proper management. In the competitive athlete or very active individual, surgery offers the best outcome for those with significant or complete tears, to withstand the rigors of sports. Also, an aggressive rehabilitation program will expedite the process and improve the outcome. Walking with full weight on the leg after surgery usually begins at 6 -8 weeks and often requires a heel lift to protect the tendon. Advanced exercises often begin at 12 weeks and running and jumping 5-6 months. While a small bump remains on the tendon at the site of surgery, the tendon is well healed at 6 months and re-injury does not usually occur.
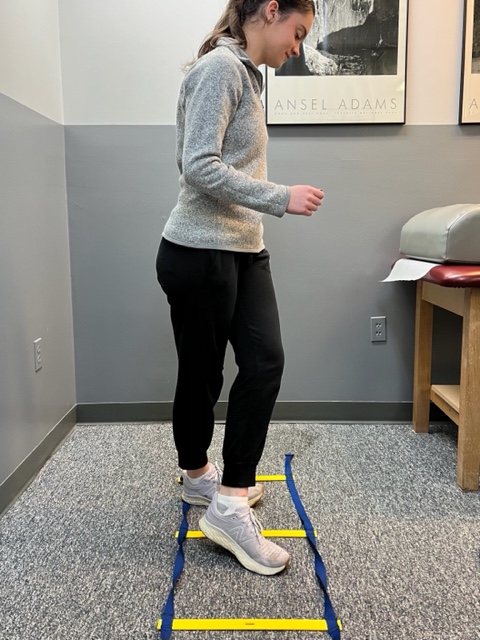
Prevention of muscle and tendon tears is critical for healthy longevity in sports and activities. In addition to the Achilles tendon, the tendons of the quadriceps (knee) and rotator cuff (shoulder) are also vulnerable. A comprehensive prevention program includes: gradual introduction to new activities, good overall conditioning, sport specific training, pre-stretch warm-up, stretch, strengthening, proper shoes, clothing, and equipment for the sport and conditions. Also, utilizing interval training, eccentric exercise (lowering body weight slowly against gravity – Photo 1) and proprioceptive and agility drills are essential (Photos 2 & 3).


In PHOTO 1a & 1b: Eccentric Lowering and Lengthening: for the Achillies tendon during exercise. Beginning on the ball of both feet (1a), bend the strong knee to shift the weight onto the weak leg (1b). Slowly lowering the ankle/heel to the ground over 5-6 seconds. Repeat.
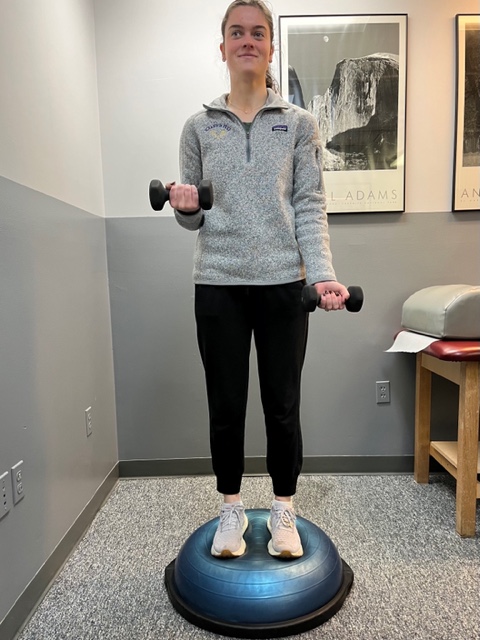
In PHOTO 2: Proprioceptive Training: for the Achillies tendon. Standing on a Bosu Ball while exercising the upper body (for example, biceps curls, shrugs, rows, lats) while maintaining balance on the ball.
PHOTO 3: Agility Drills: for the Achilles tendon involves stepping through a “gait ladder” in various patterns and at various speeds.
MODEL: Kerry McGrath, student physical therapy aide at Mackarey Physical Therapy
Sources: MayoClinic.com;Christopher C Nannini, MD, Northwest Medical Center;Scott H Plantz, MD, Mount Sinai School of Medicine

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's articles, visit our exercise forum!
As most sports enthusiasts know, Aaron Rodgers, former Green Bay Packer quarterback and recent New York Jets QB (for just over a minute and half) suffered a season ending injury when he tore his Achilles tendon in the first game of the 2023/24 NFL season. Since then, I have been answering many questions from many about the nature of the injury and how to prevent it.
As the days continue to get shorter and temperatures begin a slow steady decline, athletes and exercise enthusiasts will work harder to “fit in” a warm-up before running or other activities during the winter months. But, no matter how limited time is, skipping the warm-up is risky. This time of year, one can expect to feel a little cold and stiff, especially if you are over 40, and therefore a little caution and preparation are in order to avoid muscle/tendon strain, or worse yet, muscle/tendon tears. The more commonly torn tendon is the Achilles tendon . Prevention of muscle tears, including the Achilles tendon includes; gradual introduction to new activities, good overall conditioning, sport specific training, pre-stretch warm-up, stretch, strengthening, proper shoes, clothing, and equipment for the sport and conditions.
A muscle contracts to move bones and joints in the body. The tendon is the fibrous tissue that attaches muscle to bone. Great force is transmitted across a tendon which, in the lower body, can be more than 5 times your body weight. Often, a tendon can become inflamed, irritated, strained or partially torn from improper mechanics or overuse. Although infrequent, occasionally tendons can also snap or rupture. A tendon is more vulnerable to a rupture for several reasons such as a history of repeated injections of steroids into a tendon and use of medications such as corticosteroids and some antibiotics. Certain diseases such as gout, arthritis, diabetes or hyperparathyroidism can contribute to tendon tears. Also, age, obesity and gender are significant risk factors as middle-aged, overweight males are more susceptible to tendon tears. Poor conditioning, improper warm-up and cold temperatures may also contribute to the problem.
Tendon rupture is very painful and debilitating and must not be left untreated. While conservative management is preferred, surgical management is usually required for complete tears. The purpose of this column is to present the signs, symptoms and management of Achilles tendon ruptures.
The Achilles tendon (also called the calcaneal tendon), is a large, strong cordlike band of fibrous tissue in the back of the ankle. The tendon (also called the heel cord) connects the powerful calf muscle to the heel bone (also called the calcaneus). When the calf muscle contracts, (as when you walk on the ball of your foot), the Achilles tendon is tightened, tension is created at the heel and the foot points down like pushing a gas pedal or walking on tip of your toes. This motion is essential for activities such as walking, running, and jumping. A partial tear of the tendon would make these activities weak and painful, while a full tear through the tendon would render these activities impossible.
With age, the Achilles tendon (and other tendons) gets weak, thin, and dehydrated, thus making it prone to inflammation, degeneration, partial tear or rupture. The middle-aged weekend warrior is at greatest risk. A full or complete tear (Achilles tendon rupture) usually occurs about 2 inches above the heel bone and is associated with a sudden burst of activity followed by a quick stop or a quick start or change in direction, as in tennis, racquet ball, and basketball.
In some instances, the tendon can be injured by a violent contraction of calf when you push off forcefully at the same time the knee is locked straight as in a sudden sprint. Other times, the tendon is injured when a sudden and unexpected force occurs as in a trip off a curb or sudden step into a hole or a quick attempt to break a fall.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog Next Week: Achilles tendon Part II of II.
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's articles, visit our exercise forum!
The “First Thanksgiving” was in 1621 between the Pilgrims of Plymouth Colony and the Wampanoag tribe in present day Massachusetts to celebrate be grateful for the harvest and other blessings of the previous year. In 1789, President George Washington, at the request of Congress, proclaimed Thursday, November 26, as a day of national thanksgiving. In 1863, Abraham Lincoln proclaimed the national holiday of Thanksgiving to be the last Thursday of November.
Americans and Canadians continue to celebrate this holiday as a time for family and friends to gather, feast, and reflect upon their many blessings. Like most, I am very grateful for the simple things; family, good friends, food, shelter, and health. This year, I am also thankful for the dedicated scientists who developed the COVID 19 vaccination so we can safely enjoy Thanksgiving with our families. It turns out that being grateful is, not only reflective and cleansing; it is also good for your health!
Grateful people are more likely to behave in a prosocial manner, even when it is not reciprocated. A study by the University of Kentucky found those ranking higher on gratitude scales were less likely to retaliate against others, even when others were less kind. Emmons and McCullough conducted one of the most detailed studies on thankfulness. They monitored the happiness of a group of people after they performed the following exercise:
There are many things in our lives, both large and small, that we might be grateful about. Think back over the past week and write down on the lines below up to five things in your life that you are grateful or thankful for.” The study showed that people who are encouraged to think of things they’re grateful for are approximately 10% happier than those who are not.
Amy Morin, psychotherapist, mental health trainer and bestselling author offers this advice: “Developing an “attitude of gratitude” is one of the simplest ways to improve your satisfaction with life. We all have the ability and opportunity to cultivate gratitude. Simply take a few moments to focus on all that you have, rather than complain about all the things you think you deserve.” So…be grateful and have a happy Thanksgiving!
Source: NIH, Forbes, Amy Morin “13 Things Mentally Strong People Don’t Do.”
Visit your doctor regularly and listen to your body.
Keep moving, eat healthy foods, exercise regularly, and live long and well!

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's articles, visit our exercise forum!
According to the American Diabetes Association (ADA) and the Centers for Disease Control (CDC), 11.3% of the population in the United States or almost 37.3 million adults and children has diabetes. Unfortunately, the number keeps rising and one-third of these people are not aware that they have the disease. It will be the purpose of this column to raise the level of consciousness through education and offer recommendations for lowering blood sugar levels naturally.
Perhaps no goal is more important to a person with diabetes than maintaining a healthy blood sugar level. When managed over time, healthy blood sugar levels can slow the onset of complications associated with the disease. According to the ADA, pre-diabetes, or impaired glucose tolerance, occurs when blood glucose levels are higher than normal (110 to 125mg/dl) but below type 2 diabetes levels (126mg/dl). 54 million Americans have pre-diabetes in addition to the 20.8 million with diabetes.
While medications are effective in maintaining blood sugar levels, for those who are borderline, there are effective ways to lower your blood sugar naturally. Your physician will determine which treatment is most appropriate for your problem. Also, maintaining your ideal body weight is always important.
SOURCES: The American Diabetes Association (ADA), CDC, NIH, and Lifescript
Visit your doctor reguLlarly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's articles, visit our exercise forum!
November is National Diabetes Awareness Month. This column will present information regarding type 1 and type 2 diabetes and the diagnosis and symptoms of the disease. Next week, Part II will present the role of exercise in the management of the disease.
What is it?
Diabetes is a disease where the hormone insulin is not adequately produced or used by the body. Insulin is needed for cells to take up glucose after it is broken down from sugars, starches and other food that we eat. When working properly, this provides the fuel necessary for activities of daily living. While the exact cause is not completely understood, genetics is known to play a big role. However, environmental factors such as obesity and inactivity have also been found to play a large role.
According to the American Diabetes Association (ADA) and the Centers for Disease Control (CDC), 11.3% of the population in the United States or almost 37.3 million adults and children has diabetes. Unfortunately, the number keeps rising and one-third of these people are not aware that they have the disease.
A Fasting Plasma Glucose Test (FPG) or an Oral Glucose Tolerance Test (OGTT) can be used to screen a person for diabetes or pre-diabetes. Due to the fact that it is easier, quicker and cheaper, the FPG is the recommended test by the ADA. A FPG test results between 110 and 125 mg/dl indicates pre-diabetes. A FPG of 126 mg/dl or higher indicates diabetes.
Type 1 diabetes occurs when the islet cells of the pancreas are destroyed and unable to produce insulin. Without insulin, the cells of the body are unable to allow glucose (sugar) to enter the cells of the body and fuel them. Without the hormone insulin, the body is unable to convert glucose into energy needed for activities of daily living. According to the ADA, 5-10% of Americans diagnosed with diabetes has type 1. It is usually diagnosed in children and young adults.
While type 1 diabetes is serious, each year more and more people are living long, healthy and happy lives. Some conditions associated with type 1 diabetes are: hyperglycemia, ketoacidosis and celiac disease. Some things you will have to know: information about different types of insulin, different types of blood glucose meters, different types of diagnostic tests, managing your blood glucose, regular eye examinations, and tests to monitor your kidney function, regular vascular and foot exams.
While symptoms may vary for each patient, people with type 1diabetes often have increased thirst and urination, constant hunger, weight loss and extreme tiredness.
Type 1 diabetes increases your risk for other serious problems. Some examples are: heart disease, blindness, nerve damage, amputations and kidney damage. The best way to minimize your risk of complications from type 1diabetes is to take good care of your body. Get regular checkups from your eye doctor for early vision problems, dentist, for early dental problems, podiatrist to prevent foot wounds and ulcers. Exercise regularly, keep your weight down. Do not smoke or drink excessively.
Type 2 is the most common type of diabetes as most Americans are diagnosed with type 2 diabetes. It occurs when the body fails to use insulin properly and eventually it fails to produce an adequate amount of insulin. When sugar, the primary source of energy in the body, is not able to be broken down and transported in the cells for energy, it builds up in the blood. There it can immediately starve cells of energy and cause weakness.
Also, over time it can damage eyes, kidneys, nerves or heart from abnormalities in cholesterol, blood pressure and an increase in clotting of blood vessels. Like type 1, even though the problems with type 2 are scary, most people with type 2 diabetes live long, healthy, and happy lives. While people of all ages and races can get diabetes, some groups are at higher risk for type 2. For example, African Americans, Latinos, Native Americans and Asian Americans/Pacific Islanders and the aged are at greater risk. Conditions and complications are the same as those for type 1 diabetes.
People with type 2 diabetes experience symptoms that are more vague and gradual in onset than with type 1 diabetes. Type 2 symptoms include feeling tired or ill, increased thirst and urination, weight loss, poor vision, frequent infections and slow wound healing.
Sources: NIH; American Diabetes Association; Harvard Health Publications
Visit your doctor regularly and listen to your body.

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM. For all of Dr. Mackarey's articles, visit our exercise forum!
Preventing a fall can not only save your independence but also your life! Preventing injuries from falls reduces the need for nursing home placement. Injuries from falls are the seventh leading cause of death in people over the age of sixty-five.
The following suggestions will assist you in minimizing your risk of a fall:
Following these helpful hints will keep you safe by preventing a loss of balance and a potential fall!
Contributor: Janet M. Caputo, PT, DPT, OCS
Medical Reviewer: Mark Frattali, MD, ENT: Otolaryngology /Head Neck Surgery at Lehigh Valley Health Network

EVERY MONDAY – Read Dr. Paul J. Mackarey “Health & Exercise Forum!” via Blog
EVERY SUNDAY in "The Sunday Times" - Read Dr. Paul J. Mackarey “Health & Exercise Forum!” in hard copy
This article is not intended as a substitute for medical treatment. If you have questions related to your medical condition, please contact your family physician. For further inquires related to this topic email: drpmackarey@msn.com
Paul J. Mackarey PT, DHSc, OCS is a Doctor in Health Sciences specializing in orthopaedic and sports physical therapy. Dr. Mackarey is in private practice and is an associate professor of clinical medicine at GCSOM.
For all of Dr. Mackarey's articles, visit our exercise forum!